Confluent White Matter Lesions
Gary M. Nesbit, MD
DIFFERENTIAL DIAGNOSIS
Common
Aging Brain, Normal
Arteriolosclerosis
Chronic Hypertensive Encephalopathy
Multiple Sclerosis
Multi-Infarct Dementia
Hypotensive Cerebral Infarction
Cerebral Amyloid Disease
Less Common
Glioblastoma Multiforme
Radiation and Chemotherapy
HIV Encephalitis
PML
Encephalitis (Miscellaneous)
CADASIL
Inherited Metabolic Disorders
Metachromatic Leukodystrophy (MLD)
X-Linked Adrenoleukodystrophy (XLD)
Alexander Disease
Canavan Disease
Zellweger
Van der Knaap Leukoencephalopathies
Hypomyelination
ADEM
Enlarged Perivascular Spaces
Rare but Important
Lymphoma, Primary CNS
Lymphoma, Intravascular (Angiocentric)
Gliomatosis Cerebri
Hypothyroidism
CO Poisoning
Subacute Sclerosing Panencephalitis
Drug Abuse
Maple Syrup Urine Disease
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Confluent white matter (WM) lesions are all T2/FLAIR hyperintense & CT hypodense
Helpful Clues for Common Diagnoses
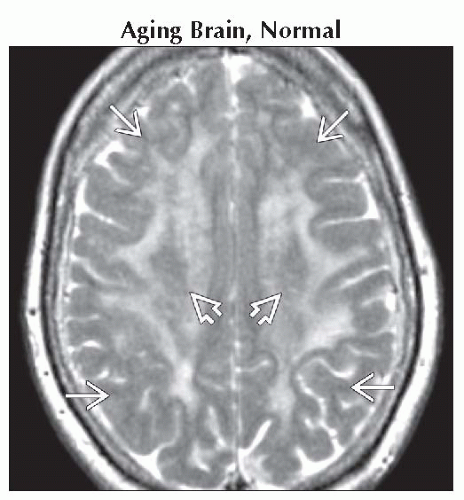
Aging Brain, Normal
Usually multiple T2 hyperintensities, but can become confluent in late elderly
Less severe for age than arteriolosclerosis or chronic hypertensive encephalopathy
Lack history of hypertension, diabetes, or other vascular disease
Arteriolosclerosis
Confluent periventricular & deep WM
Spares corpus callosum (CC)
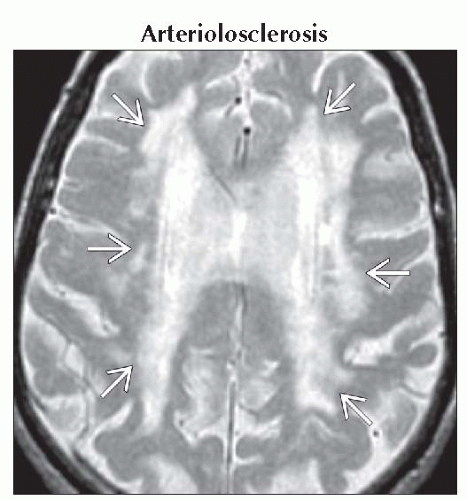
Chronic Hypertensive Encephalopathy
Basal ganglia (BG) lacunae typical
Usually deep, periventricular confluent T2 hyperintensities
Hypointense microhemorrhages on T2* common
Multiple Sclerosis
Radiating periventricular location, “Dawson fingers”
Acute tumefactive lesions large with hypointense T2 ring that enhances variable mass effect
Multi-Infarct Dementia
Similar to arteriolosclerosis & chronic hypertensive encephalopathy, but usually with peripheral & cortical infarcts
BG & pons infarcts common
Hypotensive Cerebral Infarction
Chronic hemodynamic hypotensive lesions are multifocal or confluent parasagittal WM lesions
Acute hypotension may result in confluent juxtacortical or diffuse WM lesion often associated with cortical necrosis
Cerebral Amyloid Disease
Confluent WM hyperintensity less common than peripheral multifocal lesions
Multifocal juxtacortical small infarcts & hemorrhages of varying ages common, with little to no BG involvement
Helpful Clues for Less Common Diagnoses
Glioblastoma Multiforme
Large confluent mass that may cross CC
Can have unusual spread patterns: Ependymal, pial, which can create large confluent regions
Radiation and Chemotherapy
Radiation necrosis may mimic high grade neoplasm; has low cerebral blood volume
Leukoencephalopathy: Diffuse confluent hyperintensity
HIV Encephalitis
Confluent diffuse WM hyperintensity with atrophy classic; spares subcortical U-fibers
PML
Large multifocal or confluent subcortical WM lesions without mass effect
Encephalitis (Miscellaneous)
Herpes encephalitis: Medial temporal & inferior frontal confluent T2 hyperintense
Predominantly cortical, but involves WM
Most non-herpes encephalitides involve BG, thalamus, midbrain, & WM
CADASIL
Onset at age 20-40 is common
Bilateral anterior temporal subcortical lesions appear early in diagnosis
External capsule involvement somewhat specific
After age 50, frontal lobe involvement develops into confluent lesions
Inherited Metabolic Disorders
Usually diffuse, confluent
Mitochondrial usually multifocal
All present in infancy, childhood, or rarely in young adults (Alexander disease, MLD)
ADEM
Multifocal lesions, punctate to flocculent
May become confluent when massive
Enhancement: Faint & fuzzy early, ring-like later
Usually 10-14 days following infection or vaccination
Enlarged Perivascular Spaces
Variable-sized clusters, CSF-like
Can cause focal mass effect
Helpful Clues for Rare Diagnoses
Lymphoma, Primary CNS
Callosal periventricular, may be peripheral, central isointense mass, modest mass effect
Lymphoma, Intravascular (Angiocentric)
Often confluent radiating periventricular hyperintensity along deep medullary veins
Gliomatosis Cerebri
Confluent or diffuse with minimal mass effect is typical
Hypothyroidism
Diffuse WM hyperintensity in Hashimoto encephalopathy
CO Poisoning
Diffuse WM hyperintensity in severe cases
Globi pallidi hyperintensity classic
Subacute Sclerosing Panencephalitis
Diffuse T2 hyperintensity extending into the gyri with CC involvement
Diffuse atrophy with severe WM volume loss late
No enhancement
Drug Abuse
Periventricular or diffuse WM pattern with inhaled heroin or rare vasculitis
Maple Syrup Urine Disease
Diffuse cerebellar & brainstem WM T2 hyperintensity with lesser supratentorial involvement
Alternative Differential Approaches
Inherited metabolic disorders
Macrocephaly: Canavan, van der Knaap, Alexander disease, mucopolysaccharidoses
Frontal: Alexander disease
Occipital: XLD
Image Gallery
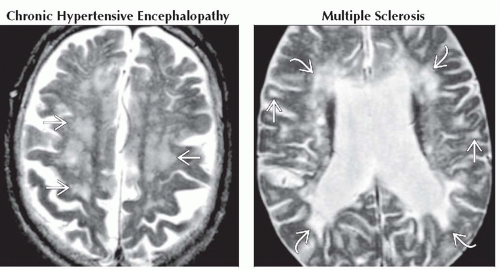 (Left) Axial T2WI MR shows patchy & confluent foci of hyperintensity in the centrum semiovale
 & atrophy. Although nonspecific, these findings are characteristic of chronic hypertensive encephalopathy. Associated basal ganglia infarcts & hemorrhage are common. (Right) Axial T2WI MR shows significant, predominantly white matter atrophy and confluent periventricular & atrophy. Although nonspecific, these findings are characteristic of chronic hypertensive encephalopathy. Associated basal ganglia infarcts & hemorrhage are common. (Right) Axial T2WI MR shows significant, predominantly white matter atrophy and confluent periventricular  , & juxtacortical , & juxtacortical  hyperintense plaques of severe chronic multiple sclerosis. hyperintense plaques of severe chronic multiple sclerosis.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|