General
 History and Physical Examination
History and Physical Examination
1. What is the most common type of headache?
Tension headache
2. What lesions can produce a head tilt?
Trochlear (IVth) nerve palsy, anterior vermis lesion, tonsillar herniation. In myasthenia gravis, the head tilts back.1
3. What is the term for the vermicular movement of the face in a patient with pontine demyelination?
Myokymia2
4. What disorders can benefit from deep brain stimulation (DBS) of the ventral intermediate (VIM) thalamic nucleus?
Essential tremor and parkinsonian tremor3,4
5. What region of the internal capsule may be affected in a patient with dysarthria and clumsy-hand syndrome?5
The genu
6. Dilute pilocarpine (0.1–0.125%) may constrict what type of pupil?
An Adie pupil. This is possibly because of denervation supersensitivity as the normal pupil reacts only to 1% pilocarpine. A pharmacologic pupil (dilated for the purpose of examination by an ophthalmologist) will not constrict with 1% pilocarpine; however, a pupil that is dilated from a compressive third cranial nerve palsy may constrict with 1% pilocarpine.6
7. What is the term given when the consensual light reflex is stronger than the direct light reflex?
Afferent pupillary defect. The lesion is ipsilateral to the side of the impaired direct reflex.7
8. What is the most common cause of spontaneous diplopia in middle-aged people?
Orbital Graves disease is the most common cause of spontaneous diplopia in this age group. It can present with normal thyroid function tests. The inferior and medial rectus muscles are involved first. The patient may present with marked lid edema, lid retraction, and ophthalmoplegia. Dysthyroid disease may occur unilaterally and with normal thyroid function tests, which makes this diagnosis difficult. Steroids are helpful in the acute setting.8
9. Which Parkinson-like disease manifests with vertical gaze palsy?
Progressive supranuclear palsy (also known as Steele-Richardson-Olszewski syndrome)7
10. In one-and-a-half syndrome, which eye movement is preserved?
Abduction of the unaffected eye9
11. How can one differentiate an oculomotor palsy from an aneurysm versus an oculomotor palsy from diabetic neuropathy?
An oculomotor palsy in diabetes usually occurs with pain and may occur with pupillary sparing, which helps to distinguish it from an aneurysmal cause. Anatomically, the parasympathetic fibers on the oculomotor nerve are at the periphery; therefore, a compressive lesion such as an aneurysm will compromise these fibers first.10
12. What disease is characterized by ataxia, myoclonus, positive immunoassay for 14–3-3 protein, and bilateral sharp waves on electroencephalogram (EEG)?
Creutzfeldt-Jakob disease (CJD)11
13. What tests can be performed to differentiate an actual seizure from a pseudoseizure?
EEG, serum prolactin level, and muscle enzyme studies11
14. What type of electrical activity occurs with an absence seizure?
3 Hz per second spike and wave12
15. How does the diplopia of myasthenia gravis differ from the diplopia of a compressive lesion?
The diplopia of myasthenia is intermittent, whereas the diplopia of a compressive lesion is constant or worsening.7
16. What extraocular muscle may be involved if a horizontal object appears slanted?
Superior oblique muscle13
17. How does one differentiate the hypertension from a pheochromocytoma versus essential hypertension?
Clonidine suppression test (reduces only essential hypertension). If no decrease in plasma catecolamine levels is detected after giving a 0.3 μg/kg oral test dose the study is considered positive (pheochromocytoma).14
18. What do lesions of the bilateral hippocampi produce?
Recent memory impairment15
19. In what percentage of left-handed subjects is the left hemisphere dominant?
Over 75%16
20. What are the clinical symptoms of normal pressure hydrocephalus (NPH)?
The chief feature is gait disturbance; the other two major components are memory loss, usually for recent events, and urinary incontinence. These features are similar to Alzheimer disease, but in Alzheimer disease the memory loss is out of proportion to the gait disorder. A good clue to NPH is that gait disturbance is usually the first symptom to appear and may precede the other symptoms by months to years. If rigidity and tremor occur, these patients can be diagnosed incorrectly with Parkinson disease. Other diseases in the differential diagnosis are depression and multiinfarct dementia. A computed tomography (CT) scan of the brain in NPH shows large ventricles out of proportion to atrophy. The cerebrospinal fluid (CSF) pressure measured by lumbar puncture is not high for unknown reasons. A good test to show that an NPH patient may improve with a ventriculoperitoneal shunt is to place a lumbar drain for a few days and watch for any improvement (especially of gait, which is very predictive).17
21. What is the name of the area involved with cortical inhibition of bladder and bowel voiding that is damaged in NPH?
The paracentral lobule17
22. What other diseases must first be ruled out to be confident about the diagnosis of NPH?
Vascular dementia, Parkinson disease, Lewy body dementia, cervical spondylotic myelopathy, and peripheral neuropathy17
23. What are the synapses that occur in the pupillary reflex?18
• An afferent impulse through the optic nerve to the superior colliculus
• The superior colliculus to the Edinger-Westphal nuclei bilaterally
• From the Edinger-Westphal nucleus through the third cranial nerve to the ciliary ganglion
• From the ciliary ganglion via the short ciliary nerves
24. If there is a problem with pupillary response, where is the lesion in relation to the lateral geniculate body?
Anterior to the lateral geniculate body19
25. What are some causes of circumoral paresthesia?
Hypocalcemia, hyperventilation, syringobulbia, and neurotoxin fish poisoning20
26. What is significant about the pitch of tinnitus?
Low-pitch tinnitus is seen in conductive deafness and Ménière disease; high-pitch tinnitus is seen with sensorineural deafness.21
27. What is the significance of a “transverse smile” in a patient with myasthenia gravis?
A myasthenic snarl (or transverse smile) may be seen with bulbar muscle involvement in myasthenia gravis.22
28. What diseases may manifest as facial myokymia?
Intrinsic brainstem glioma or multiple sclerosis (MS)2
29. What maneuver can elicit nystagmus characteristic of benign positional vertigo?
The Dix-Hallpike maneuver. The examiner turns the head of the seated patient to one side and pulls the patient backward into a supine position with the head hanging over the edge of the examining table; the patient then looks straight ahead and the examiner observes for positional nystagmus, which is indicative of benign positional vertigo.23
30. What are some characteristics of benign positional vertigo?
Fatigability is often seen and nystagmus is characteristic with rotatory movement in one eye and vertical movement in the other eye. Patients describe a “critical position” that either elicits the vertigo or alleviates the vertigo.23
31. What are some characteristics of Ménière disease?
Spontaneous bouts of prolonged vertigo, fluctuating hearing loss (poor speech perception), tinnitus, excessive endolymph within the scala media. It may mimic an acoustic neuroma.21
32. What are the major signs and symptoms of lateral medullary infarction?
Vertigo, nausea, vomiting, intractable hiccups, diplopia, dysphagia, dysphonia, ipsilateral sensory loss of facial pain and temperature, ipsilateral Horner syndrome, contralateral pain, and temperature loss of the limbs and trunk. This is also known as Wallenberg syndrome.24
33. What differentiates ptosis from third cranial nerve palsy from ptosis in Horner syndrome?
Horner syndrome ptosis is partial and disappears on looking up.25
34. What localizing value is the presence of anhidrosis in Horner syndrome?
If the lesion is proximal to the internal carotid artery (ICA) origin or involves the external carotid artery circulation then the anhidrosis is present along the face due to dysfunction of cervical sympathetic output. If the lesion is more proximal (along the first or second order neuron level) then the anhidrosis may involve a greater portion of the hemi-body.25
35. What are some causes of partial ptosis from a first-order Horner syndrome?
A first-order Horner syndrome involves the nerves from the posterolateral hypothalamus to the intermediolateral cell column (at C8–T2). Its causes include an Arnold-Chiari malformation, basal meningitis, basal skull fracture, lateral medullary syndrome, demyelinating disease, an intrapontine hemorrhage, neck trauma, pituitary tumor, and syringomyelia.25
36. What pharmacologic test can be used to determine if Horner syndrome is second order or third order?
Hydroxyamphetamine drops placed in the eye of a patient with Horner syndrome with intact postganglionic fibers (i.e., first- or second-order neuron lesions) dilates the pupil to an equal or greater extent than a normal pupil, whereas in an eye with damaged postganglionic fibers (third-order neuron lesions) the pupil does not dilate as well as a normal pupil after hydroxyamphetamine drops.25
37. What is Bell phenomenon?
On attempting to close the eyes and show the teeth, one eye does not close and the eyeball rotates upwards and outwards.26
38. What are some nutritional causes of dementia?
Wernicke-Korsakoff syndrome (thiamine deficiency), vitamin B12 deficiency, and folate deficiency
39. What is the name of the inherited disorder that presents with migraine (often hemiplegic) in early adult life, progressing through transient ischemic attacks (TIAs) and subcortical strokes to early dementia?
