Clinical Outcome Following Surgical Treatment of Spondylolysis
Brian J. C. Freeman
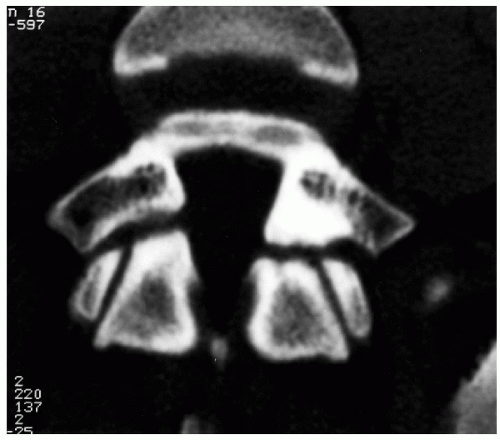
The pars interarticularis defect is unique to human beings, who by virtue of being bipedal transfer considerable weight through the pars interarticularis structure in the lumbar spine (1,2,3) (Fig. 34.1). Radiographic screenings have demonstrated an incidence of 4.4% in children between the ages of 5 and 7 years. The incidence of symptomatic pars defects in the young athletic population is much higher and is variously reported between 15% and 47% (4,5,6,7).
For those who fail conservative care, there are a number of surgical options. Direct repair of the pars defect has been shown to be effective for those with a normal disc, and it preserves intervertebral motion. Many different techniques have been described, including Buck’s direct repair (8), Scott’s wiring technique (9), Morscher’s hook-screw (10), translaminar screws (11), pedicle screws with a V-shaped rod (12), and a cable screw construct (13).
Successful outcomes have been reported, ranging from 63% in one series (14) to 100% in another series (15). Predictors of successful surgical outcome include age less than 25 years, spondylolysis of less than 4 mm, absence of disc degeneration, positive response to local anaesthetic infiltration of the pars interarticularis defect, method of surgical repair, and motivation of the individual undergoing surgery (16).
For those patients with established disc degeneration identified on magnetic resonance imaging (MRI), many surgeons who have written on this topic would advocate investigation with lumbar discography to confirm the pain source. If discography confirmed the disc to be a pain source, most would advocate spinal fusion. Some authors have advocated surgical repair of the defect in combination with total disc replacement in such a case (Marnay T., personal communication). If spondylolysis is associated with a lowgrade spondylolisthesis (Meyerding Grade 1 or 2), Dai et al. have suggested that direct repair of the defect and facet fusion produces acceptable results (17).
For those patients with a spondylolytic spondylolisthesis Grades 1 or 2 without objective neurologic deficit, most surgeons whose work is published would advocate fusion in situ; a minority would advocate reduction of the spondylolisthesis and fusion. One study compared anterior lumbar interbody fusion (ALIF) with instrumented posterolateral fusion (IPLF) for isthmic spondylolisthesis (Meyerding Grades 1 to 2) (18). No statistically significant difference was observed in clinical outcome between the two groups; satisfactory results were obtained in 85% of the ALIF group and 90% of the IPLF group. Another study of patients with isthmic spondylolisthesis reported superior long-term outcomes following noninstrumented posterolateral fusion compared to instrumented posterolateral fusion (19).
THE BIOMECHANICAL EFFECTS OF SPONDYLOLYSIS AND ITS TREATMENT
Biomechanical studies performed on fresh frozen calf lumbar spines have shown that artificially induced bilateral interarticularis defects increase the intervertebral mobility not only at the involved level but also at the upper level adjacent to the lysis (20). The increased mobility of both the lytic segment and the adjacent level was significantly reduced by the Buck screw repair. However, if a pedicle screw system was applied across the involved segment, the mobility in the adjacent segment was increased. It would appear that fixation of the pars defect alone causes less adjacent-level mechanical stress than pedicle screw-rod fixation of the motion segment.
Deguchi et al. carried out a biomechanical comparison of various fixation techniques employed for the repair of spondylolytic defects (21). The procedures were carried out on calf cadaveric lumbar spines. The four techniques that were compared were Scott’s wiring technique (wire loops passed around each transverse process and tightened under the spinous process); modified Scott’s technique (wire loops around cortical screws placed in both pedicles and tightened under the spinous process); Buck’s technique; and screw-rod-hook fixation. All fixation techniques significantly increased stiffness in the spondylolytic segment. The screw-rod-hook fixation and Buck’s technique allowed the least motion across the spondylolytic defect when tested in flexion. The authors suggest that Buck’s technique resists forces and movements in all directions, is low profile, and is less expensive than the screw-rod-hook system, but it remains technically demanding. Screw breakage or nerve root irritation requiring screw removal has occurred following Buck’s technique (8,22).
Kip et al. carried out biomechanical testing of various pars defect repairs (23). He compared the Buck screw with the Morscher hook-screw and a modified Scott wiring technique. Overall, the Buck screw provided the stiffest and strongest repair (with a mean repair stiffness of 64% of the intact stiffness), followed closely by the Morscher hook-screw (with a mean repair stiffness of 52% of the intact stiffness). The figure 8 wiring repair (modified Scott repair) was the least stiff, with a mean repair stiffness of only 3% to 4% of the intact stiffness. The authors conclude that Scott wiring of pars defects is a tension band repair that
is loaded only in flexion. It is used to repair a defect whose probable cause is repetitive hyperextension of the spine and should be questioned on biomechanical grounds. Nevertheless, it is interesting to note that similar clinical results have been obtained with both Buck’s technique and Scott’s wiring technique in some series (21).
is loaded only in flexion. It is used to repair a defect whose probable cause is repetitive hyperextension of the spine and should be questioned on biomechanical grounds. Nevertheless, it is interesting to note that similar clinical results have been obtained with both Buck’s technique and Scott’s wiring technique in some series (21).
CLINICAL OUTCOME FOLLOWING DIRECT REPAIR OF SPONDYLOLYTIC DEFECTS
The advantages of direct repair include a high rate of defect healing, preservation of intervertebral motion by avoidance of fusion across the disc, and restoration of anatomy.
BUCK’S TECHNIQUE
Buck (8) first reported the direct repair of a pars defect with a 4.5-mm stainless steel Arbeitsgemeinschaft für Osteosynthesefran or Association for the Study of Internal Fixation (AO) cortical lag screw in 1970 (Fig. 34.2). The defect was packed with cancellous bone graft and the patient was allowed to be mobile immediately following surgery. Kimura had described the insertion of bone-graft without internal fixation for spondylolysis and spondylolisthesis 2 years earlier (24). However, Kimura’s technique required the patients to remain on bedrest for 2 months and was not universally popular. Buck initially reported on 16 patients with only 1 failure (8). In 1979, he updated his results to a 75-patient series, reporting satisfactory results in 88% (25). Several series of patients were then reported in the literature with success rates varying from 72% (22) to 95% (25) (Table 34.1).
Van der Werf et al. presented a series of 12 patients in 1985, with 8 good, 2 fair, and 2 poor results (26). There were two documented pseudarthroses in this series, one with a fair result and the other with a poor result. Pedersen and Hagen described 18 patients who underwent a direct repair using Buck’s technique for a slip of Grade 1 or less (3). They reported 15 patients with a good or excellent result and 3 with a poor result (all with radiographic evidence of pseudarthrosis).
Roca et al. (27) reported on 15 patients with a slip of Grade 1 or less treated with the Buck method. There were 13 good results and 2 poor results (attributable to a
pseudarthrosis). In 1989, Bonnici et al. reported on 24 patients, 21 of whom obtained excellent results (28). Seventeen patients had adequate radiographic follow-up revealing 5 with screw loosening and 1 with a broken screw. Interestingly only 7 of 17 were noted to have healing of both defects radiographically, 5 patients had bridging of one defect, and 5 patients had no evidence of healing.
pseudarthrosis). In 1989, Bonnici et al. reported on 24 patients, 21 of whom obtained excellent results (28). Seventeen patients had adequate radiographic follow-up revealing 5 with screw loosening and 1 with a broken screw. Interestingly only 7 of 17 were noted to have healing of both defects radiographically, 5 patients had bridging of one defect, and 5 patients had no evidence of healing.
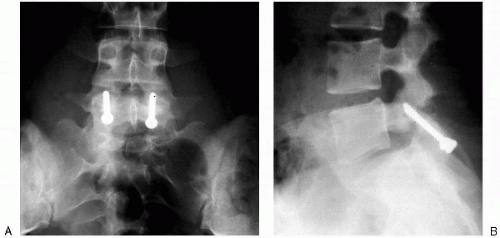 FIG. 34.2. Anteroposterior (A) and lateral (B) radiographs showing a bilateral Buck repair 6 months after operation. |
TABLE 34.1. Published results of Buck’s direct repair for spondylolysis | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree