Cranial Nerve Palsies 7-12
Introduction
The cranial nerves 7-12 arise in the brainstem, medulla, or upper cervical spine and exit the cranium from the posterior fossa. Clinically they present with a variety of different signs and symptoms. The facial nerve can be involved in pathology in the petrous bone, infratemporal fossa and face as it passes anteriorly towards and within the parotid gland so necessitating bone and soft tissue information. One common referral for MR imaging is the patient who presents with unilateral deafness or tinnitus as it can exclude even a very small intracannicular acoustic schwannoma on the 8th nerve. CT is poor at defining such a small tumour within a bony canal, but can detect tumours as small as 6 to 8 mm which extend beyond the internal acoustic porus if MR is contraindicated. The 9th, 10th, and 11th cranial nerves exit medial to the jugular vein in the jugular foramen and, therefore, often present with a constellation of complaints including difficulty in swallowing, hoarseness, and weakness of neck and shoulder movement. As much of their function is involved with innervation of glands, heart, and digestive tract, clinical signs can be sparse. A neuroma of a nerve can present as a face or neck mass with minimal or no abnormal neurology.
The hypoglassal nerve exits though a canal anterolateral to the foramen magnum and disease here will cause a palsy of the tongue on the same side.
As many of these cranial nerves have a long path through extracranial soft tissues it is necessary to include the craniocervical junction, face and neck in the examination. MDCT has completely changed the way disease of the cross-over area between these regions is assessed routinely. The ability of CT to show high resolution bone, soft tissue, and blood vessel, and review them in any plane or combination, is unique and why MDCT is of such benefit.
Applied techniques
If the presentation involves the 7th, 8th, or 12th nerves then a thin section helical contrast enhanced scan (Chapter 2) with reprocessing with both bone and soft tissue filters should suffice. The facial area should be included for facial nerve assessment, so the scan is started at the level of C3.
If disease of the jugular bulb is suspected, and here it is necessary to include patients with tinnitus or audible bruit because of the likelihood of a glomus tumour, then it is best to use an angiographic technique. The MDCTA technique as described in Chapter 8 is used, but with a delay of 40 seconds from the start of the injection, rather than an aortic triggered start, to ensure some venous filling. This technique is also used for presurgical assessment of vessels adjacent to a tumour in the posterior fossa or skull base.
Reconstruction and reformation
Thin section MPR (e.g. 2 mm) in orthogonal and curved planes with angiographic MIP and VR3D are usually all employed in addition to review of the base images. A wide window setting is necessary to distinguish vessels and vascular tumour from adjacent bone (e.g. 150 WC/450 WL as for venography). Specific presurgical questions must be clearly defined before the examination is performed to ensure that it will be answerable from the scan.
Pathology and illustrations
Intra-axial
Demyelination
Brain stem tumour
Extra-axial
Meningioma
Metastatic tumour
Arachnoid cyst
Epidermoid tumour
Nerve
Neuroma
Schwannoma
Paraganglioma
Glomus tympanicum
Glomus jugulare
Carotid body tumour
Vascular
Aneurysm, AVM
Bone
Dysplasia
Infection
Cholesterol granuloma
Tumour: primary /secondary
Soft tissues
Tumour
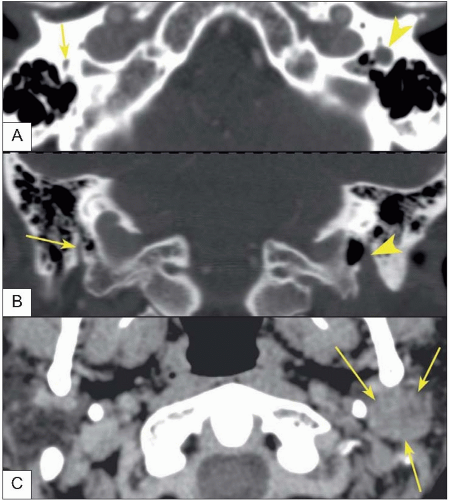
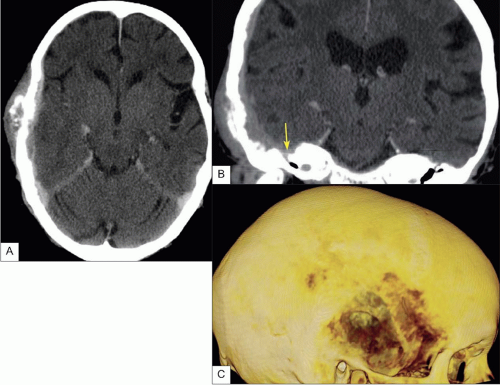 12.1 This patient presented with a right facial palsy. MDCT demonstrated a bony metastatic deposit on the outside of the skull which had grown through the bone (A, C) into the extradural space and spread over the petrous bone (B) to involve the facial ganglion (arrow). The 3D skull image defines the extent of the bone involvement, including the little skip deposit posterosuperior to the main deposit. |
Many of the pathologies listed above are demonstrated in previous chapters and will not be repeated here. Those specific to the clivus, jugular bulb, and foramen magnum and extension into the neck will now be considered.
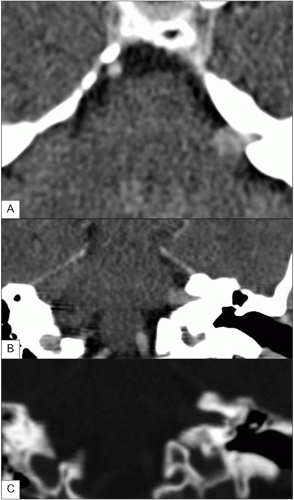 12.3 Acoustic schwannoma. It is useful to remember that modern CT will show small acoustic tumours which extend out of the IAM a little way (A, axial; B, coronal). (C) Shows erosion of the bony spur separating the 7th from the 8th nerves within the left IAM. (See also 2.7.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|