Sagittal T2 MRI cervical spine shows a solitary area of increased T2 signal at the prior level of compression, now relieved by spinal decompressive surgery.
Three-step assessment
1 Classical clinical features of MS: none, static non-progressive myelopathy associated with prior compressive trauma
2 Neurological examination: consistent with myelopathy
3 Investigations: brain MRI – non-specific; spinal cord MRI – myelomalacia from old trauma; CSF normal; evoked potentials normal
Diagnosis: Static cervical myelopathy due to old compression but no evidence of progressive multiple sclerosis.
Tip: The only way to identify progressive forms of multiple sclerosis is on history and on examination. This patient had no clear clinical history of progressive myelopathic symptoms over a number of years. She had a static myelopathy entirely related to an old compressive lesion. The areas of abnormal signal on the MRI scan were non-specific and not characteristic of MS. Importantly, other tests looking for evidence of multiple sclerosis were normal, including an MRI scan of the thoracic spine, a CSF examination and evoked potentials.
Case 58: A woman with continued progressive gait impairment after successful cervical fusion surgery
A 52-year-old woman presented with a four-year history of progressive walking impairment. She had become limited to walking only a few blocks. A cervical spine MRI scan showed spondylotic changes. There was no significant pain, but local providers recommended spinal surgery and a cervical spinal fusion was performed two years prior to presentation. Despite the surgery, she continued to have worsened gait impairment over time. She had impaired bladder emptying on ultrasound evaluation. She had a history of type 2 diabetes mellitus, hyperlipidemia and hypertension. There was no family history of multiple sclerosis.
On neurological examination, her mental status, cranial nerve and motor examination in the face and upper extremities were normal. She had severe weakness in a pyramidal distribution on the right lower extremity only. Plantar responses were extensor on the right and equivocal on the left. She walked with a right-sided circumductive upper motor neuron weakness gait. Vibratory sense was minimally reduced in the toes.
A brain MRI showed lesions highly suggestive of MS. Upon reviewing the outside cervical spinal MRI, the initial cervical spondylotic changes did not show an area of abnormal signal at the level of most severe compression (Figure 9.2). There was, however, an area of abnormal T2 signal in the high cervical cord that was clearly separate from the area of spinal cord compression. Additionally, a thoracic spine MRI showed areas of abnormal T2 signal consistent with MS. A CSF examination was undertaken and was found to be normal. She had never had visual evoked potentials.
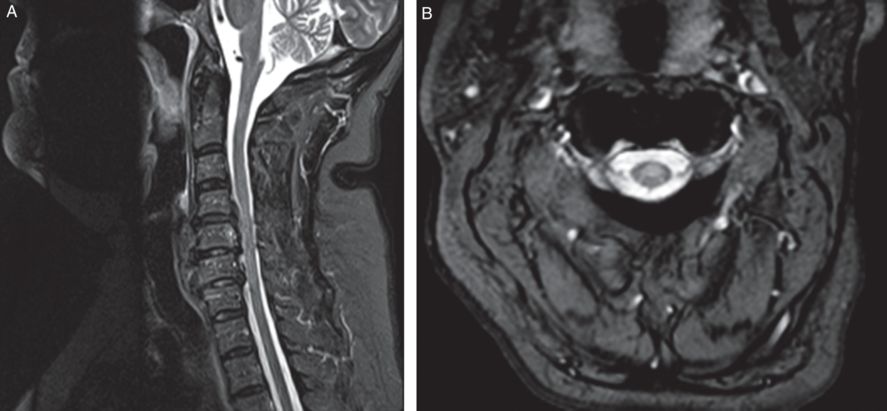
Sagittal and axial T2 MRI cervical spine shows demyelinating lesions within the cord parenchyma at C2 anteriorly, between C5 and C6 laterally and scattered throughout the thoracic cord (not shown) including a lesion within the conus. Postoperative changes of instrumented anterior interbody fusion with plate and screw fixation from the C4-C7 is demonstrated.
Three-step assessment
1 Classical clinical features of MS: progressive myelopathy
2 Neurological examination: consistent with myelopathy
3 Investigations: brain MRI consistent with MS; cervical spinal cord MRI – spondylotic changes but abnormal intramedullary cord lesion separate from compressive area consistent with MS; MRI thoracic spine consistent with MS; CSF normal
Diagnosis: Primary progressive multiple sclerosis.
Tip: Multiple sclerosis MRI spinal cord lesions may be subtle. If there are areas of stenosis due to cervical spondylosis, it should be assured that the most prominent area of intramedullary abnormal T2 signal related to the stenosis should be directly adjacent or immediately rostral to the stenosis. The later MRI scan of the brain showed areas of abnormal signal that were highly suggestive of multiple sclerosis, as did the MRI thoracic spine, which was a compelling finding in the absence of CSF abnormalities of significance such as elevated IgG index or oligoclonal bands in this patient.
The progressive worsening after successful fusion surgery suggested that that was not the original cause for the progressive myelopathy.
Case 59: Progressive hemiparesis in a man with a single cervical spinal cord lesion. Could this be MS?
A 58-year-old gentleman presented with progressive hemiparesis. He had noticed worsening left-sided weakness over the prior three years. He underwent lumbar spinal surgery for possible lumbar stenosis but he had no improvement. He had occasional paresthesias of the left hand and foot but did not have bowel or bladder impairment. When he lay supine he would get extensor spasms of the left lower extremity. He had no prominent fatigue but he required a cane to ambulate.
On examination, his mental status was found to be normal. His cranial nerves were also normal. He had moderate weakness in the left upper and lower extremities in a pyramidal distribution, with the right side being entirely normal. Reflexes were brisker on the left than on the right, and the plantar response was extensor on the left and equivocal on the right. He walked with a left-sided hemiparetic gait. His vibratory sense was impaired at the toes bilaterally.
A brain MRI showed a few areas of abnormal signal that were not highly suggestive of multiple sclerosis. A cervical spine MRI showed evidence of a single area of abnormal signal in the left lateral cord at the C3-C4 level (Figure 9.3). A thoracic spine MRI was normal. A CSF examination showed the protein minimally elevated at 55 mg/dL and with nine unique oligoclonal bands. Serological evaluations were negative including vitamin B12, copper, ceruloplasmin, ANA, paraneoplastic autoantibody screen, HIV, Lyme screen, syphilis screen and very long-chain fatty acids. NMO-IgG antibodies were negative.
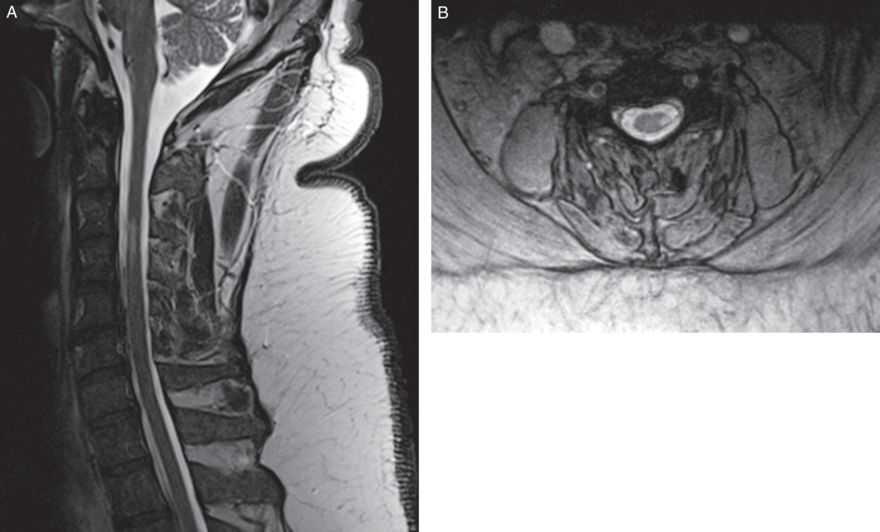
Sagittal and axial T2 MRI cervical spine showed abnormal T2 hyperintensity involving a left lateral aspect of cord at C3–4 level without associated cord expansion. Considerations include focus of demyelination such as related to MS.
Three-step assessment
1 Classical clinical features of MS: progressive myelopathy
2 Neurological examination: consistent with myelopathy
3 Investigations: brain MRI not consistent with MS; cervical spinal cord MRI – single intramedullary cord lesion suggestive of MS; thoracic spinal cord MRI normal; CSF consistent with MS
Diagnosis: Solitary sclerosis presentation of primary progressive multiple sclerosis.
Tip: Patients may have a progressive myelopathy with only a single MRI lesion associated with the characteristic features of demyelination of multiple sclerosis. Progressive impairment may occur bilaterally if the single MRI lesion is large and it may cause quadriparesis when it is located in the cervicomedullary junction.
Case 60: A man with gait impairment after bronchitis. Is it transverse myelitis?
A 76-year-old gentleman was well until four months prior to presentation. He had recovered from a viral upper respiratory tract infection on a trip to Alaska. He noticed, while riding his bike, that whenever he would hit a bump he would get a tingling sensation radiating down both upper extremities. He then developed a walking impairment with significant gait imbalance. The next month, while cutting down trees, he noticed a weakness in the upper extremities proximally and muscle stiffness. He was felt to have rotator cuff tendon disease, and underwent injections and physical therapy. Subsequently he developed tingling sensation of all fingers of both hands with numbness of the left greater than right foot. While he was previously active in the health club, he now could not lift the same amount of weights and he had difficulty even with activities such as tying his shoes, buttoning shirts and opening jars. He had no bowel or bladder incontinence. He noticed an aching sensation and a “tired” sensation in his neck.
