Cranial Nerve Palsies 3-6
Introduction
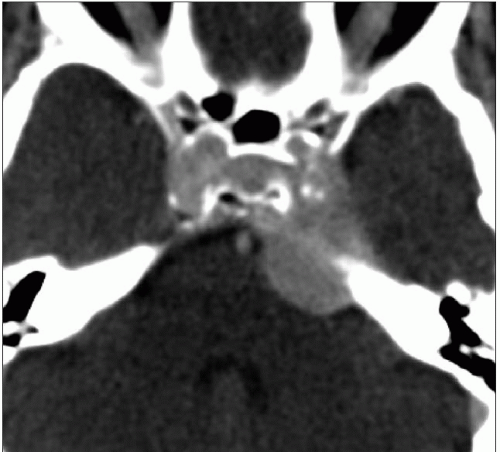
Palsies of the 3rd to the 6th nerves can be caused by pathology anywhere along the length of the nerve from the superior orbital fissure or the foramen ovale, through the cavernous sinus and the basal cisterns, to their nuclei in the mid brain (3 and 4) and pons (5 and 6). Any palsy can occur in isolation or in combination.
The volume of brain and skull involved is only about 6 cm in depth and so it is easy to use a short CT technique to examine all the possible sites of disease.
There are obvious anatomical overlaps in imaging of this busy part of the skull and brain and so you may need to refer to the chapters on the orbit, visual failure, and the pituitary to find illustrations of pathology in these sites which could be associated with a palsy of the 3rd to the 6th nerves.
The multiple sites and number of pathologies possible make this a most challenging (and most rewarding) area for the radiologist. Getting a rare diagnosis or detecting a subtle abnormality here could make your reputation! It is essential to give IV contrast and use a submillimetre helical scan to achieve best resolution and tissue differentiation. The contrast timing depends upon the likely clinical cause. If an aneurysm is suspected (e.g. isolated painful 3rd nerve palsy with pupillary involvement) then MDCTA as for the Circle of Willis is best. If cavernous sinus (multiple palsies) or skull base pathology (facial pain) seems most likely, then a venous timed scan is best (see Chapters 11 and 12).
If in doubt, do an MDCTA and plan a duplicate scan to follow at venous timing (60 seconds delay) or at 5 minutes delay if the first processed scan suggests a nonvascular mass (see Chapter 2). It is necessary to include the skull base from the hard palate to the orbital roof, as invasive tumours of the nasopharynx can spread along the nerves into the cavernous sinus and beyond.
Technique
The scan set up is as for the ‘visual failure’ protocol (Chapter 4) using a submillimetre helix with the timing of the contrast dependent upon the above clinical considerations. This is why it is so important to understand the exact nature of the clinical question being asked and why good clinical understanding and interactions are essential for optimizing neuroimaging. It is important to be present to supervise and direct these examinations to ensure maximum information from minimum scanning.
Reconstruction and reformation
Pathology and illustrations
Superior orbital fissure associated with proptosis
(Orbital apex syndrome)
Orbital granuloma
Neuroma
Nasopharyngeal malignancy with perineural spread
Cavernous sinus
Neuroma
Meningioma
Nasopharyngeal malignancy with perineural spread
Aneurysm/fistula (see Chapter 3) Cavernoma
Thrombosis (see Chapter 11)
Infection: bacterial, fungal
Secondary tumour
Lymphoma
Sphenoid sinus/clivus
Infection
Tumour: primary and secondary
Midline granuloma