Natural History
There is a great variation in the onset, severity, and progression of symptoms. The cardinal symptoms, which include gait disturbance, dementia, and incontinence, all of which do not have to be present together, may actually appear at different times. If symptoms are present, then they will usually progress.3,4 The progression can vary considerably, seeing almost stable courses over many years or severe deteriorations in several months.5 The often slow and uncharacteristic onset of symptoms makes early diagnosis of iNPH difficult. Therefore, it is difficult in many cases to estimate how long the disease has been ongoing. In exceptional cases, spontaneous regression of symptoms may occur.4 Evaluation of the patient’s medical history might be difficult due to possible dementia, therefore, the help of relatives, life partners, or both is mandatory.
The typical onset of iNPH occurs in the elderly population (older than 60 years), but it may appear earlier. The patient’s age should be at least 40 years to have a probable diagnosis of iNPH.3 Younger age does not rule out iNPH, but it makes the diagnosis less likely.
4.2 Symptoms of iNPH
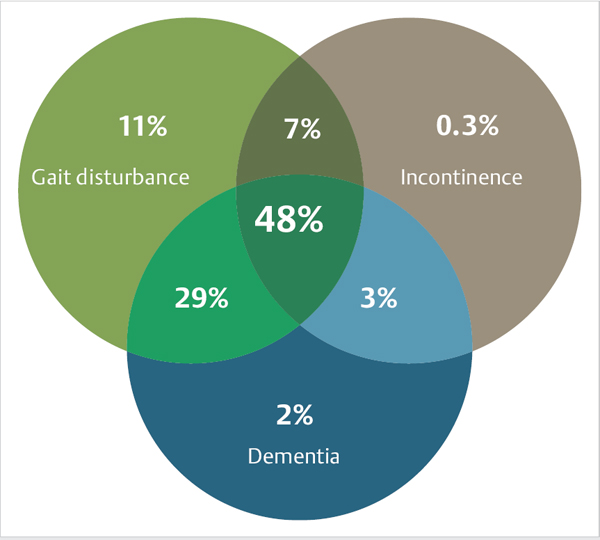
The typical triad of iNPH is gait disturbance, incontinence, and dementia, but all three symptoms will present simultaneously in about only one-half of patients.6 Gait disturbance is almost always present, whereas incontinence or dementia alone caused by iNPH is extremely rare (▶ Fig. 4.1). Several authors deny the diagnosis of iNPH if gait disturbance is not present.1 A list of the symptoms of iNPH is given in Box ▶ Symptoms of iNPH.
Symptoms of iNPH
Main symptoms
Gait disturbance
Incontinence
Dementia
Additional symptoms
Headache
Psychiatric syndromes
Dizziness/vertigo
Extended need of sleep
Large head circumference
Impairment of sexual function
Comorbidities
4.2.1 Main Symptoms
Gait Disturbance
Gait disturbance is typically the first symptom noted and is thought to be an apraxia of gait. The gait disturbance is characterized by decreased gait velocity and cadence with shorter and more variable strides (see Box ▶ Typical gait characteristics in iNPH). The step height is reduced and the dorsal extension of the forefoot is insufficient. The patient’s feet may shuffle on the floor; this has also been described as glued to the floor or as a magnetic gait.7 The gait is atactic and broad-based; when perturbed, the patient may lose balance. Patients may also have problems when they begin walking or when turning. In contrast to Parkinson disease (PD), patients with normal pressure hydrocephalus (NPH) have a preserved reciprocal arm swing,8 with a backward-directed posture and a tendency to fall. In the late stage of the condition, apraxia of the upper limbs may also occur.
Typical gait characteristics in iNPH
Atactic
Broad-based
Slow
Short step size
Magnetic gait, shuffling
Preserved reciprocal arm swing
In the early stages of iNPH, the gait disturbance is subtle, difficult to detect, and may be difficult to classify as NPH gait. Patients often complain about gait disturbance or slight balance problems, which they describe as dizziness, which cannot be recognized by others. If gait disturbance has progressed and is distinct, then it may be easily recognized as gait disturbance related to iNPH. In its final stages, patients can walk only with massive support and may become bedridden.
Incontinence
Increased urinary frequency and urgency is often found toward the onset of the disease (see Box ▶ Typical bladder symptoms in iNPH). The gait disturbance may accentuate the urgency, because it impedes reaching the toilet in time. In advanced stages, complete urinary incontinence and even fecal incontinence may be present.3 Less commonly, voiding difficulty is found; 14% of patients with iNPH have a postvoid residual of more than 100 mL.9
Typical bladder symptoms in iNPH
High urinary frequency
Urinary urgency
Complete urinary incontinence
Fecal incontinence (rare)
Pathophysiologically, the bladder dysfunction in iNPH is the sequela of a neurogenic bladder dysfunction with detrusor overactivity, which was noted in 95% of patients.9
The incontinence in iNPH is not as well described in the literature as compared with the other symptoms of gait disturbance and dementia.
Dementia
Dementia in iNPH corresponds to a frontal subcortical dementia with psychomotoric slowing, apathy, affective indifference, inattentiveness, and memory deficits (see Box ▶ Typical signs of mental disorders in iNPH).3 Intellectual abilities seem to be present, but in a sleepy, blurred condition with loss of spontaneity and communication.10 Patients may not be able to answer questions right away (akinetic mutism), but, after insisting, there will be a delayed answer that is often correct.10,11 Symptoms may range from subtle to severe.
Typical signs of mental disorders in iNPH
Psychomotor slowing
Apathy
Affective indifference
Inattentiveness
Memory impairment
Differentiating dementia seen in iNPH from other forms of dementia may be difficult because symptoms may be blurred by comorbidities that often exist such as AD and cerebrovascular disease.2
Pathophysiology of Dementia in iNPH
The cause of dementia in iNPH is not understood, but the frontostriatal system, subcortical structures, and periventricular projection fibers may be involved.3
4.2.2 Other Symptoms
Headache
Headache is typically found in high-pressure hydrocephalus; however, it is invariably present in iNPH as well. Exact data about the frequency of headache in NPH are not available, and headache as a symptom of iNPH is controversial. Although some authors almost neglect headache, others consider headache to be an important NPH symptom, much like Kiefer et al12 who assigned headaches the same importance as complete urinary incontinence or severe gait disturbance in the grading score named after him. Headache is usually felt as “pressure in the head.” If headache is present in NPH, then it is also important to evaluate its improvement after a spinal tap test as well as after shunting.
Psychiatric Syndromes
Psychiatric syndromes may appear in parallel with iNPH, but, in some cases, they may appear as a symptom of iNPH, as described in several case reports.3,13,14,15 Depression, mania, paranoia, and others were described as resolving with shunt treatment; however, the pathogenesis is not clear. Knowledge of psychiatric syndromes is important, though, because typical symptoms seen in NPH may be obscured by psychiatric disorders and adequate therapy may be withheld.
Dizziness/Vertigo
Often patients complain about dizziness/vertigo, but it is difficult to objectively assess this uncomfortable feeling. Many clinicians suggest dizziness is the subjective sensation of gait ataxia and the fear of falling. In fact, it often disappears simultaneously with gait improvement after shunting. Dizziness is also addressed in the Kiefer grading scale of iNPH, reflecting that dizziness is at least one of the more or less important subjective symptoms of iNPH.12 However, dizziness may also be a sign of the comorbidities of NPH, particularly cerebral microangiopathy.
Extended Need of Sleep
Patients with iNPH usually sleep more than healthy people, as reported by patients and their relatives, although reliable data are missing. Dementia with missing impulses, interest, and—hence—boredom may be the cause. The raised need for sleep decreases after shunting.16,17
Large Head Circumference
Patients with iNPH often have a significantly larger head circumference compared with the normal population.18 This observation supports the assumption that congenital asymptomatic hydrocephalus plays a role in the development of iNPH at least in some patients.18
Impairment of Sexual Function
Sexual dysfunction in patients with iNPH is often not evaluated and, if present, it is assumed to be a normal complaint of an older person. However, in some cases, a regained variable sexual desire may be observed after treatment.19
Comorbidities
Nearly 90% of patients with iNPH have comorbidities such as cardiovascular diseases, diabetes mellitus, PD, and AD.2 Sometimes it is difficult to differentiate between the comorbidity and the primary disease (i.e., AD, cerebrovascular disease, PD). Frequent coexistence also raises the question of similar pathogenetic pathways of NPH, AD, and cerebrovascular disease. The importance of comorbidities was recognized by Kiefer who developed and introduced the comorbidity index, which suggests a clear impact on the outcome after shunting.20,21 Therefore, comorbidities of NPH must be recognized because they play a role in further treatment indications.
4.3 Differential Diagnosis
Many other diagnoses may mimic iNPH (see Box ▶ Differential diagnosis of iNPH). Knowledge of the differential diagnoses is essential for making the correct diagnosis as well as for initiating the correct treatment. To achieve this, the most important differential diagnoses are described below, with their differentiation from iNPH.
Differential diagnosis of iNPH
Secondary normal pressure hydrocephalus
Chronic obstructive hydrocephalus
Parkinson disease
Alzheimer disease
Binswanger disease/cerebrovascular disease
Brain atrophy
Cervical myelopathy
Lumbar spinal canal stenosis
4.3.1 Secondary NPH and Chronic Obstructive Hydrocephalus
If there are clinical signs of NPH along with a preexisting condition that could interfere with cerebrospinal fluid (CSF) resorption, such as meningitis, subarachnoid hemorrhage (SAH), traumatic brain injury (TBI), then we are referring to secondary NPH (sNPH). However, the causative factor for NPH remains unclear and is controversial if these events were only of a moderate severity and/or occurred many years or even decades ago. Therefore, no clear limit can be defined between iNPH and sNPH.
In iNPH and sNPH, no direct obstruction of the CSF pathways can be seen in imaging. This assumes that there is a communicating hydrocephalus, which is in contrast to chronic obstructive hydrocephalus, where often an aqueductal stenosis or fourth ventricle outlet obstruction is seen.
Symptoms
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree