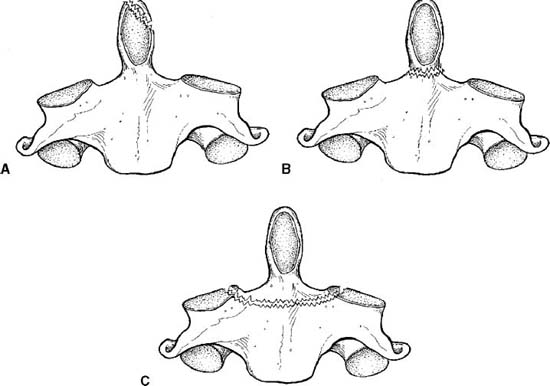
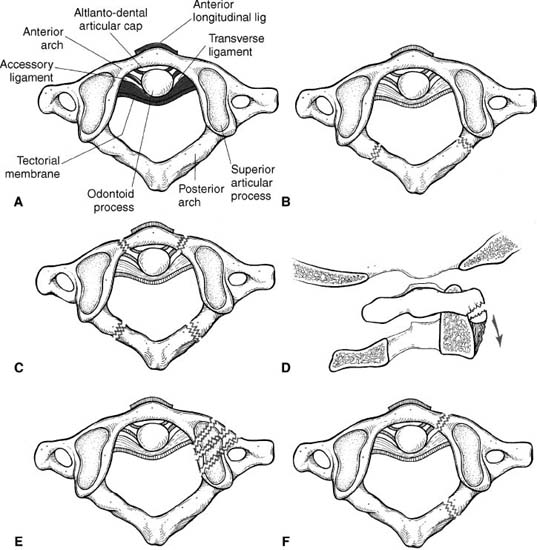
8 I. General considerations A. Fifty thousand cervical spinal column or cord injuries reported yearly in the United States B. Most spinal column or cord injuries occur in males between the ages of 15 and 24. C. Mechanism 1. Motor-vehicle accidents are the most common mechanism (40 to 56%). 2. Falls (20 to 30%) 3. Gunshots (12 to 21%) 4. Sports (6 to 13%) D. Midcervical spine (C4–C6) is most commonly affected anatomic region. II. Patient evaluation A. Detailed history including mechanism of injury as well as associated injuries must be sought. B. Early recognition of the injury begins in the field. 1. Cervical collar and spine board are applied to patient. 2. Transfer to an emergency department a. Trauma resuscitation team evaluates airway competency, breathing, and circulation. 3. Anteroposterior and lateral radiographs of the entire spine are obtained. C. Pharmacological therapy 1. Acute spinal cord injury is treated with administration of high-dose methylprednisolone a. Begin with 30 mg/kg over 15 minutes. b. Then, 5.4 mg/kg for the duration listed below. (1) Less than 3 hours from injury—24-hour duration (2) Three to 8 hours from injury—48-hour duration (3) More than 8 hours from injury—no treatment c. Recent reports question efficacy. Canadian Spine community, for example, no longer advocates its utilization. A. Occipital condyle fractures 1. Rare injury 2. One third occur in conjunction with atlanto-occipital dislocations. 3. Diagnosis most commonly made incidentally with a head computed tomography. a. Ligamentous injury, intracranial hematoma, and neurological deficit may accompany this injury. 4. Treatment a. Usually rigid orthosis or halo vest for 3 months b. Flexion-extension film is obtained at 3 months. c. Occipital-cervical arthrodesis for resultant instability B. Occiput–C1 dislocation 1. Unstable and almost always fatal a. Survivors usually have severe neurological deficits. 2. Violent, twisting, or flexion-extension force on the head 3. Disruption of all ligamentous attachments 4. Radiographic diagnosis a. Harris radiographic lines 5. Treatment a. Closed reduction b. Occipital-cervical fusion C. C1–C2 subluxation 1. More common in children than in adults 2. Common complaints a. Neck pain with evidence of torticollis b. Suboccipital pain c. Limited cervical rotation D. May be associated with odontoid or atlas fractures 1. Rupture of transverse ligament a. Anterior atlantodens interval (1) Three to 5 mm indicate rupture of the transverse ligament. (2) Seven to 8 mm indicate complete ligamentous disruption. (3) Greater than 10 mm causes spinal cord compression. b. Treatment (1) If instability 3 to 5 mm, halo or rigid orthosis is used for 2 to 3 months. (2) If > 5 mm instability, then fuse C1–C2 2. Atlantoaxial rotatory fixation a. The head is tilted toward the side of fixation and the chin and C2 spinous process is pointed toward the opposite direction. E. Fracture of Atlas (C1) (Fig. 8–1) 1. Axial loading disrupts the atlantal ring. 2. Neurological injury is rare because of the wide spinal canal. a. Cranial nerve injuries may be observed. 3. An anteroposterior open-mouth odontoid view to assess the lateral masses of C1 relative to the lateral mass of C2 a. Greater than 6.9-mm widening of lateral mass indicates transverse ligamentous rupture. (1) Allow atlas fractures to heal first with halo immobilization for 2 to 3 months. (2) C1–C2 fusion may be done if instability is greater than 5 mm. 4. Treatment a. Cervical orthosis for 3 months if nondisplaced b. Halo vest for 3 months if displaced or delayed union c. Posterior C1–C2 fusion for nonunion F. Fractures of the odontoid (Fig. 8–2) 1. Type I
Cervical Spine Trauma
Neupsy Key
Fastest Neupsy Insight Engine