CADASIL. The disease CADASIL (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy) is a recently identified cause of stroke and vascular dementia. CADASIL is identified by finding mutations in a gene called Notch3, which influences how cells in blood vessels grow and develop.27
40. What tests or procedures can one perform to determine if a patient with NPH will benefit from a shunt?18
• The presence of β waves can be noted with intracranial pressure (ICP) monitoring for more than 4 hours over a 24-hour period.
• After lumbar CSF drainage for a few days, there is clinical improvement.
41. What is the most common cause of cardioembolic stroke?
Atrial fibrillation28
42. What arteries supply macular vision?
Posterior cerebral artery (PCA) and middle cerebral artery (MCA)29
43. What are symptoms of color desaturation in MS?
Patients complain about their perception of color; for example, the perception of red color as different shades of orange or gray.30
44. In acoustic schwannomas, when tumors are greater than 2 cm the trigeminal nerve may be involved causing facial pain, numbness, and paresthesias. What sign on CN examination may be an early manifestation of this phenomenon?
Depression of the corneal reflex on the side of the tumor is an early sign. Facial weakness is surprisingly uncommon despite marked CN VII compression.
45. At what diameter of the carotid vessel lumen does a carotid bruit manifest on auscultation?
Carotid artery bruits, often atherosclerotic in nature, become audible when the residual vessel lumen diameter approaches 2.5 to 3 mm; they later disappear as the lumen is thinned to 0.5 mm.31,32
46. What are some features of Cushing syndrome?
Moon face, acne, hirsutism and baldness, buffalo-type obesity, purple striae over flank and abdomen, bruising, muscle weakness and wasting, osteoporosis, hypertension, susceptibility to infection, and diabetes mellitus
47. What are conditions that may result in upgaze palsy?
Tumor on the quadrigeminal plate or pineal region (Parinaud syndrome), hydrocephalus or other causes of elevated ICP, Guillain-Barré syndrome, myasthenia gravis, botulism, hypothyroidism
48. In what percentage of patients will phenytoin result in a skin rash?
49. What is the diagnosis (until proven otherwise) of an adult patient who presents with recurrent meningitis without any other predisposing conditions?
CSF fistula. Recurrent meningitis in an infant may be a manifestation of basal encephalocele.
50. What is the other name of the disease known as cupulolithiasis?
Benign positional vertigo35
51. What causes horizontal diplopia?
Paresis of one or both of the sixth CNs. This may occur, for example, with pseudotumor cerebri as a false localizing sign. The firm attachment of the abducens nerve at the pontomedullary junction and its attachment to the dural elements as it passes into the Dorello canal make it susceptible to stretch forces in cases of high ICP.36
52. A cherry red spot in the retina is seen in which conditions?
• Tay-Sach disease
• Niemann-Pick disease
• Pseudo-Hurler syndrome (GM1 ganglioside)
53. Retinitis pigmentosa is seen in which conditions?
• Friedreich ataxia
• Refsum disease
• Cockayne syndrome
• Kern-Sayre syndrome
54. What is cerebellar mutism?
Mutism seen in children usually 1–4 days after a vermian lesion resection that may take weeks to months to resolve
55. What is the House-Brackman classification of a seventh cranial nerve injury?
• Grade I: Normal
• Grade II: Mild deformity and mild synkinesis
• Grade III: Moderate damage, good eye closure, forehead function is preserved
• Grade IV: No forehead function, partial eye closure
• Grade V: No eye closure
56. Which questions should be asked regarding seventh cranial nerve palsy?
• Ask about history of diabetes mellitus, pregnancy, autoimmune disorders, and ear/parotid surgery.
• Also inquire about otalgia, otorrhea, vertigo, and blurred vision as well as taste.
57. What is Melkersson-Rosenthal syndrome?
Triad of recurrent orofacial edema, recurrent seventh cranial nerve palsy, and lingua plicata39
58. What is Ramsay-Hunt syndrome?
• Herpes zoster oticus
• Third most common cause of seventh cranial nerve palsy
59. What is Heerfrodt syndrome?
60. Bilateral seventh cranial nerve palsy is indicative of which disease?
Lyme disease
61. What is Millard-Gubler syndrome?
Ipsilateral sixth and seventh cranial nerve palsy and contralateral hemiparesis41
62. What is Brissaud-Sicard syndrome?
Ipsilateral CN VII hemispasm and contralateral hemiparesis41
63. What is Foville syndrome?
Ipsilateral CNs VI and VII involvement and horizontal gaze paralysis with contralateral hemiparesis41
64. What is Panayiotopoulos syndrome?
Benign occipital lobe epilepsy in children (40% idiopathic). Presents between 1 and 14 years of age and includes eye deviation and myoclonic jerks. It is sleep-induced and has a good prognosis.42
 Techniques
Techniques
65. What is the diameter in millimeters of a 12-French suction tip used in neurosurgery?
Three French units equal 1 mm. A 12-French suction catheter has an outer diameter of 4 mm at the tip.
66. What is exposed from a properly placed burr hole at the keyhole area?
The frontal dura in the upper half and the periorbita in the lower half
67. Where is the keyhole in relation to the frontozygomatic point?
Directly above the frontozygomatic point43
68. What is the significance of the frontozygomatic point?
It is the location on the lateral orbital bone (~2.5 cm from the zygoma attachment), which if connected with the 75% point (three-fourths of the distance from the nasion to the inion) approximates the location of the sylvian fissure.43
69. An incision reaching the zygoma that is more than 1.5 cm anterior to the ear may interrupt what nerve?
The branch of the facial nerve that passes across the zygoma to reach the frontalis muscle43
70. Where are the skull landmarks for upper and lower Rolandic points?
Upper point is 2 cm behind the “50% point” and the lower point is midway on the zygoma. Connecting these two points approximates the location of the central sulcus.38
71. How can the internal auditory canal be identified below the floor of the middle fossa?
By drilling along a line ~60 degrees medial to the axis of the arcuate eminence, near the middle portion of the angle between the axis of the greater superficial petrosal nerve (GSPN) and axis of the arcuate eminence (Fig. 5.1)37
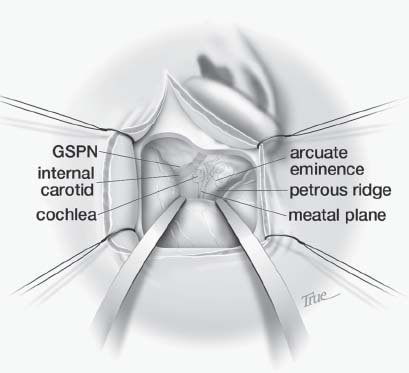
Fig. 5.1 Middle fossa approach for resection of vestibular schwannoma with labeled landmarks. GSPN, greater superficial petrosal nerve. (Reprinted with permission from Badie, p. 22844)
72. What types of variations on the subfrontal operative route are used to access a suprasellar craniopharyngioma or other lesions of the 3rd ventricle?