He had no prior symptoms of clinical attacks of multiple sclerosis such as optic neuritis, diplopia, hemiparesis or hemisensory deficit in the past. He also had no history of symptoms of inflammatory myelopathy.
On neurological examination it was found that facial and proximal upper extremities power was normal. Weakness was found to be greater in the left than right wrist extensors, finger extensors and all intrinsic hand muscles with normal lower extremity strength. Muscle stretch reflexes were brisk with bilateral, sustained ankle clonus and bilateral extensor plantar responses. He walked with a spastic ataxic gait and could not tandem walk.
A brain MRI was found to be normal. A cervical spine MRI showed evidence of spondylosis, which was described by the local radiologist as only “mild to moderate.” A thoracic spine MRI scan and CSF examination were normal.
He was diagnosed with presumed “transverse myelitis” related to bronchial infection.
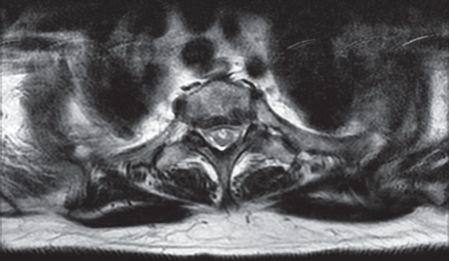
A repeat cervical spine MRI was unchanged; however, the results were now reinterpreted to be evidence of advanced spinal stenosis at C4-C5 and C5-C6 levels with associated non-enhancing T2 hyperintensity within the cord, which are consistent with compressive spondylotic myelopathy (Figure 9.4).

Sagittal T2 MRI cervical spine showing multilevel cervical spinal stenosis, advanced at C4-C5, with associated cord signal at this level compatible with spondylotic myelopathy.
Three-step assessment
1 Classical clinical features of MS: progressive myelopathy
2 Neurological examination: consistent with myelopathy
3 Investigations: MRI brain not consistent with MS; MRI cervical spinal cord consistent with compressive etiology; MRI thoracic spinal cord normal; CSF normal
Diagnosis: Compressive cervical spondylotic myelopathy.
Tip: Progression for more than four weeks is less compatible with inflammatory myelopathy such as transverse myelitis. Exclusion of compressive cervical spondylotic myelopathy is a critical initial step in evaluating and treating patients with myelopathy. This patient underwent immediate cervical spinal decompressive surgery and had marked improvement immediately after.
Case 61: Acute myelopathy while undergoing shoulder surgery. Is it transverse myelitis?
A 72-year-old woman underwent elective rotator cuff surgery. She was recovering from the surgery well and was not on any medications. It was thought that she may have been vaccinated for pneumococcus while hospitalized. Two weeks after the surgery, she awoke with significant chest pain. She was taken by the EMT providers back to the hospital after administering aspirin. Initially, she was discharged after no significant impairment was found. The next evening, she developed severe lower extremity paralysis which manifested in thoracic sensory level and bladder dysfunction with an inability to urinate. She was hospitalized and received three days of intravenous corticosteroids and oral corticosteroids for six days on a decreasing dose with minimal improvement.
She remained with ongoing urinary urgency, hesitancy and rare bowel incontinence. Her motor impairment improved over a number of months. She had no previous symptoms of MS attacks or CNS demyelination in the past and no progressive neurological impairment. She had a history of hypertension, hyperlipidemia and coronary artery disease. There was no family history of MS or other neurological disease. Her diagnosis was of inflammatory transverse myelitis possibly related to vaccination.
On undergoing a neurological examination months later, a motor examination of the face and upper extremities were found to be normal. Reflexes were reduced in the upper extremities, and plantar responses were flexor bilaterally. Her gait was cautious. Vibratory and joint position senses were normal in the hands and feet. There was reduced sensation to pinpricks and temperature that was greater in the left than right leg and the back and abdomen on both sides.
A brain MRI showed small vessel ischemic changes but no changes of demyelination. A cervical spine MRI was normal. A thoracic spinal cord MRI scan showed evidence of abnormal signal at T1 through T3 without gadolinium enhancement. A repeat thoracic spine MRI showed evidence of a focal non-enhancing T2 signal abnormality at the T2 level in the expected location of the anterior spinal artery (Figure 9.5). There were no abnormal flow voids, gadolinium enhancement or other evidence of an arteriovenous fistula. A lumbar spine MRI was normal. A CSF examination was normal, including the white blood cell count, IgG index and oligoclonal bands. West Nile Virus testing and NMO-IgG antibodies were both negative, as were an extensive battery of other viral and inflammatory markers on the serum and CSF. Chest and abdomen CTs were both normal.
Axial T2 MRI thoracic spine shows a focal non-enhancing T2 hyperintensity along the ventral margin of the thoracic spinal cord at the T2 level in the expected location of the anterior spinal artery that is consistent with ischemic myelopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








