Front Neurol Neurosci. Basel, Karger, 2014, vol 33, pp 11-18 (DOI: 10.1159/000351888)
______________________
The Concept of Acute Cerebrovascular Syndrome
Shinichiro Uchiyama
Department of Neurology, Tokyo Women’s Medical University School of Medicine, Tokyo, Japan
______________________
Abstract
Early after the onset of transient ischemic attack (TIA), patients are at very high risk of stroke. There is no meaning to differentiate TIA in acute settings from acute ischemic stroke (AIS) only by the duration of symptoms. Acute TIA and AIS are on the same spectrum of acute ischemic syndrome in the central nervous system. We proposed a new concept termed acute cerebrovascular syndrome (ACVS), which includes TIA in acute settings and AIS. The concept of ACVS is comparable to acute coronary syndrome (ACS), which includes unstable angina and acute myocardial infarction. When a focal symptomatic reversible ischemia occurs in the brain, it is called TIA, and when a focal symptomatic irreversible ischemia occurs in the brain, it is called AIS. Patients with ACS share a single pathophysiological mechanism, that is rupture of unstable plaque followed by formation of plateletrich thrombi to plug up coronary arteries. Unlike ACS, the mechanism of ACVS is complicated, which is not only large artery atherosclerosis similar to ACS but also cardioembolism or small vessel occlusion. In addition, there are no measurable biomarkers for ACVS, while there are practical biomarkers for ACS. Nevertheless, the concept of ACVS is practical to emphasize the importance of immediate evaluation and starting treatment to prevent subsequent stroke in acute settings of TIA. Therefore, TIA in acute settings as well as AIS should be recognized as ACVS, which is a medical emergency.
Copyright © 2014 S. Karger AG, Basel
Importance and Definition of Transient Ischemic Attack
Transient ischemic attack (TIA) is well known to be a prodromal syndrome of ischemic stroke. In reality, 15-30% of patients with ischemic stroke have a history of TIA [1]. Rothwell and Warlow [2] have analyzed 4 studies (Oxford Vascular Study, Oxfordshire Community Stroke Project, UK TIA Aspirin Trial, and European Carotid Surgery Trial), and reported 23% of patients with ischemic stroke had a history of TIA. TIA is, however, easily neglected or underestimated by patients or their families because the symptoms naturally disappear without any treatment. According to a survey in the general population by the Japan Stroke Association, recognition of TIA as a risk factor for stroke was only 34.5%, which was much lower than that of hypertension (94.3%) or hypercholesterolemia (76.4%; fig. 1) [3]. Even by general physicians, TIA is non-prioritized since it is regarded as minor stroke. The TIA Study Group (principal investigator: Kazuo Minematsu) supported by the grant in aid for the Cardiovascular Research from the Japanese Ministry of Health, Labour and Welfare has conducted a survey on the recognition of TIA in general practitioners, and reported that only 42.9% of them answered to immediately consult with stroke-specialized hospitals for patients suspected of TIA in whom the symptoms had disappeared on examination (fig. 2) [4].
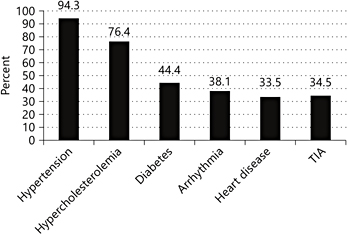
Fig. 1. Recognition of risk factors for stroke in the general population in a survey of the Japan Stroke Association.
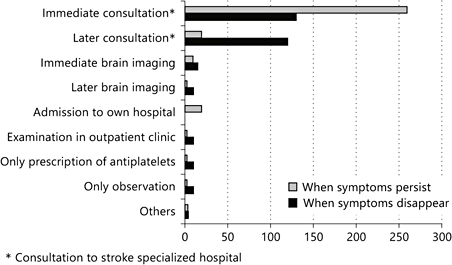
Fig. 2. Survey of general practitioners by the TIA Study Group (Cardiovascular Research of the Japanese Ministry of Health, Labour and Welfare).
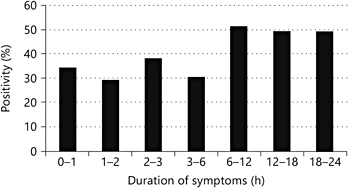
Fig. 3. Duration of neurological symptoms and positivity of DWI. Quoted and modified from Shah et al. [9].
However, TIA patients early after the onset are at very high risk of stroke. According to a population-based study of early risk of stroke after TIA or minor stroke by the Oxford Vascular Study, the estimated risks of recurrent stroke at 7 days, 1 month, and 3 months after a TIA were 8.0, 11.5, and 17.3%, respectively [5]. In addition, it has been reported that in patients who experienced stroke within 2 weeks after the onset of TIA, approximately 30% of stroke cases occurred within 24 h [2]. Therefore, TIA should be recognized to be an emergency requiring immediate evaluation and starting treatment.
There is no global consensus on the definition of TIA. In the classical criteria, TIA is defined as focal neurologic brain or retinal ischemic symptoms which disappear within 24 h [6]. However, the TIA Working Group in the United States defined TIA as brain or retinal ischemic symptoms within 1 h of the duration without responsible ischemic lesions [7]. Afterwards, the American Heart Association/American Stroke Association redefined TIA as transient focal ischemic symptoms in the brain, retina, or spinal cord without evidence of ischemic lesion regardless of the duration of symptoms [8].
New Concept of Acute Cerebral Ischemia
Distribution of the duration of TIA with positive MRI diffusion-weighted image (DWI) is continuous without any specific cutoff point (fig. 3) [9]. A pooled analysis of 808 patients from 10 centers demonstrated that DWI-positive lesions were present in 33%, and these DWI lesions frequently evolve into chronic ischemic lesions on follow-up T2 or fluid-attenuated inversion recovery images [9]. Thus, it is not possible to differentiate TIA from ischemic stroke by symptom duration. Finally, TIA and acute ischemic stroke (AIS) are on the same spectrum of acute ischemic syndrome in the central nervous system.
In the TIAregistry.org (www.tiaregistry.org), which is an international, multicenter cooperative, investigator-driven, web-based observational study, the members in the first steering committee meeting (2008 in Paris) proposed a new concept termed acute cerebrovascular syndrome (ACVS), which includes TIA in acute settings and AIS. The concept of ACVS is comparable to acute coronary syndrome (ACS; fig. 4). When a focal symptomatic reversible ischemia occurs in the brain, it is called TIA, and when a focal symptomatic irreversible ischemia occurs in the brain, it is called AIS. On the other hand, when a focal symptomatic reversible ischemia occurs in the heart, it is called unstable angina (UA), and when a focal symptomatic irreversible ischemia occurs in the heart, it is called acute myocardial infarction (AMI). Finally, UA and AMI are categorized into ACS; they share a single pathophysiological mechanism, that is rupture of unstable plaque followed by formation of platelet-rich thrombi to plug up coronary arteries [10, 11].
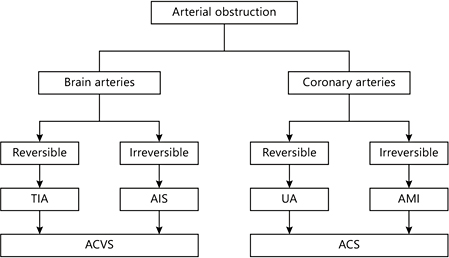
Fig. 4. Concepts of ACVS and ACS.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