Lamina terminalis approach, opticocarotid approach through the opticocarotid triangle, subchiasmatic approach below the optic chiasm, and the transfrontal–transsphenoidal approach through the planum sphenoidale and sphenoid sinus (Fig. 5.2)45
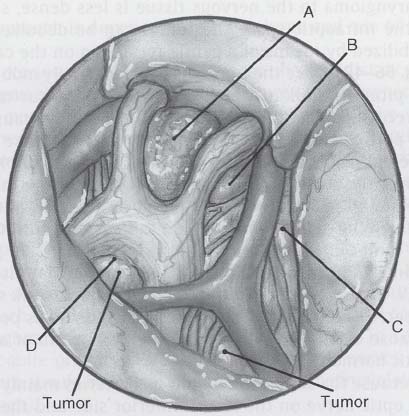
Fig. 5.2 Variation routes of the subfrontal approach to access suprasellar mass: A, between optic nerves; B, opticocarotid triangle; C, carotid-oculomotor triangle; D, lamina terminalis. (Reprinted with permission from Sekhar & Fessler, p. 68446)
73. What operative approach can be used for a tumor of the tegmentum of the midbrain?
Subtemporal transtentorial approach
74. What length of temporal tip may be safely removed from the nondominant side?
6–7 cm47
75. What are the initial steps in performing a superficial temporal artery biopsy?
Trace out the artery’s course with Doppler ultrasound, determine branching pattern, sample the frontal branch by dissecting the artery under microscope, and obtain a segment 3–5 cm long.48
76. What is the inferior frontal gyrus on the dominant hemisphere called?
Broca area
77. Through which triangle may one access the posterior fossa dura anterior to the sigmoid sinus?
The Trautman triangle49
78. Following the GSPN will lead to which ganglion?
The geniculate ganglion
79. What part of the internal capsule lies very close to the foramen of Monro?
The genu of the internal capsule50
80. After a callosal opening, how can one determine if one has opened the left or right lateral ventricle?
By observing the relationship of the thalamostriate vein and choroid plexus; the thalamostriate vein is located lateral to the choroid plexus (Fig. 5.3).51
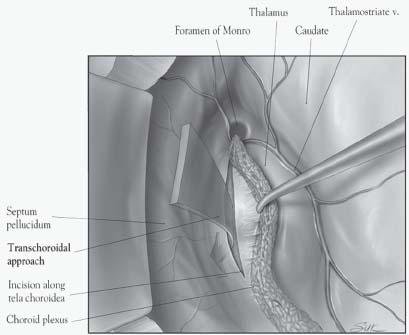
Fig. 5.3 Transcallosal approach to the lateral and 3rd ventricles. (Reprinted with permission from Badie, p. 5044)
81. After a callosal opening, if a surgeon determines that there are no intraventricular structures present, what most likely is the cause assuming he or she has proceeded correctly up to this point?
He has entered a cavum septum pellucidum.51
82. How can one enlarge the foramen of Monro in an operation for a large colloid cyst?
The ipsilateral column of the fornix can be incised at the anterosuperior margin of the foramen of Monro of the nondominant side. There is a risk of memory loss any time the fornix is manipulated. If access is needed to the mid portion of the third ventricle, opening the tela choroidea medial to the choroid plexus is a safe pathway.51
83. What nucleus of the thalamus may be damaged while opening the body of the choroidal fissure?
The dorsomedial nucleus51
84. What areas of bone may need to be removed to successfully clip a low-lying basilar artery aneurysm?
The posterior clinoids, or a portion of the dorsum sellae. An anterior petrosectomy may also be performed to clip the aneurysm.52
85. What are the boundaries in performing an anterior petrosectomy?
Behind the petrous ICA, in front of the internal acoustic meatus, and medial to the cochlea53
86. What are the pterional routes to a basilar aneurysm?
Opticocarotid triangle, between carotid bifurcation and optic tract, carotid–oculomotor triangle above the posterior communicating (PComm) artery, carotid–oculomotor triangle below the PComm artery52
87. In what cases would one approach an anterior communicating (AComm) artery aneurysm from the left?
In a dominant left A1, dome pointing to the right, another left-sided aneurysm, possibly a left-sided blood clot54
88. For a craniotomy, what are reasons to use a linear incision? A “lazy S” incision? A flap incision? A zigzag incision?
A linear incision increases blood supply to the wound. A “lazy S” incision is used to prevent the incision line in the dura from lying directly underneath the incision in the skin. A flap incision is used so that scalp blood flow is not compromised (the base cannot be too short, and remember that blood flow is coming from inferior to superior). A pedicle that is narrower than the width of the flap may result in the flap edges becoming gangrenous. A zigzag coronal incision (sometimes called a stealth incision) is used in craniosynostosis surgery to minimize the visibility of incisional scalp alopecia in children. A zigzag coronal incision also provides greater access to the anterior and posterior skull in craniosynostosis surgery.
89. What is the technique for placing a ventriculoatrial (ventriculovenous) shunt?
An incision is made across the anterior border of the sternomastoid muscle, and the jugular vein is identified. The vein is tied off distally and a small opening made into the jugular vein to pass the shunt down the jugular vein into the right atrium of the heart. Using electrocardiographic monitoring, the atrium is indicated by the P wave configuration becoming more and more upright, and when it becomes a biphasic P wave the tip has just entered the atrium, which is the optimal placement. Intraoperative fluoroscopy is used to confirm that the catheter is at the T6 level. Shunt nephritis is a complication of vascular shunts.55
90. What is the technique for inserting a ventriculopleural shunt?
An incision is made between the second and third ribs lateral to the midclavicular plane, and the tubing is inserted after puncture of the parietal pleura.
91. During posterior fossa surgery, brisk venous bleeding occurs on midline dural opening. What is the source of the bleeding and what can be done to stop it?
The circular sinus can bleed during posterior fossa decompression. This bleeding is best controlled with hemostatic clips.
92. What are the landmarks and trajectory for frontal ventriculostomy or shunt placement? Occipital ventriculostomy or shunt placement?
A frontal burr hole is best placed 10 cm from the nasion and 3 cm right of midline (unless there is a reason not to cannulate the right lateral ventricle). It is best to aim the catheter midway between the lateral orbital rim and the tragus, in the direction of the medial canthus. Aiming directly at the tragus places the end of the catheter at the 3rd ventricle. For frontal cannulation, 6 cm of catheter is inserted below the dura. For an occipital approach, select the point 7 cm above the inion and 3 cm to the right of the midline (unless there is a reason not to cannulate from the right). With this trajectory, the catheter is aimed 1 cm above the nasion. For the occipital approach, 10 cm of catheter is used; however, it is best to measure the exact distance needed on the preoperative CT scan. Occipital catheter placement may have a lesser chance of seizure disorder and better cosmesis than a frontal catheter.56
 Operative Anatomy
Operative Anatomy
93. What bones form the hard palate?
The anterior part is formed by the maxilla and the palatine bones form the posterior part.
94. What veins are connected at the torcula?
The superior sagittal sinus, transverse sinus, straight sinus, and occipital sinus
95. What bones form the zygomatic arch?
The anterior part is formed by the zygoma and the posterior part is formed by the squamosal part of the temporal bone.
