16 | Cerivcal Ostomyelitis |
 | Case Presentation |
History and Physical Examination
A 98-year-old woman presented to the emergency department with complaints of severe neck pain and night sweats. She noted progressive neck pain over the preceding 6 weeks. She denied any history of trauma, drug or alcohol abuse, foreign travel, or immunosuppressive disorders.
Radiological Findings
Her workup included plain radiographs, which showed severe spondylosis and an abnormal appearance of the C5-6 level with collapse of the disk space and destruction of the surrounding end plates (Fig. 16–1). Magnetic resonance imaging (MRI) demonstrated an apparent abscess at the C5-6 level with a perispinal collection and a small epidural component (Fig. 16–2). Laboratory studies demonstrated a mildly elevated white blood count (WBC) (10.5 mg/dL) without a left shift, an elevated erythrocyte sedimentation rate (ESR) (65 mm/h), and an elevated C-reactive protein level (8.5 mg/dL).
Diagnosis
Cervical osteomyelitis and epidural abscess
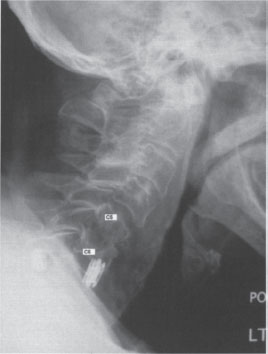
Figure 16–1 This plain radiograph (lateral view) of the cervical spine shows evidence of severe spondylosis and collapse of C5-6 intervertebral disk space with destruction of the adjacent end plates.

Figure 16–2 This T2-weighted sagittal magnetic resonance image shows an abscess at the C5-6 level with a perispinal collection and a small epidural component.
 | Background |
The most common presenting symptom for cervical osteomyelitis is neck pain, followed by fevers. Neurological symptoms or deficit is present in ~20% of cases. Because the symptoms are nonspecific, a delay in diagnosis is common.1 The physical examination often reveals neck tenderness, muscle spasm, and restricted motion. Vital signs may demonstrate fever and tachycardia. A thorough neurological examination of the extremities is indicated to rule out a neurological deficit.
 | Causative Agents |
Spinal infections can be caused by a wide variety of pathogens, including bacteria (pyogenic infection), mycobacteria or fungi (granulomatous infection), and parasites (echinococcosis).2 The most common organism in the Western world is Staphylococcus aureus, which is found in ~60% of cases, followed by Streptococcus species (~20%), and gram-negative bacilli (~14%).3 Infections with Methicillin-resistant Staphylococcus aureus (MRSA) are not uncommon, especially in hospitalized patients.4 In third world nations, tuberculosis remains a common cause of cervical osteomyelitis.
With pyogenic infection, the disk, end plate, and vertebral body are most often affected. Perispinal abscess and epidural infection are common.5 Rarely, Streptococcus agalactiae may be found in postpartum females or newborn infants. This species is notable for causing extensive tissue destruction predisposing to spinal instability and abscess formation. Treatment may require prolonged antibiotic therapy and radical debridement.6 Atypical infections (mycobacteria or fungus) may spare the disk space and cause large anterior perispinal infections while destroying the vertebral bodies.7
 | Incidence and Risk Factors |
The incidence of spine infection has been increasing over the past few decades.8 This is due in part to an increased incidence of intravenous drug abuse and larger numbers of immunosuppressed individuals undergoing treatment for cancer or organ transplantation. Diabetes mellitus, a common risk factor for spinal infection, is also becoming more prevalent.9,10 Cervical osteomyelitis is more common with increasing age (mean age at presentation is 60) and has a slight male predominance (~60% male).11 The cervical spine is affected in almost one third of the cases of pyogenic spinal infection. Spinal epidural abscess accompanies cervical spondylodiskitis in ~90% of cases.12 In Western societies, diabetes mellitus is the most common predisposing factor to pyogenic vertebral osteomyelitis.13 Because hematogenous dissemination is the most common route of spinal inoculation, relative immune compromise is often present.4 Other conditions associated with cervical spinal infections include rheumatoid arthritis, chronic steroid use, acquired immunodeficiency syndrome (AIDS), and cancers.12
 | Laboratory Studies |
WBC is elevated in fewer than half of affected patients. ESR is more sensitive for infection but also nonspecific. C-reactive protein level is generally elevated and may respond more quickly to treatment than the ESR.4,14
Blood cultures generally have a low sensitivity and yield with positive results in only ~25% of cases. Image-guided needle biopsy is much more specific for obtaining a bacteriologic diagnosis and should be considered in cases where open surgical debridement is not planned to ensure that optimal antibiotic therapy is instituted.15
 | Radiological Imaging |
Plain radiographs may show narrowing or loss of the affected disk space and destruction of the vertebral end plates (Fig. 16–1). MRI is the preferred imaging modality for spinal osteomyelitis and has a diagnostic accuracy of over 90%. MRI is noninvasive and provides anatomical localization of the infection and demonstrates the presence of epidural abscess formation or extraspinal extension.16 Bone scintigraphy is sensitive but not specific for osteomyelitis/diskitis and is less frequently used. Computed tomographic (CT) scans may be helpful in defining the degree of bony destruction in cases of osteomyelitis.
 | Authors’ Preferred Method of Surgical Management |
In the described case, due to the presence of the gross infection with an epidural abscess, surgical debridement was recommended. The patient underwent an anterior approach with thorough debridement of the infection and fusion of the C5-6 level with autogenous bone. Specimens were sent for aerobic, anaerobic, acid fast, and fungal cultures. Decompression of the neural elements was achieved. Consideration was given to posterior fusion and stabilization of the cervical spine. However, the graft was felt to be secure and, given the patient’s age, the morbidity of additional surgery was felt to outweigh the added benefits of posterior surgery.
For cervical osteomyelitis, surgical treatment should be considered for patients with disabling pain, significant spinal deformity, sepsis, large perispinal abscesses, epidural abscess formation, neurological symptoms, or severe immunosuppression. The goals of surgery are to adequately debride the infection, obtain material for culture, decompress the neural elements, and reconstruct the spine in a stable fashion to allow a bony fusion to occur.17
Pearls and Pitfalls
The author manages most cases of pyogenic cervical osteomyelitis with anterior surgical debridement. Multiple cultures are taken during the debridement. The neural elements are fully decompressed in cases where spinal epidural abscess is present. Reconstruction of the spine is achieved using autogenous iliac crest bone graft removed prior to the debridement procedure. The iliac crest site is closed fully prior to debridement to prevent contamination of the bone harvest site. Some authors have described the use of cage implants. allograft bone, or anterior plating in the face of a thorough debridement. However, we generally avoid anterior instrumentation or allograft due to the risk of bacterial seeding. If significant destruction of the spine is present, posterior fusion and instrumentation are also performed using a clean operative setup, This provides maximal stability to the spinal segment and enhances healing and resolution of the infection.
Following adequate surgical treatment of a pyogenic cervical infection, fusion is expected in 95 to 100% of patients, and eradication of the infection is achieved in most cases.



