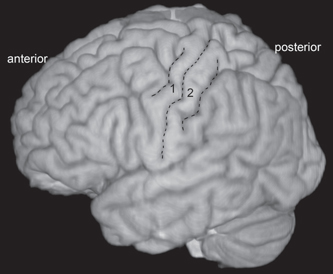
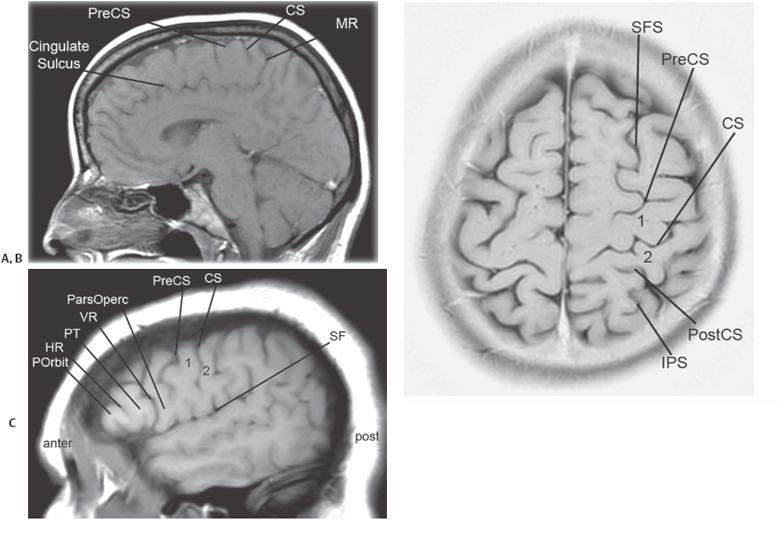
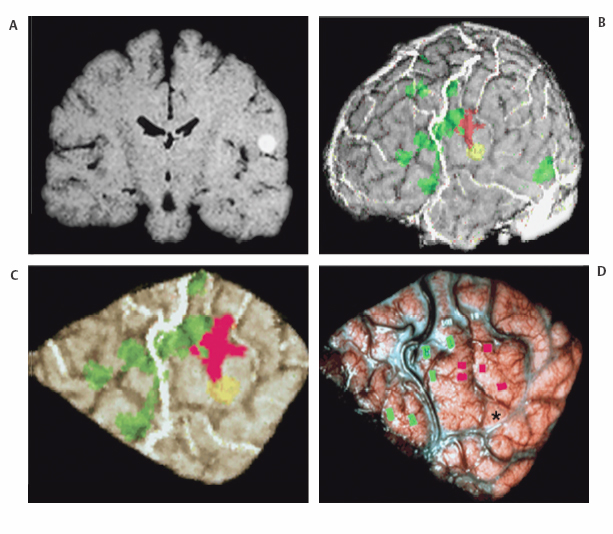
6 Cortical Resection in the Central Region The surgical treatment of epilepsy in the central region or rolandic cortex presents special challenges to neurosurgeons. Not only does the central region provide essential somatomotor and somatosensory control of the contralateral face and limbs, this region of the brain is highly epileptogenic. Lesions in this region often produce disabling and treatment refractory seizures, which can frequently result in episodes of focal status epilepticus. In this chapter, we will review the anatomy of the rolandic cortex, the seizure semiology, and the most appropriate presurgical evaluation as well as the various diagnostic and therapeutic surgical approaches in the management of intractable seizures of the central region. The central or rolandic region is composed of the pre- and postcentral gyri. The precentral gyrus or motor strip is anatomically the most posterior portion of the frontal lobe, whereas the postcentral gyrus or sensory strip is the most anterior portion of the parietal lobe. The two central gyri are defined by the vertically oriented central sulcus, which runs from the region of the sylvian fissure superiorly and posteriorly toward the interhemispheric fissure. The central region is further defined by the pre- and postcentral sulci, which run roughly parallel to the central sulcus. The precentral sulcus is often discontinuous in its mid-portion (Fig. 6.1). Whereas the pre- and postcentral gyri can be easily detected as the vertically oriented gyri in the central region of the brain on either an anatomical specimen or a three-dimensional (3-D) volumetric magnetic resonance imaging (MRI) rendering (Fig. 6.1), it is sometimes much more difficult to accurately define the central sulcus on standard sagittal, axial, or coronal MRI sections. Knowledge of sulcal anatomy and cerebral topography, however, can aid in the confident localization of the pre- and postcentral sulci even in the presence of local pathology. In the midsagittal plane, one can define the central sulcus by following the cingulate sulcus as it courses parallel to the corpus callosum to its marginal ramus that turns upward toward the vertex. The sulcus seen ~8 to 9 mm anterior to the end of the marginal ramus is the termination of the central sulcus (Fig. 6.2A). The marginal ramus of the cingulate sulcus defines the posterior border of the paracentral lobule, whereas the para-sagittal portion of the precentral sulcus defines its anterior border. On an axial MRI scan near the vertex, one can also follow the superior frontal sulcus, which travels parallel to the interhemispheric fissure ~15 to 20 mm off the midline. It typically terminates in a “T” intersection with the superior portion of the precentral sulcus. The two sulci running parallel and just posterior to the precentral sulcus are the central and postcentral sulci, respectively. The intraparietal sulcus is located on the lateral surface of the parietal lobe. It runs parallel to the interhemispheric fissure and often forms a T intersection anteriorly with the superior portion of the postcentral sulcus (Fig. 6.2B). In the axial MRI images near the vertex, it is also important to realize that the precentral gyrus or motor strip is actually wider and thicker than the postcentral gyrus. This is due to the fact that the gray matter in the precentral gyrus is on average 2.8 to 3.1 mm thick, whereas the gray matter cortical thickness in the sensory or