96. What bones form the nasal septum?
The perpendicular plate of the ethmoid and the vomer
97. What bones form the clivus?
The sphenoid bone and occipital bone
98. What nerve carries parasympathetic innervation of the parotid gland?
The auriculotemporal nerve
99. Which cerebellar peduncle carries only afferent fibers?
The middle cerebellar peduncle
100. Which thalamic veins join the thalamostriate vein?
None of them—despite its name
101. The superior orbital fissure provides a communication between what two areas?
The orbit and the middle fossa
102. The lamina terminalis extends upward from the optic chiasm and blends into what structure?
The rostrum of the corpus callosum57
103. What cistern is contained in the posterior incisural space?
The quadrigeminal cistern
104. The lateral and medial posterior choroidal arteries are branches of which circle of Willis artery?
The posterior cerebral artery
105. How does CSF secreted from the choroid plexus enter the subarachnoid space?
Via the fourth ventricular foramina of Magendie and Luschka
106. What is the rate of CSF formation?
About 500 mL per day (or 0.33 mL per minute) under normal conditions58
107. What is the normal diameter of the supraclinoid ICA?
4–5 mm59
108. What ligament does the abducens nerve pass under?
The petrosphenoid ligament
109. Where does the basal vein originate and through which cisterns does it pass?
The basal vein originates on the surface of the anterior perforated substance and it courses through the crural and ambient cisterns to reach the quadrigeminal cistern and join with the internal cerebral vein.
110. What is the most medial structure in the cavernous sinus?
The internal carotid artery60
111. What are the 10 anatomic triangles identified near the cavernous sinus?
The 10 triangles in the cavernous sinus area can be grouped into three regions with the triangles grouped as follows (Fig. 5.4):60
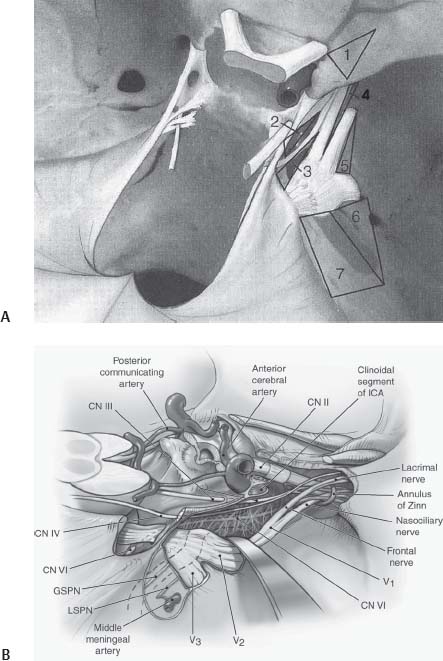
Fig. 5.4 (A) Triangles of the cavernous sinus. 1, Anteromedial; 2, paramedian; 3, Parkinson; 4, anterolateral; 5, lateral; 6, Glasscock (posterolateral); 7, Kawase (posteromedial). (B) Surgical anatomy of the cavernous sinus and basal region. GSPN, greater superficial petrosal nerve; LSPN, lesser superficial petrosal nerve; ICA, internal carotid artery. ([A] Reprinted with permission from Badie, p. 13640; [B] Reprinted with permission from Sekhar & Fessler, p. 63446)
1. The parasellar region
• The anteromedial triangles
• The paramedian triangles
• The oculomotor triangles
• The Parkinson triangles
2. The middle cranial fossa area
• The anterolateral triangles
• The lateral triangles
• The posterolateral (Glasscock) triangles
• The posteromedial (Kawase) triangles
3. The paraclival region
• The inferomedial triangles
• The inferolateral (trigeminal) triangles
 Preoperative Assessment
Preoperative Assessment
112. What is the most common side effect of mannitol?
Renal failure
113. When do the majority of perioperative myocardial infarctions occur?
Between postoperative days 3 and 5
114. What is the best method in current use to assess cerebral metabolism quantitatively?
Positron emission tomography (PET)
115. Why are inhalational anesthetics referred to as “uncoupling” agents with respect to cerebral hemodynamics and metabolism?
They decrease cerebral metabolism, but increase cerebral blood flow through vasodilatation. If an inhalational agent is to be given to a patient with poor intracranial compliance, hyperventilation should be initiated prior to induction. Isoflurane has less of an effect on cerebral blood flow than other agents.38,61
116. When should the use of nimodipine in vasospasm be reconsidered?
In the face of diminished cardiac contractility, use of nimodipine (which is a negative inotrope) may exacerbate the cardiac complications.
117. What should be considered in the evaluation of a patient who is scheduled for an elective craniotomy for meningioma who is hyponatremic and hypotensive, but otherwise healthy?
Adrenal insufficiency
118. What types of coagulopathies are not detected by prothrombin time/partial thromboplastin time/international normalized ratio (PT/PTT/INR) and platelet counts?
Dysfibrinogenemia, von Willebrand disease, factor XIII deficiency, aspirin/Plavix use
119. What disorders can lead to platelet sequestration?
Hypersplenism associated with cirrhosis, Gaucher disease, sarcoidosis
120. In what patient population does steroid use increase the risk of gastrointestinal hemorrhage?
Patients with preexisting ulcer disease
121. Oxygen transport is maximal when hematocrit is in what range?
30–32%
122. What finding on a CT scan of the head would be predictive of the success of a third ventriculostomy for hydrocephalus?
Triventricular hydrocephalus (or obstructive hydrocephalus) from aqueductal stenosis or blockage of third ventricular outflow62
123. What are the basic types of morphology of cerebral aneurysms?
Saccular, dissecting, and fusiform. The morphology of the aneurysm influences surgical and/or endovascular treatment.
Trauma and Emergencies
 Trauma
Trauma
124. What is the most common cause of subarachnoid hemorrhage (SAH)?
Head trauma63
125. What is the most common cause of cerebrospinal fluid leakage?
Head trauma; having a skull fracture doubles the patient’s risk of a cerebrospinal fluid leak. Cerebrospinal fluid leaks may occur from the nose (rhinorrhea), ear (otorrhea), or orbit (mimicking tears).63
126. How can one differentiate if nasal drainage is CSF or nasal secretion?
The primary distinction between CSF and nasal drainage is the glucose level. Glucose is present in CSF (at 50% of the serum level) and not present in nasal drainage. A protein level of less than 1 g per liter is suggestive of CSF. The double-ring sign (“halo signrdquo;) seen on the bed sheets or clothing of patients with nasal drainage is only suggestive of a CSF leak; the β2-transferrin test can confirm the presence of CSF.64
127. What is the best initial treatment for a CSF leak?
Bed rest and head elevation. Most leaks stop within 3 days. If after 3 days the leak persists, lumbar drainage may be used. Rarely is surgery needed to repair the source of the leak. The use of prophylactic antibiotics is controversial and may select for more virulent bacteria should infection occur.64
128. What is the major cause of spontaneous intracranial hypotension?
Spontaneous CSF leaks. Diffuse pachymeningeal enhancement on magnetic resonance imaging (MRI) is the most common imaging finding. Patients often complain of headache that is alleviated by lying flat. A CT myelogram or radionucleotide cisternogram may be used to find the leak site.64
129. What are the areas most prone to diffuse axonal injury after head trauma?
Corpus callosum and superior cerebellar peduncle65
130. What is the microscopic hallmark of diffuse axonal injury?
Axonal retraction balls, which are eosinophilic globular swellings at the proximal and distal sites of disrupted axons. They are formed by axoplasm and driven by altered axoplasmic transport.65
131. Regarding bullet wounds to the skull, which site is typically smaller, the entrance or exit wound?
In through and through missile wounds to the skull, the entrance wound is typically smaller.
132. What radiologic view is necessary to fully appreciate an occipital bone fracture on plain x-ray films?
The Towne view66
133. Which allele predisposes one to greater risk of Alzheimer disease after a head injury?
Apolipoprotein E4 (APOE4)
134. What area of the intracranial facial nerve is most commonly damaged by blunt trauma?
The area of the facial nerve around the geniculate ganglion67
135. What is the Schirmer test?
This test distinguishes facial nerve injuries proximal and distal to the geniculate ganglion. The test involves placing a narrow strip of thin paper on the conjunctiva to assess for lacrimation. Injuries proximal to the geniculate ganglion tend to produce a dry eye, whereas injuries distal to the ganglion do not interfere with lacrimation. Whether the location of the facial nerve injury is proximal or distal to the geniculate ganglion is important because the choice of surgical approach differs with different sites of injury.68
136. What type of temporal bone fractures more frequently result in external manifestations such as otorrhea of CSF and tympanic membrane perforation?
