13 When is cervical surgery for patients with cervical myelopathy “early/on time,” or “late/too late”? Evidence-based level I–III medical studies were utilized to determine the timing for anterior, posterior, or circumferential cervical surgery (Table 13.1). Variables impacting the timing of cervical surgery included the patient’s age, the number of minor/major comorbidities, the severity/duration of neurological dysfunction and rate of myelopathy progression, and the complexity of the contemplated surgical approach. Cervical procedures had to simultaneously address stenosis (congenital/acquired), disk herniations (soft disks/spurs), degenerative spondyloarthrosis, and ossification of the posterior longitudinal ligament (OPLL), ossification of the yellow ligament (OYL), olisthy/instability, and kyphosis. Postoperatively, the efficacy of surgery could be assessed utilizing the neurological examination in combination with two factors: the extent of canal expansion, and resolution of hyperintense magnetic resonance (MR) cord signals. The increase in the total dimension of the spinal canal measured on axial MR or computed tomographic (CT) views at the prior levels of maximal cord compromise reflected the adequacy of canal decompression. Comparison of preoperative and postoperative T2-weighted MR images revealed whether the preoperatively documented hyperintense cord signal progressed, regressed, or resolved, and reflect whether the preoperative study indicated that reversible edema or irreversible myelomalacia was present; these findings were additionally excellent prognostic signs as to whether surgical timing was respectively early/on time or late/too late. Table 13.1 Evidence Levels of Published Studies
Cervical Myelopathy: Timing of Surgery
Level | Number of Studies | Study Type |
|---|---|---|
I | 3 | |
II | 9 | |
III | 12 | |
|
| |
|
|
 What Is the Natural History for Progressive Cervical Cord Compression?
What Is the Natural History for Progressive Cervical Cord Compression?
Level II
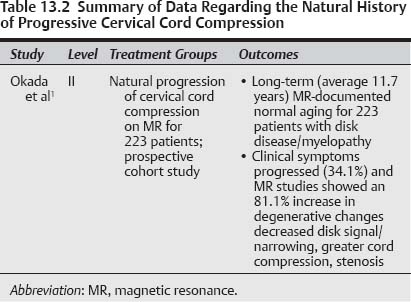
In a level II prospective, long-term (average 11.7 years ± 0.8 years) longitudinal study, the normal aging of the cervical spine was evaluated for patients with documented disk disease and the onset of clinical symptoms/signs of myelopathy (Table 13.2).1 The series involved 223 patients (123 males, 100 females), averaging 39 years of age. Patients were followed (rate of 44.9%) utilizing both (1) MR studies performed at the beginning of the study, and 10 years later, and (2) neurological examinations accompanied by question-naires/surveys. MR-documented pathology focused on the extent of (1) decreased signals in the disk spaces, (2) anterior dural/cord compression, (3) posterior disk protrusions (PDP), (4) disk space narrowing (DSN), and (5) foraminal stenosis (FS). Degenerative changes progressed in 189 patients (81.1%); the signal in the disk decreased (59.6%), anterior dural/cord compression increased (61.4%), PDP increased (70%), DSN increased (26.9%), and FS increased (9%).
Pearls
• Level II data show that patients with cervical disk disease/myelopathy will demonstrate progression of cervical pathology on 10-year follow-up MR studies 81.1% of the time.
• MR findings include decreased signals in disk spaces, anteroposterior cord compression, disk space narrowing, and stenosis.
The latter three MR-documented factors increased disproportionately over the 10-year follow-up interval in the older patients, and correlated with the onset of one or more clinical symptoms in 34.1% of individuals. Notably, no such positive correlations were drawn between the rate of MR-documented progressive degeneration and the sex of the patient, a history of smoking or ethanol abuse, sports played, or body mass index (obesity).
 How Can Patients with Cervical Myelopathy, Cord Compression, and Major Comorbidities Be “Carefully Selected” for Surgical versus Nonsurgical Management?
How Can Patients with Cervical Myelopathy, Cord Compression, and Major Comorbidities Be “Carefully Selected” for Surgical versus Nonsurgical Management?
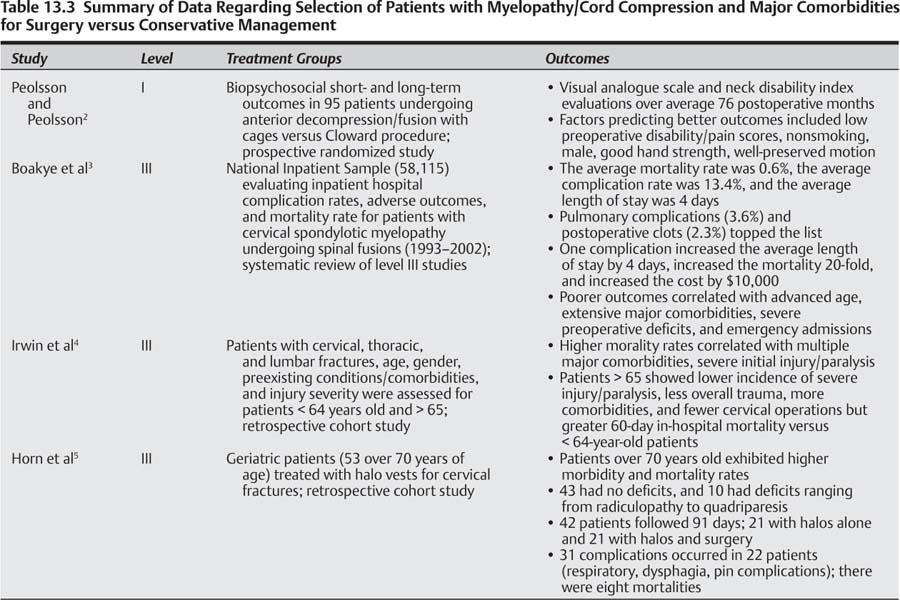
Myelopathic patients with cervical cord compression should undergo stringent preoperative “clinical” screening to determine whether they are viable candidates to undergo surgical intervention (Table 13.3).
Pearls
• Myelopathic patients with significant major comorbidities should be carefully selected for cervical surgical procedures.
• The most common major risk factors include diabetes, hypertension, coronary artery disease/stents/bypasses, peripheral vascular disease, carotid disease, and pulmonary pathology.
• Other major risk factors include immunosuppression [human immunodeficiency virus (HIV), cancer], hepatitis C, psychiatric disease, longstanding chronic pain syndromes, smoking, and ethanol abuse.
• Level I data looking at biopsychosocial elements predictive of short- and long-term outcomes noted better results for those with lower preoperative disability and pain intensity, non-smoking status, males, good hand strength, and well-preserved motion.
• One level III study looking at a national inpatient sample database involving 58,115 patients showed a mortality figure of 0.6% and a complication rate of 13.4% for spinal fusions; they also noted that one complication increased the average length of stay by 4 days and increased the mortality rate 20-fold.
Patients have to be able to “tolerate” the cessation/alteration of multiple medications and deal with medical/surgical stress in the immediate preoperative, intraoperative, and short-/long-term postoperative periods. Multiple clinical factors and minor/major comorbidities may prohibit certain patients from cervical surgery; these typically include advanced age and multiple attendant major comorbidities (diabetes, hypertension, heart diseases/stents/bypasses, peripheral vascular disease, carotid disease, and pulmonary pathology, among others). Older patients with known heart disease should undergo preoperative cardiac stress test screening to ascertain whether they are viable surgical candidates. Others on warfarin for mechanical heart valves, or those on aspirin and/or Plavix (clopidogrel bisulfate; Bristol Myers Squibb, Hopewell, NJ) or warfarin for atrial fibrillation, cardiac disease/stents/bypasses, peripheral vascular disease, stroke/carotid disease, other vasculopathies, and hypercoagulation syndromes among others, may not be medically acceptable for surgical intervention. In many cases, one must not only consider the risks of stopping medications prior to surgery (could switch in some cases to heparin/low molecular weight derivatives and stop within 12 hours of surgery), but also the risks of delayed reintroduction of medications postoperatively. In general, a minimum of 10 days to 2 weeks should pass before reintroducing these medications because, otherwise, there is an increased risk of postoperative hemorrhages/hematomas, wound breakdown, and paralysis.