postcentral gyrus is ~1.9 mm.1 It is often possible to see an omega-shaped gyrus or knuckle, which represents the somatosensory localization of hand function.2 One can also define the central region by its anatomical relationship to the sylvian fissure and the inferior frontal gyrus on a para-sagittal MRI scan. In most cases, one is able to discern the horizontal and vertical rami in the inferior frontal gyrus dividing this gyrus into the pars opercularis, pars triangularis, and par orbitalis. The first sulcus immediately posterior to the pars opercularis and extending to the sylvian fissure is the precentral sulcus. The sulcus just posterior and running parallel to this but not reaching the sylvian fissure is the central sulcus (Fig. 6.2C). The precentral gyrus or motor strip is composed of Brodmann’s areas 4 and 6. Cytoarchitecturally, these areas are composed of a six-layer neocortex with giant pyramidal cells, an almost complete absence of granular cells, and numerous densely packed intracortical fibers, especially in the plexiform layer. The postcentral gyrus or sensory strip is composed of Brodmann’s areas 3, 1, and 2. Cytoarchitecturally, this area contains granular cells and a modest number of pyramidal cells. It too has many intracortical connections along the postcentral gyrus and anteriorly into the precentral gyrus.3 These connections are essential to normal sensorimotor function. The postcentral gyrus receives large numbers of afferents from the ventral posterior medial and lateral nuclei of the thalamus. The precentral gyrus gets most of its afferent information via the ventral lateral nucleus of the thalamus from the cerebellum. A supplementary sensory area (SM2) lies at the inferior portion of the postcentral gyrus along the insula and parietal operculum with extension on occasion into the precentral region.4 There is some degree of somatotopy in this area, although it is much less distinct than in the primary somatosensory areas. Fig. 6.1 Three-dimensional brain reconstruction. View of lateral surface. Precentral, central, and postcentral sulci are outlined with dashed line. 1, precentral gyrus; 2, indicates postcentral gyrus. There are numerous thalamocortical and reciprocal connections in the central region. The primary efferent output of the central region is the corticospinal tract. This extends caudally from the central region, through the centrum semiovale, condensing as the pyramidal tract within the posterior limb of the internal capsule then distributing to their target motor nuclei either in the brainstem or spinal cord. There is a distinct and important somatotopic arrangement to sensorimotor function in the central region. Penfield and Rasmussen classically described this somatotopic organization with the tongue and face represented in the inferior portion of the central region near the sylvian fissure.5 The thumb, fingers, and hand are situated at the middle portion of the central region in the area of the omega gyrus with the upper extremity and trunk approaching the midline with parts of the lower extremity and foot in the paracentral lobule. The pharynx and oropharynx are typically localized along the operculum of the central region. Fig. 6.2 (A) T1 parasagittal MRI. PreCS indicates the precentral sulcus. MR indicates the marginal ramus. CS indicates the central sulcus. (B) T2 high-axial MRI. SFS indicates the superior frontal sulcus. PreCS, indicates the precentral sulcus. IPS indicates the longitudinally running intraparietal sulcus. PostCS indicates the laterally running postcentral sulcus. 1 indicates the precentral gyrus. 2 indicates the postcentral gyrus. (C) T1 midsagittal MRI. Inferior frontal gyrus subdivided into pars orbitalis (POrbit), pars triangularis (PT), and pars opercularis (ParsOperc). The horizontal ramus (HR) and vertical ramus (VR) define the PT. The inferior portion of the PreCS defines the posterior portion of the ParsOperc. SF indicates the sylvian fissure. With functional MRI, we can now create accurate structural and functional models of individual patients’ brains.6 First, a 3-D volumetric acquisition and surface rendering is acquired, and then functional imaging data are obtained while the subject performs a specific sensorimotor task. The areas of cortex activated during this task are then co-registered to the anatomical model thereby localizing the central sulcus. These images can be used preoperatively to define the location of the central region and plan surgical approaches (Fig. 6.3). The clinical semiology of seizures originating in the central region is much more stereotyped than focal epilepsy of the frontal, temporal, or parietal lobes. Seizures of the central region are rarely characterized by auras with subjective or emotional accompaniment. The majority of the attacks are heralded by primary somatomotor or somatosensory symptoms or signs. Seizures typically begin with clonic movements of the face, arm, or leg with no alteration of consciousness. The clonic movements may remain localized to the affected region or may spread and secondarily generalize. If the seizure spreads along the sensory or motor strip, the patient or clinician may observe progression of the clonic motor movements to involve more of the affected extremity or face and then spread to contiguous areas. This socalled Jacksonian march is the clinical accompaniment of the spread of epileptic discharges along the rolandic cortex.7 The seizure may stop at this point or may go on to a secondary generalized tonic-clonic convulsion. If the seizures involve the inferior portion of the motor strip where face and tongue are represented, the patient often experiences a speech arrest. This is true whether the seizure involves the dominant or nondominant hemisphere. Isolated focal tonic contraction of a limb is rare but when seen at the beginning of a seizure most often represents a more localized spread into supplementary motor areas with lesions closer to the interhemispheric fissure.8 Because of the lower threshold for epileptic discharges, seizures involving the central region can frequently result in focal status epilepticus or epilepsia partialis continua (EPC). These episodes of focal status epilepticus are often associated with very small, discrete and restricted lesions in either the somatomotor or somatosensory cortex and can be very difficult to control pharmacologically. Gliosis and post-inflammatory changes have been implicated in genesis of EPC especially in Rasmussen’s encephalitis.9 The characteristic clinical feature of EPC is focal myoclonus of the distal part of one extremity that may last for minutes, hours, or days. If the epileptic discharges are confined to a small cortical region, then the clonic movements may be confined to a single group of muscles or a single finger. At other times, more extensive muscle segments are involved, and the entire limb may be involved in the synchronous myoclonic jerks. It is common for patients to suffer a transient postictal paresis of minutes to hours.10
Anatomical Considerations
Seizures of the Central Region
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