Longitudinal fractures more frequently result in external signs of injury, whereas transverse fractures generally spare the middle ear, tympanic membrane, and external auditory canal. For this reason, transverse fractures manifest fewer external signs of injury. Transverse fractures most commonly pass through the otic capsule; longitudinal fractures typically spare the otic capsule.67
137. Why is an EEG sometimes ordered in cases of lowered level of consciousness posttrauma?
To rule out subclinical status epilepticus69
138. What range of cerebral perfusion pressures are accommodated by cerebral autoregulation?
60–160 mm Hg70
139. How does one calculate cerebral perfusion pressure?
Cerebral perfusion pressure equals the mean arterial pressure minus the intracranial pressure (CPP = MAP—ICP).71
140. CPP should be maintained above what number after a severe head injury?
70 mm Hg71
141. How does one calculate MAP?
MAP is twice the diastolic pressure, which is added to the systolic pressure; then all are divided by three. MAP = ((2D) + S)/ 3). It is two times the diastolic because the majority of the cardiac cycle is in diastole.71
142. At what blood flow rate does electrical activity of the cerebral cortex fail?
About 20 mL/100 g/min71
143. What brainstem reflexes are mandatory to test in performing brain death evaluation?
Pupil reflex, corneal reflex, oculovestibular reflex, oculocephalic reflex, gag reflex. Additional tests that should be performed are checking for a response to deep central pain and the apnea test. The patient should be checked for normothermia and normal blood pressure, and show no evidence of drug or metabolic intoxication.72
144. In using auditory evoked potentials in the evaluation of brain death, what wave is necessary for the test to be valid?
Wave I, at least on one side72
145. What are some medications that are neuroprotective?
Corticosteroids, free-radical scavengers, calcium channel blockers, glutamate antagonists, mannitol, and barbiturates
146. A trauma patient with a broken leg is neurologically stable, but deteriorates after manipulation of his broken leg by the orthopedic service on hospital day 5. What is the most likely cause of the deterioration in this patient?
Fat emboli syndrome
147. Why is a bifrontal exposure often needed in trauma cases for persistent rhinorrhea?
Fractures of the anterior fossa often extend across the midline
148. What does the literature state about prophylactic antibiotics for CSF leaks after traumatic head injury?
An article in Lancet (1994) states that the use of prophylactic antibiotics only encourage the resistance and late attacks of meningitis; therefore, they are not recommended.73
149. What does the literature state about hyperventilation in the setting of traumatic brain injury?
Hyperventilation of head-injured patients may do more harm than good by decreasing cerebral perfusion pressure and delivery of O2 and glucose. There are no good prospective, randomized studies to date to support the use of hyperventilation in head injury.74
150. What is a possible diagnosis of a young adult with a family history of migraines who presents to the emergency room after head trauma and complains of blindness?
Trauma-triggered migraine with transient cortical blindness74
151. How can an acute subdural hematoma appear isointense to brain in a multitrauma patient?
When the hematocrit is less than ~23, this may cause an acute subdural to appear isointense to brain. Another possibility is in the setting of coagulopathy.75
152. Why are epidural hematomas more frequently seen in younger adults than in the elderly?
The dura is thinner and more adherent to the skull in the elderly. This decreases the ease with which the dura tears in relation to an overlying skull fracture. Epidural hematomas are much more common in children and young adults than in the elderly, probably because of the flexibility of the skull and the readiness with which the dura strips off the bone (Fig. 5.5).
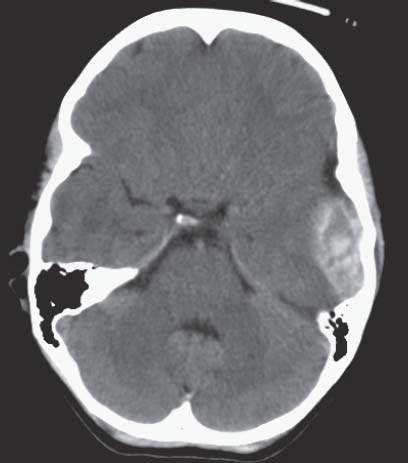
Fig. 5.5 CT scan without contrast showing epidural hematoma in a pediatric patient. Note the early uncal herniation.
153. How are epidural hematomas different in children and adults?
In children, epidural hematomas are caused by venous bleeding more often than in adults (where the usual culprit is the middle meningeal artery). In retrospective studies, it is therefore not surprising that 60% of children and 85% of infants with epidural hematomas had no disturbance of consciousness at the time of injury.76
154. Barbiturates are the most common class of drugs used to suppress cerebral metabolism in the setting of major cerebral trauma. What is the typical dosage of pentobarbital and what tests can be used to make sure the right amount is given?
A loading dose of 10 mg/kg is administered over 30 minutes then 5 mg/kg per hour is administered over 3 hours. If systolic blood pressure drops by more than 10 mm Hg or the perfusion pressure falls below 60 mm Hg, the loading dose infusion should be slowed. A maintenance infusion of 1 to 3 mg/kg per hour is begun after loading is completed. The infusion is titrated to burst suppression on the electroencephalogram and a serum level of 3 to 4 mg/dL. When checking for brain death, remember that the level of pentobarbital must be less than 10 μg/mL.74
155. Where on the carotid artery is the most common location for a traumatic aneurysm?
Most traumatic aneurysms of the carotid artery are located on the segment between the proximal and distal dural rings. They are pseudoaneurysms that may project medially into the sphenoid sinus. They may present with the classic triad of head injury with basal skull fracture, unilateral visual loss, and epistaxis.77
156. What are some shortcomings of the Glasgow Coma Scale (GCS)?
It does not allow the assessment of eye opening in periorbital trauma, verbal response in intubated patients, and brainstem function or reflexes. The GCS also works poorly for patients in the first 2 years of life. The GCS, however, remains the standard for defining the level of consciousness after head injury and is a reliable and independent predictor of long-term outcome. The GCS is also used for patients who have not sustained trauma, such as postoperative patients.
157. Finding a linear skull fracture on radiologic exams in a conscious patient increases the risk of intracranial hematoma by how much?
400-fold according to a study by Mendelow et al78
158. What is the definition of an “early” posttraumatic seizure? A “late” posttraumatic seizure?
An early posttraumatic seizure is one that occurs within the first 7 days of an injury; those that come after 7 days are called late posttraumatic seizures. About 10% of adults with early seizures will develop status epilepticus. Prophylactic phenytoin therapy may be stopped in ~1 to 2 weeks to prevent early posttraumatic seizures; however, there is no proven advantage that phenytoin or other anticonvulsants prevent late posttraumatic seizures.
159. What is the preferred method of intubation in a patient with a basal skull fracture?
Orotracheal intubation. There is a possibility of entering the cranium through the cribriform plate with a nasotracheal intubation.
160. What are the prerequisites for a growing skull fracture?74
1. The skull fracture occurs in infancy or early childhood.
2. There is a dural tear at the time of the fracture.
3. There is brain injury at the time of the fracture with displacement of leptomeninges and possibly brain through the dural defect.
4. There is subsequent enlargement of the fracture to form a cranial defect.
 Emergencies
Emergencies
161. A fall in end tidal CO2 could be the only clue to what emergency?
Air embolus
162. How is air embolism treated?
Packing the wound with wet sponges, lowering the patient’s head, using jugular venous compression, rotating the patient’s left side downward, aspirating from the venous line that is in the right atrium, and ventilating the patient while maintaining adequate blood pressure and heart rate
163. What are some cases where hyperemia of the brain can occur?
Head trauma, after carotid endarterectomy or stenting, and after excision of an arteriovenous malformation (AVM)
164. How is the diagnosis of disseminated intravascular coagulation (DIC) confirmed?
Low platelet count, prolonged PT, elevated fibrin degradation products, and reduced fibrinogen levels
165. What is the treatment of a cluster headache in a patient who is in excruciating pain?
Oxygen, sumatriptan, or a combination of both. Restlessness and agitated behavior are reported symptoms in 93% of cluster headache patients.
166. Which drug is best in the immediate control of seizures in status epilepticus?
Lorazepam is better than diazepam or phenytoin69
167. What is the treatment algorithm for status epilepticus?
Lorazepam 4 mg (or 0.1 mg/kg) intravenously (IV) over 2 minutes, may repeat after 5 minutes. Simultaneously load with phenytoin 1200 mg (or 20 mg/kg), or 500 mg if already on phenytoin. Phenobarbital may be given up to 1400 mg at a rate of less than 100 mg/min. If seizures continue, consider general anesthesia. It is also important in the initial stages of status to send laboratories for electrolyte levels and antiepileptic drug levels if the patient is already on an agent. A normal saline IV drip may be started and 50 mL of 50% glucose given, as well as 100 mg of thiamine. Other agents that may be used if the above measures are not effective include pentobarbital (while watching for circulatory depression and being prepared to use a pressor), midazolam, or propofol.69
168. What are the signs and symptoms of myxedema coma and how is it properly treated?
Myxedema coma is an emergency of hypothyroidism. The signs are hypotension, bradycardia, hyponatremia, hypoglycemia, hypothermia, and hypoventilation. Treatment consists of IV fluids, intubation if necessary, IV glucose, 400 mg hydrocortisone IV over 24 hours, and 0.5 mg levothyroxine IV followed by 0.05 mg levothyroxine per day.79
169. What are the three places that a shunt may be occluded?
The entry point (proximal occlusion), the valve system (valve obstruction), and the distal end (distal catheter occlusion). A CT scan of the head, a shunt series, and palpation of the valve are important in determining the site of the occlusion.
170. A patient with a prior history of pituitary tumor presents with a sudden onset of headache and rapid visual failure with extraocular nerve palsies. What is the most likely diagnosis and how is it treated acutely?
This is pituitary apoplexy, which can clinically mimic a SAH. Death may follow unless urgent steroid treatment is started.
171. How should life-threatening cerebellar swelling from infarction be managed (Fig. 5.6)?
Resection of cerebellar infarction has been advocated in patients in whom life-threatening deterioration is occurring from focal cerebellar swelling, herniation, and brainstem compression or secondary fourth ventricular obstruction and hydrocephalus. A ventriculostomy may be needed as a temporizing measure in anticipation of surgery; however, one must be cognizant of the risk of upward herniation.
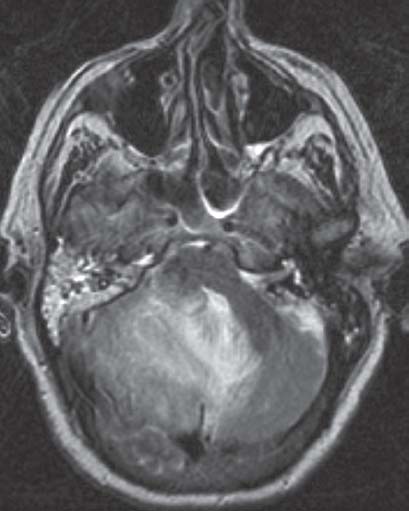
Fig. 5.6 Life-threatening cerebellar swelling from right cerebellar hemisphere infarction.
172. What are the drugs used in neuroleptic malignant syndrome?
Bromocriptine (dopamine receptor agonist) and dantrolene (muscle relaxant). Neuroleptic malignant syndrome is a rare condition seen with dopamine antagonist and long-acting depot neuroleptic preparations. Drowsiness, fever, tremor, and rigidity occur suddenly.
173. What is the most common cerebral vascular complication encountered during pregnancy?
Subarachnoid hemorrhage is the most common cerebral vascular complication encountered during pregnancy. The risk of rupture parallels the hemodynamic changes, reaching an apex in the third trimester, in concert with blood volume changes. Aneurysms are most prone to rupture during the seventh and eighth months of pregnancy and at delivery.80
174. What is the most common site of hypertensive cerebral hemorrhage?
The putamen
175. What are the signs and symptoms of Addisonian crisis and how is it properly treated?
Addisonian crisis is an adrenal insufficiency emergency with symptoms of mental status changes and muscle weakness. Signs of postural hypotension, shock, hyponatremia, hyperkalemia, hypoglycemia, and hyperthermia may be seen. For a glucocorticoid emergency, administer 100 mg IV hydrocortisone (Solu-Cortef; Pfizer Pharmaceuticals, New York, NY) immediately (STAT) and then 50 mg IV every 6 hours. Concurrently, one should also give cortisone acetate 75 to 100 mg intramuscularly (IM) STAT, and then 50 mg IM every 6 hours. For a mineralocorticoid emergency, it is best to give desoxycorticosterone acetate 5 mg IM twice daily.81
176. What is central pontine myelinolysis?
A rare disorder of pontine white matter producing insidious flaccid quadriplegia and mental status changes. This disorder results from correcting hyponatremia too rapidly; Na+ should be corrected no faster than 10 mEq/L in 24 hours.
177. What is neurogenic pulmonary edema?
Neurogenic pulmonary edema is associated with SAH, head trauma, and seizure disorder. It is caused by an increased capillary permeability in the lungs associated with an increased in sympathetic discharge. Treatment is aimed at reducing ICP, maintaining positive pressure ventilation, and supportive care.
178. How is an acute attack of migraine headache best treated?
Prochlorperazine (Compazine; Brentford, Middlesex, UK) 10 mg IV
179. What potential emergency can occur intracranially if nitrous oxide anesthesia is not discontinued prior to closure of the dura during surgery?
Tension pneumocephalus
180. What are the most common complications of the transoral operative route?
CSF leakage and infection
Neoplasms
181. What is the name of a cystic tumor of the suprasellar region that arises from neuroectodermal remnants of Rathke pouch?
Craniopharyngioma (Fig. 5.7)82

Fig. 5.7 Coronal T1-weighted magnetic resonance image with contrast demonstrating a craniopharyngioma with suprasellar cystic extension.
182. What preoperative medication can lessen general and cardiac risks in patients with a growth hormone (GH) secreting tumor?
Somatostatin analogue83
183. Which type of lesion can present with calcification in the sella area and erode through the posterior clinoids?
Craniopharyngioma. Erosion of the posterior clinoids may also occur from chronic increases in ICP for a variety of reasons.82
184. What type of tumor can erode the internal acoustic meatus? The petrous apex? The clivus? The sellar floor? The orbital foramen? The jugular foramen?
Internal acoustic meatus: An acoustic schwannoma
Petrous apex: A trigeminal schwannoma
Clivus: A chordoma
Sellar floor: Large pituitary tumors
Orbital foramen: An optic nerve glioma
Jugular foramen (the bone): A glomus jugulare tumor
Also note that an aneurysm may erode through bone, such as an aneurysm eroding through the sphenoid sinus presenting with epistaxis.84
185. What disease may produce generalized bone erosion? Generalized hyperostosis?
Multiple myeloma produces generalized bone erosion. Paget disease usually results in generalized hyperostosis. Recall that a meningioma results in focal hyperostosis.84
186. What is the most common extradural neoplasm involving the clivus?
A chordoma (Fig. 5.8). The two subgroups of chordoma are the typical and the chondroid; it is suggested in the literature that chondroid features portend a better prognosis.84
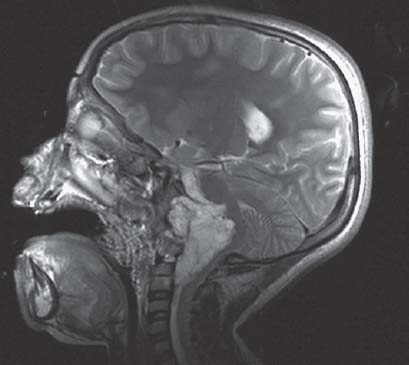
Fig. 5.8 Sagittal T2-weighted magnetic resonance image demonstrating a clival chordoma with severe brainstem compression.
187. What is the immunohistochemical staining profile of a chordoma versus a chondrosarcoma?
Chordomas virtually always stain positive for keratin with variable S-100 expressivity. Chondrosarcomas lack epithelial markers, but are nearly always positive for S-100.85
188. If chordomas are histologically benign, what features make this lesion clinically malignant?
The malignant potential of a chordoma arises from the critical location at which these tumors arise as well as from their locally aggressive nature, high rate of recurrence, and occasional tendency to metastasize.86
189. What is the most common site of origin for chordoma?
The sacrum
190. What is the second most common site for chordoma?
The clivus
191. Prophylactic cranial irradiation may be considered part of the standard treatment of patients with what disease?
Small-cell lung carcinoma87
192. Which neurosurgical lesion is currently most commonly removed by endoscopic methods?
A colloid cyst (Fig. 5.9)
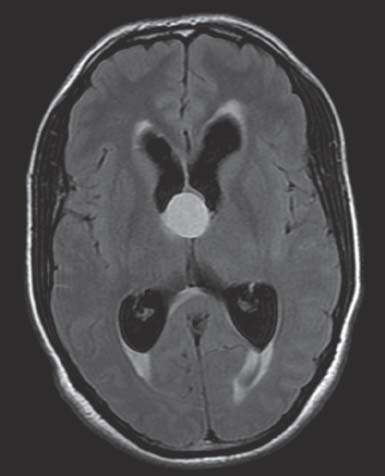
Fig. 5.9 Axial fluid-attenuated inversion recovery (FLAIR) magnetic resonance image demonstrating a colloid cyst of the 3rd ventricle.
193. Where are colloid cysts found?
The anterior roof of the 3rd ventricle88
194. How do colloid cysts cause death?
They cause obstructive hydrocephalus that if left untreated may lead to death.89
195. What is the most common intraorbital tumor found in adults?
A cavernous hemangioma. These are benign, slow-growing vascular lesions. They can manifest as a painless, progressively proptotic eye. They are mostly unilateral, but bilateral cases have been reported. No predilection exists for race or ethnicity.90
196. What is the second most common type of intracranial schwannoma?
A trigeminal schwannoma (the vestibular type is the most common)
197. What is the most common presentation of a choroid plexus tumor?
Intracranial hypertension91
198. What are the differences in location of a choroid plexus papilloma between an adult and a child?
Choroid plexus papillomas are rare benign tumors of the central nervous system (CNS) that occur mostly in children and have a slight male predominance. These tumors are usually found in the left lateral ventricle in children (Fig. 5.10) and the 4th ventricle in adults. They account for less than 1% of all intracranial tumors.84
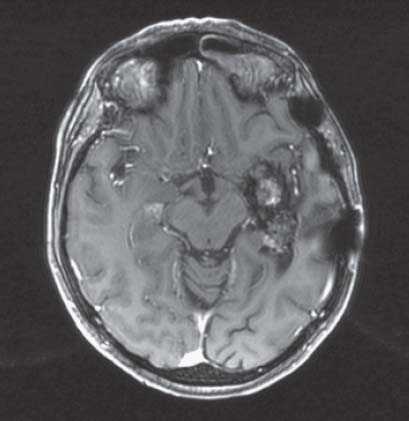
Fig. 5.10 Axial T1-weighted magnetic resonance image with contrast demonstrating a choroid plexus papilloma of the left temporal horn.
199. How can a surgeon differentiate tumor from radiation necrosis?
PET, single photon emission computed tomography (SPECT) and/or biopsy84
200. What type of histochemical stain do pathologists use to differentiate collagen from glial tissue?
Trichrome92
201. What is the median survival time for malignant glioma?
9 months
202. What is the significance of elevated choline peaks and reduced N-acetyl-aspartate (NAA) levels in spectroscopic evaluation of brain tumors?
Increased choline levels indicate increased membrane turnover. NAA (which reflects neuronal integrity) is reduced in tumors. The combination of both of these findings indicates tumor infiltration (Fig. 5.11).93
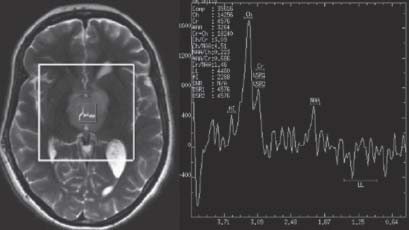
Fig. 5.11 Magnetic resonance spectroscopy of thalamic infiltrating glioma showing elevated choline peak and reduced NAA peak.
203. What are the prognoses for midbrain, medullary, and pontine gliomas?
Survival rates are best for midbrain and worst for pontine gliomas. Medullary gliomas are intermediate.
204. What CSF tumor marker is positive in germinomas?
Placental alkaline phosphatase94
205. Which pineal region tumor is most sensitive to radiation?
A germinoma95
206. What serum marker should you look for in a patient with a pineal region tumor?
β-Human chorionic gonadotropin (HCG) and a-fetal protein (AFP) because these neoplasms are of germ cell origin. β-HCG is elevated in choriocarcinomas. AFP is elevated in embryonal carcinomas and yolk sac tumors.
207. What tests can one perform to distinguish a primary tumor from a MS plaque when there is an enhancing lesion on MRI?
Visual evoked potentials, oligoclonal bands, and immunoglobulin G (IgG). The patient’s history is also important.30
208. What are the three most common focal brain lesions in human immunodeficiency virus (HIV)?
Toxoplasmosis, primary lymphoma, and progressive multifocal leukoencephalopathy (PML)
209. What cancer (CA) is sensitive to chemotherapy and radiation, usually never operated on, and exhibits paraneoplastic syndromes like syndrome of inappropriate antidiuretic hormone secretion (SIADH) or syndrome of ectopic adrenocorticotropic hormone (ACTH) production?
Small-cell lung CA
210. What modality can distinguish primary lymphoma of HIV from other focal mass lesions associated with HIV?
A fluorine-18 fluorodeoxyglucose (18-FDG) PET scan. Lymphomas have a higher uptake than toxoplasmosis or PML.96
211. What is the median survival of a child with a pontine tumor?
9–12 months
212. When is radiation therapy indicated in oligodendroglioma?
For anaplastic transformation. Chemotherapy is recommended for all cases of oligodendroglioma. Loss of 1p/19q predicts an almost 100% response rate to procarbazine, lomustine (CCNU), and vincristine (PCV) chemotherapy in oligodendroglial tumors.97
213. What is the preferred approach for a lesion situated entirely within the atrium of the ventricle?
Posterior transcortical approach directed through the superior parietal lobule98
214. What approaches are best suited for pineal region tumors?
Occipital transtentorial or infratentorial supracerebellar
215. What diagnostic test is recommended for a pediatric patient with a posterior fossa tumor?
MRI of the spine to rule out drop metastases
216. What are the survival rates of the four grades of gliomas?99
Grade I: 8 to 10 years
Grade II: 7 to 8 years
Grade III: ~2 years
Grade IV: <1 year
217. What is the role of surgery in primary CNS lymphoma?
No role for debulking, only biopsy if there is a question as to the lesion. Primary central nervous system lymphoma (PCNSL) may mimic a glioblastoma multiforme (GBM) radiographically.
218. What is Collins’ law?
Collins’ law (or rule) states that a congenital tumor may be considered cured if it does not recur within a period equal to the person’s age plus 9 months after surgery. This rule does have some exceptions and may be applicable ~80% of the time.100
219. What is the recurrence rate for benign meningiomas?
2–3% in 5 years101
220. Where do meningiomas arise from?
Arachnoid cap cells present in the arachnoid granulations (convexity meningiomas) and in the arachnoid layers of the meninges (for non-convexity meningiomas).102
221. What is the rate of malignant change of meningiomas?
1–2%101
222. How do meningiomas of the foramen magnum present?
Pyramidal weakness initially affecting the ipsilateral arm, followed by the ipsilateral leg, spreading to the contralateral limbs when the tumor enlarges103
223. What is the chromosomal abnormality found in meningiomas?
Over 70% of these tumors have monosomy 22104
224. What are the most common CNS locations of meningiomas?
Ninety percent are cranial, 9% are spinal. The most common intracranial locations in order of highest occurrence are parasagittal, convexity, sphenoid tuberculum, olfactory groove, foramen magnum, optic sheath, tentorial, and intraventricular.105
225. From where do convexity meningiomas derive their blood supply?
The external carotid artery branches
226. What bony skull abnormality is most often seen with meningiomas?
Hyperostoses. This is thought to occur because meningiomas secrete osteoblastic factors promoting bone growth.105
227. Which hormone receptors do meningiomas exhibit?
Progesterone and estrogen. This may explain why meningiomas are more common in women and why they tend to grow with pregnancy and breast CA.
228. What is Foster-Kennedy syndrome?
Optic atrophy in one eye and papilledema in the other eye with anosmia. This syndrome is sometimes seen with olfactory groove meningiomas.106
229. What is the median survival for an oligodendroglioma that enhances with gadolinium? That does not enhance?
The median survival from the initial diagnosis of all low-grade oligodendrogliomas is 4 to 10 years, but only 3 to 4 years for anaplastic oligodendrogliomas (those that enhance). Oligodendrogliomas are chemosensitive. Patients with anaplastic oligodendrogliomas who have a loss of heterozygosity on chromosome 1p or combined loss of heterozygosity on 1p and 19q survive substantially longer (~10 years) than patients who lack these genetic changes.107
230. When is the facial nerve encountered in the cerebellopontine (CP) angle during the resection of an acoustic neuroma? And during the resection of a CP angle meningioma?
In acoustic neuromas, the facial nerve lies anterosuperior to the tumor and is typically encountered late in surgery. In CP angle meningiomas, the facial nerve may lie at the posterior tumor edge and may be injured early in surgery unless it is identified.
231. Any patient younger than 40 years old with a unilateral acoustic neuroma should also be evaluated for what condition?
Neurofibromatosis type II (NF2)108
232. What do brainstem auditory evoked potentials show in a patient with acoustic schwannoma?
A delay of wave V latency on the affected side
233. What medication may shrink a neurosarcoid mass at the skull base?
A corticosteroid109
234. What laboratory tests can support the diagnosis of sarcoid?
Elevated serum and CSF angiotensin converting enzyme (ACE), elevated serum immunoglobulins, elevated serum calcium, and elevated CSF cell count (monocytes), IgG, Ig index, and presence of oligoclonal bands. Nervous system involvement occurs in ~8% of sarcoid patients. Sarcoid usually involves the meninges, skull base, cranial nerves, and pituitary stalk. Immunosuppression with corticosteroids is usually indicated and long-term therapy is required.109
235. What are some slow-growing, painless calvarial masses?
Osteoma, ossifying fibroma, chondroma, hemangioma, epidermoid, dermoid, meningioma, fibrous dysplasia, and nonossifying fibroma84
236. What is the most common primary skull neoplasm?
Osteoma110
237. Which malignancies are associated with neurofibromatosis type I (NF1)?
Malignant peripheral nerve sheath tumors (MPNSTs), pheochromocytoma, and leukemia111
238. What osseous lesion and condition are usually seen with NF1?
Sphenoid dysplasia and thinning of long bones112
239. What is the mode of inheritance of NF2?
Autosomal dominant on chromosome 22113
240. Where are chordomas found?
Almost all chordomas occur near the clivus or sacrum.114,115
241. What is the difference between an osteoid osteoma and an osteoblastoma?
Size. These are benign bone tumors. When the lesion is 2 cm or less, it is called an osteoid osteoma; if it is larger than 2 cm in size, it is referred to as an osteoblastoma.116
242. What is Gardner syndrome?
Gardner syndrome is characterized by intestinal polyposis with frequent malignant degeneration, benign soft tissue neoplasms, and multiple osteomas of the skull and mandible.110
243. What is the most common location for epidermoid tumors?
The cerebellopontine angle
244. What are some cerebral metastases in pediatric patients?
Neuroblastoma, rhabdomyosarcoma, and Wilm tumor
245. What are the radiosensitive cerebral metastases?
Small-cell lung CA, multiple myeloma, germinoma, lymphoma, and leukemia
246. Where do metastatic brain tumors appear?
At the gray–white junction
247. What are the most common hemorrhagic metastatic brain tumors?
In order of highest occurrence: lung, breast, renal cell carcinoma, choriocarcinoma, and melanoma
248. Which metastatic brain tumor is associated with the shortest life expectancy?
Melanoma117
249. Which brain lesion is associated with gelastic seizures?
Hypothalamic hamartomas118
250. Besides a brain MRI, which other diagnostic procedures are needed in a patient with an ependymoma?
A spinal MRI and a lumbar puncture (if not contraindicated).
251. What are the most common tumors of the jugular foramen?
Also called glomus jugulare tumors, paragangliomas are most common, followed by schwannomas and meningiomas. Paralysis of the lower CNs is often the initial symptom of tumors arising in the jugular foramen. In the case of a paraganglioma, patients may present with hearing loss, pulsatile tinnitus, and facial paralysis if the tumor is very large.119
252. What is the most common presenting sign of a glomus tumor?
Unilateral hearing loss due to invasion of the middle ear120
253. What is the most common vessel supplying a glomus jugulare tumor?
The ascending pharyngeal artery121
254. What laboratory studies should be done preoperatively in the workup of a glomus tumor? How would that affect perioperative management?
A 24-hour urine sample should be analyzed for vanillylmandelic acid, metanephrines, and catecholamines to determine the secretory status of the tumor. A secreting tumor would need to be managed with a blockers 2 weeks before surgery and with a β blocker the day before surgery to prevent a hypertension crisis.
255. What CNs are most commonly affected by the growth of a glomus jugulare tumor?
CNs IX, X, XI (those nerves that pass directly through the jugular foramen), CN VII (the facial nerve, usually along the mastoid segment), and CN XII (the hypoglossal nerve)122
256. What is the differential diagnosis for a cerebral ring-enhancing lesion?
Glioma, lymphoma, infection, demyelinating plaque, radiation necrosis, resolving hematoma, cysticercosis, sarcoid, or granulomatous disease84
257. What particular genetic alteration makes malignant gliomas chemoresponsive?
Loss of heterozygosity at 1p and 19p (mainly oligodendrogliomas)107
258. What do the terms “communicating” and “noncommunicating” refer to with hydrocephalus?
In communicating hydrocephalus, the ventricular system is in communication with the subarachnoid space of the brain and spinal cord; in the noncommunicating form, there is a block either within the ventricular system (i.e., tumor, blood) or in its outlets to the subarachnoid space, so that the ventricles and subarachnoid space are discontinuous.123
259. What are tumor markers and how can they help in diagnosing a brain tumor?
Tumor markers are substances found in the blood, urine, or body tissues that can be elevated in cancer, and are identified by immunohistochemical techniques. Identification of certain antigens specific for particular tumors help in the diagnosis of brain tumors.
• Glial fibrillary acidic protein (GFAP) is a marker for astrocytic tumors.
• S-100 has a similar distribution as GFAP, but is more localized in Schwann cells.
• Cytokeratin is a marker for metastatic carcinoma.
• Synaptophysin is a marker for neuronal tumors.
• HMB45 is a marker for malignant melanoma.
• Ki-67 is a marker of proliferation of various tumors.
• Loss of heterozygosity markers is often important in oligodendrogliomas (1p and 19q).
• AFP and human chorionic gonadotrophin are markers for yolk sac tumors and choriocarcinomas, respectively.94