Additional major risk factors that increase perioperative risks include marked osteoporosis, immunosuppression (AIDS/HIV, cancer), hepatitis (particularly hepatitis C), severe psychiatric illness (depression, panic attacks, psychosis), social factors (secondary gain, compensation, lack of familial support, others), long-standing chronic pain syndromes, prolonged addiction to major narcotics or alcohol, chronic long-term smokers, chronic obstructive pulmonary disease or emphysema, and those with severe-fixed preoperative neurological deficits.
Level I
A prospective, randomized trial looked at biopsychosocial elements correlating with short- and long-term outcomes for patients undergoing anterior cervical decompression and fusion based on visual analogue scales (VAS) and the neck disability index (NDI).2 In this series, 95 patients were randomly assigned to anterior surgery utilizing an intervertebral fusion cage or a Cloward procedure. Patients were followed for a bimodal time period; average 19 months (range 12 to 24 months), and 76 months (56 to 94 months). Factors that reliably predicted better short- and long-term outcomes included preoperative low disability and pain intensities, nonsmoking status, male sex, good hand strength, and well-preserved motion. Preoperative radiographic findings and the specific operative techniques utilized did reliably predict outcomes for either time period.
Level III
Utilizing the National Inpatient Sample, inpatient hospital complication rates, adverse outcomes, and mortality figures were retrospectively assessed for 58,115 patients with cervical spondylotic myelopathy (CSM) undergoing spinal fusion between 1993 and 2002.3 The average mortality figure was 0.6%, the complication rate was 13.4%, and average length of stay (LOS) was 4 days. Pulmonary complications (3.6%) and postoperative clots (2.3%) topped the list for perioperative complications. One complication increased the average LOS by 4 days, increased the mortality rate by 20-fold, and typically cost an additional $10,000. Advanced age, extensive major comorbidities, more severe preoperative neurological deficits, and emergency admissions were the predominant factors contributing to poorer outcomes and increased mortality and complication rates. Those with three or more comorbidities demonstrated a higher risk of medical complications and in-hospital mortality. Patients 85 years or older exhibited a 44-fold increase in mortality rates, compared with patients age 65 to 84 with a lesser 14-fold increase in mortality. Additionally, patients over 84 years of age showed a 40-fold higher frequency of adverse outcomes, and 5-fold greater probability of medication-related complications. Furthermore, more adverse outcomes were observed following posterior fusions (16.4%) versus anterior fusions (11.9%).
In a separate retrospective cohort evaluation of patients with cervical, thoracic, or lumbar spine fractures; age, gender, preexisting conditions/comorbidities, and injury severity were evaluated for adults (16 to 64 years old: 6029) versus geriatric patients (>65 years old; 3973).4 Preinjury patient-related variables, the extent of the injury, the treatment rendered, and the in-hospital versus 60-day mortality figures for the different patient populations were compared. Higher 60-day mortality rates were positively correlated with (1) multiple preexisting medical risk factors/comorbidities and (2) more severe initial injuries/paralysis. However, the 60-day mortality rate was substantially reduced by operative intervention. Although geriatric patients exhibited a lower incidence of severe cervical injury/paralysis, less severe overall trauma, more preexisting comorbidities, and fewer cervical operative procedures, they showed a greater 60-day in-hospital mortality rate compared with younger patients.
In another series, geriatric patients exhibited higher morbidity and mortality rates when treated with halo vest fixation addressing cervical spine injuries.5 Fifty-three patients were identified from a discharge database of patients over the age of 70 who sustained cervical fractures warranting halo fixation; 10 had deficits ranging from radiculopathy to quadriparesis, whereas 43 had no neurological deficits. Of the 42 total patients who were followed an average of 91 days, 21 patients received halo braces alone, whereas 21 had both halo vests and surgery. Thirty-one complications occurred in 22 patients; these included respiratory dysfunction (four patients), dysphagia (six patients), and pin-related complications (10 patients). There were eight mortalities; two were unrelated to the halo device, whereas six died of respiratory failure/cardiovascular collapse (perioperative mortality rate of 14%). Overall, complications associated with the halo devices in geriatric patients (average age 79.9 in this series) largely reflected the severity and number of their underlying comorbidities.
 What Adjunctive Factors Contribute to the Decision to Perform Early/On Time Cervical Surgery?
What Adjunctive Factors Contribute to the Decision to Perform Early/On Time Cervical Surgery?
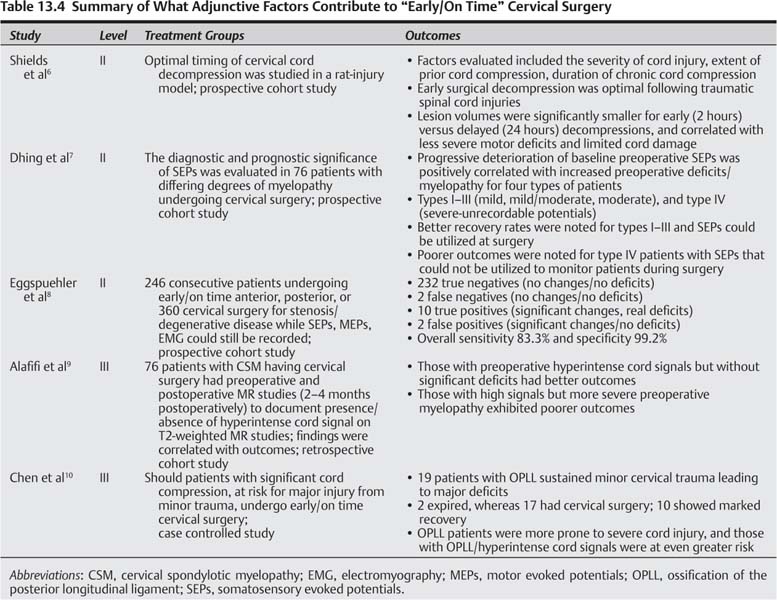
Four major factors contribute to the decision to perform early/on time cervical surgery for patients who experience the onset/progression of myelopathy (Table 13.4).
• Adjunctive factors, which contribute to decisions favoring early/on time cervical surgery, include (1) the attempt to avoid permanent neurological sequelae, (2) response to electrophysiological abnormalities, (3) observation of a hyperintense signal in the cord (edema vs myelomalacia), and (4) severe radiographic cord compression.
• Level II data in a rabbit animal model correlated the optimal timing for surgery in a spinal cord injury model with (1) the severity of cord injury, (2) the extent of prior cord compromise, and (3) the duration of chronic preexisting cord compression; for all three parameters, earlier intervention correlated with improved outcomes.
First, experimental evidence suggests that early surgery averts permanent neurological sequelae. Second, electrophysiological evidence (somatosensory evoked potentials, motor evoked potentials) signals cord compromise and constitutes another set of indicators favoring early/on time surgery.
Pearls
• Abnormal electrophysiological studies, including SEPs, MEPs, and EMG may prompt early/on time surgical intervention in patients with cord compression and myelopathy.
• In level II studies, early surgery correlated with adequately preserved preoperative electrical potentials (SEP, EMG, MEP) and better outcomes, while those with deterioration in potentials/unrecordable potentials demonstrated poorer outcomes.
Third, the initial appearance of hyperintense intrinsic cord signals on T2-weighted MR studies reflect the onset of edema and/or early myelomalacia even in patients minimally symptomatic or with mild myelopathy; those with accompanying significant cord compression; however, may warrant early/on time surgery to avert irretrievable cord injury. Fourth, patients with severe radiographic cord compromise, with/without significant myelopathy, may require early/on time cervical decompression to avoid the risk of severe neurological injury/quadriplegia associated with even minor trauma. In summary, there are multiple “adjunctive” pros favoring early/on time cervical surgery in patients with cervical cord compression and the onset/progression of myelopathy.6–10
What Is the Efficacy of Early versus Late Surgery in a Rabbit Spinal Cord Injury Model?
LEVEL II
The optimal timing for cervical decompression in a rat spinal cord injury model with stenosis-related spinal cord compromise was correlated with three variables: (1) severity of cord injury, (2) the extent of extrinsic preexisting cord compression, and (3) the duration of chronic prior cord compression.6 A mild spinal cord injury model was created in the rabbit, centered at the T10 level. It employed 1.13 mm and 1.24 mm thick spacers to mimic stenosis and produced respective 38% and 43% degrees of stenosis. The extent of cord damage linearly reflected the extent/duration of cord compromise. Early surgical decompression proved to be optimal following traumatic injuries. The lesion volume was significantly smaller for the early (2 hours) versus delayed (24 hours) decompressions, correlated with less severe motor deficits (e.g., animal able to support his or her own weight), and limited cord damage (6 to 12 hours). Notably, the longer preoperative intervals resulted in more irretrievable cord damage, confirmed by the observation of more severe/irreversible motor deficits.
Should Electrophysiological Abnormalities Impact the Choice for Early/On Time versus Late/Too Late Cervical Surgery?
Abnormal electrophysiological studies; somatosensory evoked potentials (SEPs), motor evoked potentials (MEPs), and electromyography (EMG) may prompt early/on time surgical intervention in patients with cervical cord compression experiencing the onset of and/or progression of myelopathy. Delays/abnormalities in SEPs (median, ulnar, or posterior tibial responses), and MEPs signal ongoing cord compromise. Early surgery may, therefore, be warranted for two major reasons. First and foremost, early surgery may prevent the further deterioration of these potentials reflecting the onset of permanent myelopathic deficits and irretrievable neurological injury. Second, once these potentials deteriorate, become unstable, or even become immeasurable, they can no longer be effectively utilized to avert intraoperative neurological catastrophes.
LEVEL II
The diagnostic and prognostic significance of SEPs was evaluated in a prospective cohort study involving 76 patients with differing degrees of preoperative myelopathy undergoing cervical surgery.7 Progressive deterioration of baseline preoperative SEP wave preservation and configuration was positively correlated with increased preoperative neurological deficits/myelopathy. Patients were divided into four types reflecting increasingly impaired SEPs: types I to III (mild, mild/moderate, moderate impairment) with recordable SEPs, compared with type IV (marked impairment: unrecordable potentials), which could no longer be elicited. The number of patients in types I to IV were, respectively, 27 (36%), 30 (39%), 8 (11%), and 11 (14%). The recovery rates from “identifiable” SEPs (types I to III), were greater than for those with “unidentifiable” waves (type IV). They concluded that adequately preserved preoperative SEPs (types I to III) were useful for intraoperative monitoring in patients with mild to moderate myelopathy. Alternatively, unidentifiable SEP recordings (type IV) that correlated with more severe/irreversible preoperative neurological deficits, could not be effectively utilized for intraoperative monitoring and correlated with poorer outcomes.
In another prospective cohort study, 246 consecutive patients having anterior, posterior, or circumferential cervical surgery predominantly attributed to stenosis and degenerative disease, underwent multimodal intraoperative monitoring at a time (early/on time) when all potentials were present/recordable (SEPs, EMG, MEPs were performed).8 The results of intraoperative monitoring revealed that 232 were true negatives (no significant changes/no deficit), two were false negatives (no significant changes/no deficits), 10 were true positives (significant changes/real deficits), and two were false positives (significant changes/no deficits). The overall sensitivity was 83.3%, whereas the specificity was 99.2%. In this study, the performance of early/on time surgery, defined as taking place prior to the deterioration of SEPs and MEPs, allowed patients’ operative procedures to be effectively and safely monitored.
Should Hyperintense Cord Signals on T2-Weighted Magnetic Resonance Images Prompt Early/On Time Surgery for Cervical Myelopathy?
The presence of a hyperintense signal in the cord on pre-operative T2-weighted MR studies should prompt consideration of early/on time surgery for patients with myelopathy attributed to cervical cord compression.
Pearls
• Hyperintense signals within the spinal cord on T2-weighted MR studies indicated the need for early/on time surgery to avoid irreversible or further progression of cord damage.
• In a level III study, those patients with hyperintense cord signals preoperatively but without significant neurological deficits demonstrated the best postoperative outcomes.
• Those with hyperintense signal abnormalities in the cord but with significant myelopathy (Babinski signs, clonus) showed poorer postoperative results.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree