Clinical Epilepsy
QUESTIONS
1. Discontinuation of phenytoin during epilepsy monitoring is most likely to first activate:
A. Polymorphic delta activity
B. Epileptiform discharges
C. Ictal discharges
D. Triphasic waves
View Answer
1. (C): Antiepileptic drugs are often discontinued during inpatient epilepsy monitoring to precipitate seizures or ictal discharges. Discontinuation of phenytoin has not been associated with activation of epileptiform discharges, but epileptiform discharges may be activated by seizures. Similarly, phenytoin therapy does not suppress epileptiform discharges. (Ebersole and Pedley 2003, pp. 464-467)
On the other hand, valproate has been shown to reduce or suppress generalized 3 Hz spike-and-wave discharges.
2. The electroencephalography (EEG) of a migraineur will likely reveal:
A. Generalized slowing
B. Occipital spikes
C. Enhanced photic drive
D. All of the above
View Answer
2. (D): Migraine can produce a variety of EEG abnormalities. The reported EEG changes include generalized slowing (or focal in hemiplegic migraines), loss of normal alpha rhythm, enhanced photic drive, and attenuated beta activity. Occipital spikes were also reported in basilar migraines. In the absence of specific EEG changes in migraine, there is little justification in obtaining EEGs for migraineurs. (Ebersole and Pedley 2003, p. 324)
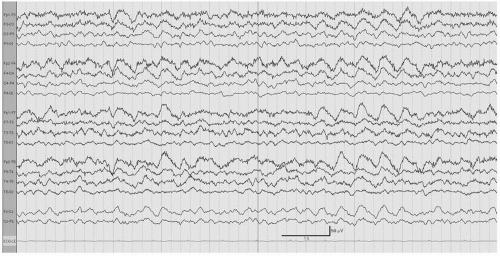
3. The EEG recording shown in Figure 7.1 is that of a 67-year-old man with dementia. The likely diagnosis is:
A. Picks disease
B. Subacute sclerosing panencephalitis
C. Creutzfeld-Jakob disease
D. Herpes encephalitis
View Answer
3. (C): This EEG tracing (Fig. 7.1) is displayed in a longitudinal bipolar montage. The background activity is disorganized with diffuse irregular delta activity. There are frequent periodic broad sharp waves with a left frontotemporal predominance recurring at 0.5 to 1 cps. These findings along with the clinical history of dementia are consistent with the diagnosis of Creutzfeld-Jakob disease. Creutzfeld-Jakob disease is characterized clinically by a rapidly progressing dementia, motor dysfunction, and startle myoclonus. In this condition, the discharges can be asymmetrical (in this case more on the left). These discharges may become more frequent and persistent after stimulation and maybe associated with myoclonic jerks. In the absence of clinical information, this pattern is nonspecific. Of note, this EEG pattern may be transient in the course of Creutzfeld-Jakob disease. (Blume, Kaibara and Young 2002, pp. 462-468)
4. Prolonged slow activity after hyperventilation is most likely the result of:
A. Hyponatremia
B. Hypocalcemia
C. Hypoglycemia
View Answer
4. (C): Hyperventilation is an activation technique routinely performed in outpatient EEG recording. Patients are asked to hyperventilate for 3 or 5 minutes. This technique is primarily performed to activate generalized 3 Hz spike-and-wave discharges and absence seizures. In normal individuals, there is appearance of diffuse high-voltage synchronous or asynchronous delta activity. This response is more prominent in children and becomes progressively milder and shorter with older age. It usually subsides within 1 minute of the end of hyperventilation. However, it is well documented that hyperventilation effect on the EEG depends also on blood glucose. Hypoglycemia is known to cause a prolonged EEG response from hyperventilation. (Ebersole and Pedley 2003, pp. 130-132; Blume, Kaibara and Young 2002, pp. 81-87)
5. A simple partial seizure with olfactory hallucination will be likely recorded at:
A. F7
B. T5
C. P3
D. F3
View Answer
5. (A): Seizures with olfactory hallucinations most often arise from the uncus, and are most likely to involve the anterior temporal (F7) and midtemporal (T3) electrodes. (Niedermeyer and Lopes Da Silva 1999, p. 491; Abou-Khalil and Misulis 2006, pp. 10-12)
6. A 22-year-old man has infrequent auras of strange epigastric feeling followed by confusion, lip smacking, right arm dystonic posturing, and automatism of the left hand. In the postictal state, patient is unable to communicate for approximately 5 minutes. His seizure onset will most likely be in the:
A. Nondominant mesial temporal lobe
B. Dominant mesial temporal lobe
C. Nondominant neocortical temporal lobe
D. Dominant neocortical temporal lobe
View Answer
6. (B): The clinical semiology of this complex partial seizure is highly suggestive of mesial temporal lobe epilepsy (MTLE). Auras of rising abdominal sensation and fearful feelings are common in that syndrome. Also, oroalimentary automatism (such as lip smacking), dystonic posturing, and limb automatism are more common in MTLE. As for lateralization, postictal aphasia is highly predictive of dominant hemisphere involvement, and dystonic posturing is contralateral to the ictal discharge. More commonly seen in neocortical temporal lobe epilepsy are auditory auras and early facial clonic activity. (Wyllie, Gupta and Lachhwani 2005, pp. 365-367)
7. Generalized 3 Hz spike-and-wave discharges were first described by:
A. Jean-Martin Charcot
B. Gibbs and Gibbs
C. Henri Gastaut
D. Hans Berger
View Answer
7. (B): Gibbs and Gibbs were the first to describe the generalized 3 Hz spike-and-wave discharge seen in absence seizure. Hans Berger was the first physician who recorded brain activity from humans using electrodes. Jean-Martin Charcot was a famous 19th century neurologist. Henri Gastaut was a neurologist with extensive original work on epilepsy. (Niedermeyer and Lopes Da Silva 1999, pp. 5-7; Wyllie, Gupta and Lachhwani 2005, pp. 169-170)
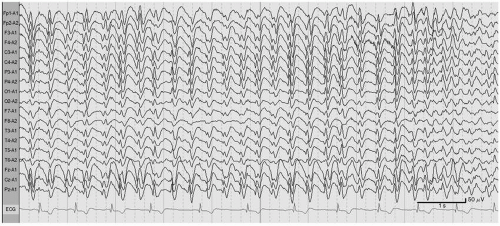
8. The EEG recording shown in Figure 7.2 is most consistent with:
A. Roving eye movements
B. Sweat artifact
C. Encephalopathy
View Answer
8. (C): This EEG tracing (Fig. 7.2) is displayed in a longitudinal bipolar montage. There is a bilateral frontal intermittent rhythmic delta activity (FIRDA). This EEG pattern indicates a nonspecific generalized cerebral dysfunction. It is frequently seen in patients with encephalopathy. Its frontal predominance is due to the fact that this pattern is regarded as a projected rhythm of disrupted thalamocortical projections. FIRDA is a normal finding during drowsiness, but can be seen with several pathologic processes. Unlike temporal intermittent rhythmic delta activity (TIRDA), this EEG pattern is not usually associated with higher risk of seizures. (Ebersole and Pedley 2003, pp. 295-296; Blume, Kaibara and Young 2002, p. 472)
9. Which of the following drugs can activate epileptiform discharges?
A. Clorazepate
B. Chloral hydrate
C. Clozapine
D. Promethazine
View Answer
9. (C): Clozapine is a selective dopamine receptor blocker used in refractory schizophrenia. Clozapine can induce a variety of EEG changes ranging from slowing to activation of epileptiform discharges and seizures. Epileptiform discharges are usually seen in the form of bilateral spike-and-wave discharges maximal in the anterior sagittal regions. Rapid titration and high doses of clozapine increase the risks of seizures. Clorazepate produces excessive beta activity, more than chloral hydrate. (Ebersole and Pedley 2003, pp. 468-470)
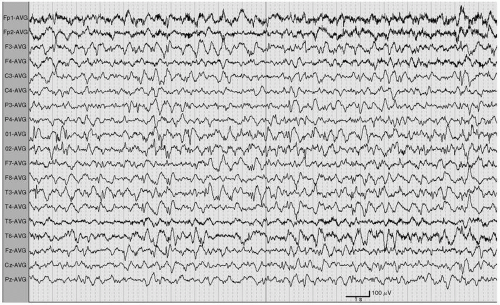
10. The EEG of a typical spell of an 11-year-old girl is shown in Figure 7.3. Among the following antiepileptic drugs, which is the most appropriate choice to make?
A. Carbamazepine
B. Ethosuximide
C. Tiagabine
D. Gabapentin
View Answer
10. (B): This EEG tracing (Fig. 7.3) is displayed in an ear referential montage. There is a continuous and rhythmic 3-Hz spike-and-wave discharge with bifrontal predominance. This EEG pattern is consistent with a typical absence seizure.
Ethosuximide is the drug of choice for isolated typical absence seizures. The remaining three antiepileptic drugs are effective against partial onset seizures only. (Blume, Kaibara and Young 2002, pp. 328-329; Wyllie, Gupta and Lachhwani 2005, pp. 823-824)
11. Seizures can be caused by all of the following electrolyte imbalances except:
A. Hypernatremia
B. Hypercalcemia
C. Hypermagnesemia
D. Hyperkalemia
View Answer
11. (C): Several electrolyte derangements can provoke seizures. These include hyper or hyponatremia, hyper or hypocalcemia, hypomagnesemia, or hypophosphatemia. The critical factor in precipitating seizures is the rate of electrolyte concentration changes rather its absolute concentrations. On the contrary, hypermagnesemia is known to be protective against seizures and magnesium sulfate is the drug of choice in seizure prevention in patients with eclampsia. (Ebersole and Pedley 2003, pp. 360-361)
12. All of the following characterize frontal lobe complex partial seizures except:
A. Tendency to cluster
B. Long duration
C. Abrupt start and end
View Answer
12. (B): After temporal epilepsy, frontal lobe epilepsy is the second most common type of partial epilepsy accounting for approximately 20% to 30 % of cases. Frontal lobe complex partial seizures are relatively brief seizures with an abrupt start and end, with a tendency to cluster or cause status epilepticus. They also tend to rapidly generalize. Often they have absent or short postictal states. (Wyllie, Gupta and Lachhwani 2005, pp. 367-368)
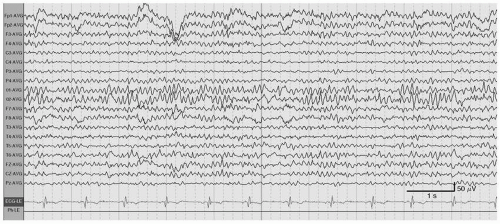
13. The EEG recording shown in Figure 7.4 is that of a 2-year-old boy. The findings are most consistent with the diagnosis of:
A. Lennox-Gastuat syndrome
B. West syndrome
C. Benign rolandic epilepsy
D. Landau-Kleffner syndrome
View Answer
13. (B): This EEG tracing (Fig. 7.4) is displayed in an average referential montage. There are high-voltage disorganized waves (shown in the calibration mark) intermixed with multifocal asynchronous spikes and sharp waves. There are also intervening periods of generalized attenuation. These findings are most consistent with hypsarrhythmia, an EEG pattern typically associated with infantile spasms of West syndrome. Hypsarrythmia may be diffuse or may predominate in one hemisphere. The periods of attenuation are variable and are best appreciated during non-rapid eye movement (NREM) sleep. This EEG pattern may be missed if sensitivity of the recording is not adjusted to allow better visualization of the giant waveforms. (Blume, Kaibara and Young 2002, pp. 157-159, 212-216)
14. The EEG of a 42-year-old man with an ammonia level of 82 µmol/L will most likely show:
A. Spike-and-wave discharges
B. Periodic lateralized epileptiform discharges
C. Triphasic waves
D. Normal attenuated EEG
View Answer
14. (C): Hyperammonemia occurs with hepatic encephalopathy. EEG findings depend on the degree of encephalopathy and vary from slowing of the background to severe attenuation. In moderate stages of hepatic encephalopathy like in this case, triphasic waves are commonly seen in adult patients. Triphasic waves are not specific to hepatic failure, but are reported to occur more commonly in this condition than in other metabolic states. (Ebersole and Pedley 2003, pp. 359-360)
15. In juvenile myoclonic epilepsy, myoclonic seizures are best recorded:
A. During sleep
B. After awakening
C. After a heavy meal
D. At any time
View Answer
15. (B): Myoclonic seizures are the key seizure type in patients with JME. They consist of mild to moderate jerks of the arms, legs, or trunk. Similarly to generalized tonic-clonic seizures of JME, they tend to cluster after awakening in the morning or after naps, especially after sleep deprivation. Other known triggers are fatigue, stress, and alcohol. (Wyllie, Gupta and Lachhwani 2005, pp. 392-393)
16. The EEG recording shown in Figure 7.5 is that of a 12-year-old girl. The slowing in the occipital electrodes is most consistent with:
A. Mild encephalopathy
B. Cortical blindness
C. Posterior tumor
View Answer
16. (D): This EEG tracing (Fig. 7.5) is displayed in an average referential montage.
There is a normal symmetrical 11 Hz posterior rhythm intermixed with transient slower activity in the delta range during wakefulness. This is consistent with the posterior slow waves of youth. This EEG pattern is common in children aged 8 to 14 years but can be seen up to 21 years of age. It shares the same distribution and reactivity as the alpha rhythm. (Ebersole and Pedley 2003, pp. 115-123; Blume, Kaibara and Young 2002, pp. 43-45)
17. A 14-year-old male with myoclonic jerks and generalized convulsive seizures is admitted for long-term video EEG study. If a generalized seizure is recorded with clonic-tonic-clonic evolution, the interictal EEG will most likely show:
A. 1 Hz spike-and-wave discharges
B. 3 Hz spike-and-wave discharges
C. 4 to 6 Hz spike-and-wave discharges
D. Temporal lobe sharp waves
View Answer
17. (C): A generalized seizure starting in the clonic phase is usually caused by a cluster of repeated myoclonic seizures before generalization. This is commonly seen in JME, which typically has an interictal pattern of 4 to 6 Hz spike-and-wave or polyspike-and-wave discharges. (Wyllie, Gupta and Lachhwani 2005, pp. 393-394)
18. A 26-year-old woman with unusual spells and depression is admitted for long-term video EEG study in conjunction with phenytoin withdrawal. Four short spells of asynchronous leg bicycling are recorded. Mental status was not tested during any of the recorded spells but was intact at the end of each spell. EEG remained normal throughout the study. What is the next most appropriate step?
A. Continue video EEG recording
B. Start fluoxetine
C. Consult psychiatry
D. Discharge patient home
View Answer
18. (A): The stereotypy of these spells is highly suggestive of seizures. The brief duration, the bicycling movements, and the absence of a postictal state are all highly suggestive of frontal lobe seizures. The epileptic nature of the attacks may become more clear as seizures become more severe with antiepileptic drug (AED) withdrawal, particularly with secondary generalization. It is not uncommon to have absent interictal abnormalities or even no definite ictal changes on scalp EEG in some frontal lobe seizures. This is mainly due to the inability to record deeply located dipoles. (Wyllie, Gupta and Lachhwani 2005, pp. 242-243, 249)
19. During a long-term video EEG study, a 3 Hz spike-and-wave discharge is being recorded. What should the examiner do?
A. Turn the patient to his left side
B. Give IV lorazepam STAT
C. Test the patient’s level of consciousness
D. Pinch the patient’s hand
View Answer
19. (C): The classification of seizure types according to the International League Against Epilepsy classification is based on both clinical and electrographic features. To diagnose absence seizures, impaired awareness should be demonstrated during the generalized 3 Hz spike-and-wave discharge. (Wyllie, Gupta and Lachhwani 2005, pp. 308-309, 347-363)
20. All of the following are EEG requirements for the evaluation of brain death except:
A. A minimal core temperature of 36C or higher
B. A minimum of eight scalp electrodes
C. A minimum interelectrode distance of 8 cm
D. A sensitivity of 2 µV/mm for at least 30 minutes
View Answer
20. (C): EEG revealing electrocerebral inactivity can be used as a supportive tool in the evaluation of brain death. The minimal requirements used are as follows:
Absence of sedation and normal core temperature
Minimum of eight scalp electrodes
Interelectrode impedance more than >100 Ω and <10,000 Ω
Sensitivity of 2 µV/mm for at least 30 minutes
Appropriate filter setting
Absence of reactivity (Daube 2002, pp. 104-105)
21. Which of the following drugs at low doses is the least likely to activate beta activity?
A. Lorazepam
B. Phenobarbital
C. Clorazepate
D. Chloral hydrate
View Answer
21. (C): Among the drug listed, chloral hydrate is least likely to produce beta activity, especially at low doses. This is the main reason why it is commonly used as a sedative in children undergoing EEG recording. Benzodiazepines (lorazepam and clorazepate) and barbiturates (phenobarbital) are strong inducers of beta activity, even at low doses. (Fisch 1999, p. 97)
22. In a patient with suspected epilepsy and one negative 20minutes awake outpatient EEG, all of the following can increase the yield of the subsequent outpatient EEG recording except:
A. Record the next EEG for 2 hours
B. Perform the next EEG with sleep deprivation to help obtain sleep
C. Schedule the next routine EEG no earlier than 1 week after a typical spell
D. Obtain a 24-hour ambulatory EEG study
View Answer
22. (C): Performing an additional EEG will increase the yield in patients with epilepsy. In many patients, sleep is essential to activate epileptiform discharges. Prolonging the next recording, using sleep deprivation, and obtaining a longer study with sleep are all useful. In addition, obtaining a study in the postictal state may improve the yield, because seizures activate epileptiform discharges and the EEG may also record postictal slow activity. There is no advantage in delaying the EEG after a seizure. (Wyllie, Gupta and Lachhwani 2005, p. 170)
23. Which of the following conditions is the least likely to show an abnormal EEG?
A. Multiple sclerosis
B. Advanced Alzheimer’s dementia
C. Glioblastoma multiforme
D. Middle cerebral artery infarct
View Answer




23. (A): Among the neurologic conditions listed, multiple sclerosis is the least likely to show abnormalities on EEG. Middle cerebral artery infarct and gioblastoma multiforme are the most likely to show abnormalities ranging from focal slowing to epileptiform or ictal discharges because of the focal structural nature of the disease. Alzheimer’s disease is almost always associated with slowing of the posterior rhythm, especially in moderate to severe cases. (Ebersole and Pedley 2003, pp. 387-390)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree