Chapter 152 Complex Lumbosacropelvic Fixation Techniques
Anatomic and Biomechanical Considerations
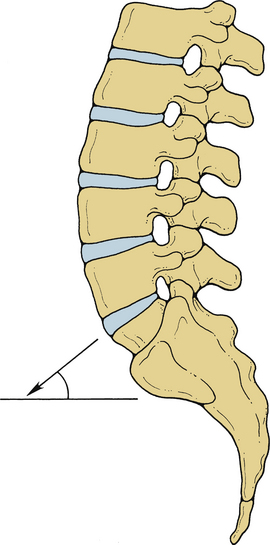
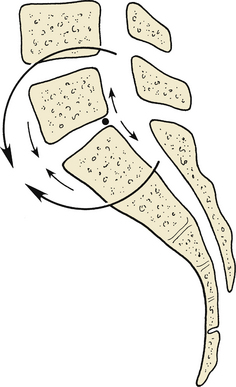
The LSJ is a unique spinal level in several respects.1 In the sagittal or flexion-extension axis, it has the largest range of motion of any thoracic or lumbar level, averaging 17 degrees of total movement. In the axial plane and during rotation and lateral (coronal plane) bending, the LSJ has the most limited range of motion of any spinal level, averaging 1 degree of rotation and 3 degrees of bending, respectively.2 Because of the normal lordotic curvature of the lumbar spine, the slope of the lumbosacral intervertebral disc (L5-S1) is usually the steepest of any disc, with respect to the true horizontal. The summation of spinal load vectors results in exposure of the lumbosacral disc to the largest loads encountered throughout the spine. The large loads carried and the angular position of the disc at the LSJ produce unique load-bearing characteristics, including the highest level of translational shear force in the entire spine (Fig. 152-1).1,3,4
Sacrum
The sacrum is formed from five fused vertebrae in which the specially adapted and large transverse processes merge into thick lateral masses, the alae. The sacral spinal canal has four pairs of dorsal and ventral foramina. The subdural and subarachnoid spaces terminate as the thecal sac tapers at the caudal margin of S2. The filum terminale internum is an extension of the pia arachnoid of the conus medullaris, extending from the tip of the conus to the end of the subdural space. At the termination of the subdural space, the thecal sac tapers to invest the filum terminale internum and form the filum terminale externum. The filum terminale externum extends to the end of the sacral canal and attaches to the rostral portion of the coccyx.
Sacroiliac Joint
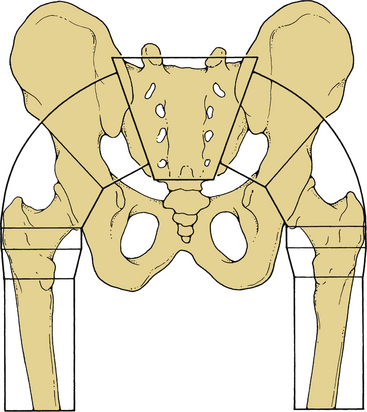
The SIJ is formed by the interdigitating surfaces of the sacral alae and the iliac bones. It is predominantly a fibrocartilaginous amphiarthrodial (no synovial capsule) joint. There is a small diarthrodial (synovial capsule present) portion located at the ventral aspect of the SIJ. The interdigitation and matching contours of the iliac and sacral alar surfaces create an interlocking mechanism to help stabilize the joint. The wedgelike shape of the sacrum helps stabilize the SIJ and serves to transfer loads from the spine to the pelvis (Fig. 152-2).
The SIJ is essentially an immobile joint that functions as a shock absorber for the spine. In studies on fresh cadavers, there was minimal motion in pediatric specimens, and none in adults.5 Another cadaveric study has demonstrated that in adults older than 50 years of age, autofusion of the joint is observed in 75% of specimens.6
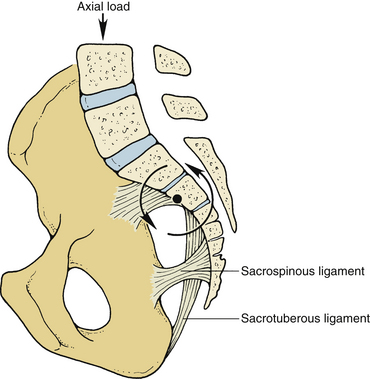
The major biomechanical function of the pelvis is that of transferring loads from the SIJ to the hip joints. The stable transfer of these loads is dependent on the ligaments connecting the lumbar vertebrae and the sacrum to the pelvis. The ligamentous structures spanning the SIJ include the interosseous, dorsal, and ventral sacroiliac ligaments (Fig. 152-3). The interosseous, sacroiliac, and dorsal sacroiliac complex provides the major stabilization for the SIJ.
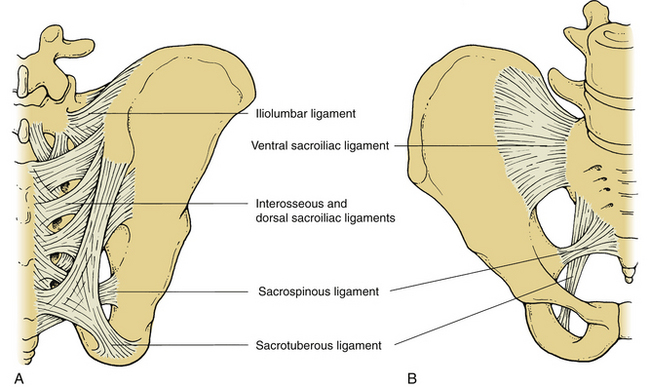
FIGURE 152-3 Dorsal (A) and ventral (B) views of the major ligamentous attachments of the sacroiliac joint.
The force vector of axial load from the spine is located ventral to the SIJ. This causes a ventral rotational tendency of the sacrum at the level of the SIJ. The center point of this rotational vector is located near the center of the S2 vertebral body (Fig. 152-4). The sacrospinous and sacrotuberous ligaments pass from the lower sacrum to the ischial bones. The position of these ligaments creates a long moment arm through which they are able to resist sacral rotation and are thereby able to maintain the lordotic lumbosacral posture despite the gravitational sagittal plane vector.
Muscular Interactions
In the resection of sacral tumors, stability of the sacropelvic region can be jeopardized because portions of the sacrum and possibly the SIJ are removed. Resection of the caudal portion of the sacrum up to the S1-2 interspace and removal of up to one third of the SIJ can be performed with only a 30% loss of weight-bearing capacity. The lower half of the S1 body and up to one half of the SIJ can be resected with a 50% loss of weight-bearing stability.7 Preservation of 50% of weight-bearing capacity is adequate for early ambulation in the postoperative period, and further stabilization is not likely to be necessary. In general, in cases of tumor or other destructive lesions of the sacral (e.g., infection), the bilateral alae should be evaluated. If one ala or more than 50% of bilateral alae are destroyed, the patient will require lumbopelvic fixation.
Indications for Lumbosacralpelvic Fixation
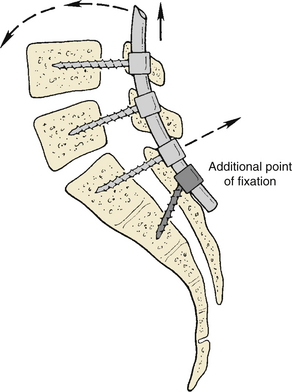
In short-segment cases and in the absence of osteopenia, sacral fixation with a single pair of bone screws is adequate. In longer-segment cases (e.g., scoliosis, postsacrectomy reconstruction, and multisegmental lumbosacral fusion) or with osteoporotic bone, more substantial segmental fixation is required to achieve rigidity. In addition, when high-grade lumbosacral spondylolistheses (grades III and above) are reduced, standard sacral screws may be inadequate and lead to loosening or sacral fracture. Rigidity is a crucial element in these constructs because fusion rates are directly related to use of rigid instrumentation, and better outcomes clearly correlate with the acquisition of a solid fusion.8–15 If a long instrumentation construct is placed, the sacral attachment is usually subjected to large cantilevered forces that may lead to screw pull-out (Fig. 152-5). Additional points of sacral or sacropelvic fixation may prevent complications in such cases.
The SIJ is autofused in many adults older than 50 years of age. Long-term follow-up study of patients with instrumentation constructs crossing the SIJ has demonstrated no adverse effects relating to the presence of the implants.16 Therefore, if it is necessary for additional security of fixation in the lumbosacropelvic region, placement of instrumentation across the SIJ is a rational approach for providing spinal stability.
Lumbosacral Pivot Point
In a study of the biomechanics of sacropelvic fixation, McCord et al. described the concept of the lumbosacral pivot point.17 This is the axis of rotation at the lumbosacral junction. During flexion, the portions of L5 and the sacrum that are ventral to this pivot move toward one another. Likewise, the portions of L5 and the sacrum located dorsal to this pivot point will move apart during flexion (Fig. 152-6). Anatomically, the lumbosacral pivot point is marked by the intersection of the middle osteoligamentous column and the lumbosacral (L5-S1) disc. In constructs that cross the SIJ, only those devices that pass ventral to this point provide a significant biomechanical advantage regarding rigidity of fixation.
Complex Techniques of Sacral Fixation
Many lumbosacral fusions can be adequately immobilized with placement of bone screws into the sacral pedicles. These screws, however, obtain their thread purchase in the broad cancellous channel of the sacral pedicle. Therefore, bone screws in the sacral pedicles are subject to failure because of the relative porosity of the sacrum, the manner in which stress tends to be concentrated at the termini of a fusion construct, and the large flexion moments to which these constructs are subjected.18,19 Sacral screws may fail by pull-out or by fracture.18 In cases in which it is believed that the use of a single pair of bone screws may not be adequate for stabilization, the use of more complex techniques is warranted.
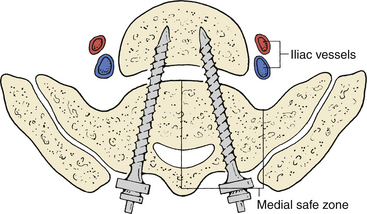
With regard to injuring structures ventral to the sacrum, cadaveric studies have shown that the widest margin of safety is found at the medial safe zone (Fig. 152-7).20 Therefore, placing the screws in a medial or toed-in direction is preferred at the S1 or promontory level. Some authors have advocated bicortical purchase of sacral screws to enhance pull-out resistance, which affords some pull-out strength advantage, although this involves additional risk.20–25 Zindrick et al. found that bicortical purchase with a 6.5-mm diameter screw resulted in an increase in pull-out strength of about 30%.25 Penetrating an excessive distance beyond the ventral cortex carries the risks of neurologic deficit, chronic pain from lumbosacral trunk injury, sympathetic chain injury, peritonitis, sepsis, and hemorrhage,20,24 although these risks are minimal if the screw penetrates 1 cm or less.
Fixation with Sublaminar Devices
The addition of sublaminar devices such as hooks, wires, or cables at the sacrum is a simple means of enhancing fixation. It should be borne in mind that the sacral laminae are often quite thin and may not provide substantial strength to hold such devices. All of these devices, including hooks, are tension-band fixators. Dorsally placed tension-band constructs provide limitation of flexion but do not provide substantial torsional stability or resistance to extension. With fusions at the LSJ, it has been shown that fixation with sublaminar devices alone does not improve the fusion rate when this rate is compared with that of noninstrumented fusions.26 Therefore, sublaminar devices should be used at the LSJ only in conjunction with other devices.
Although the bony thickness at the sacral lamina is meager, the bone stock is usually quite substantial at the nearby dorsal foramina. Thus, the dorsal foramina are excellent sites to place hooks for the purpose of enhancing construct strength. When added to a sacral pedicle screw construct, this technique has been shown to significantly increase rigidity.27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree