Cranial stab wounds are lower velocity and usually involve a smaller impact area than missile wounds. They can present their own specific difficulties including a relatively high risk for vascular injuries and a retained weapon embedded in the skull. The orbit is a common site for penetration into the cranial vault, especially in children. Knives are the most common weapon employed in cranial assaults, but objects as innocuous as a pencil or a sewing needle may penetrate the cranium (Fig. 72.1)
♦ Preoperative
- Careful assessment of the site of penetration, depth, and trajectory of stab wounds are important factors in determining the extent of damage to the brain.
- Do not attempt removal of a retained weapon until the scalp incision and bone flap are completed.
- Administration of tetanus vaccination
- Seizure prophylaxis, typically phenytoin or fosphenytoin load, 18 mg/kg
- Antibiotic prophylaxis with broad spectrum agent with good central nervous system penetration (e.g., ceftriaxone 1 to 2 g based on weight)
- Consider early angiography in all patients with penetrating stab wounds involving dural penetration as a result of the risk of traumatic intracranial aneurysm. Computed tomography–angiography at initial evaluation may also help determine injury to major arterial and venous vascular structures.
- Ophthalmologic consultation if cranial penetration is through the orbit
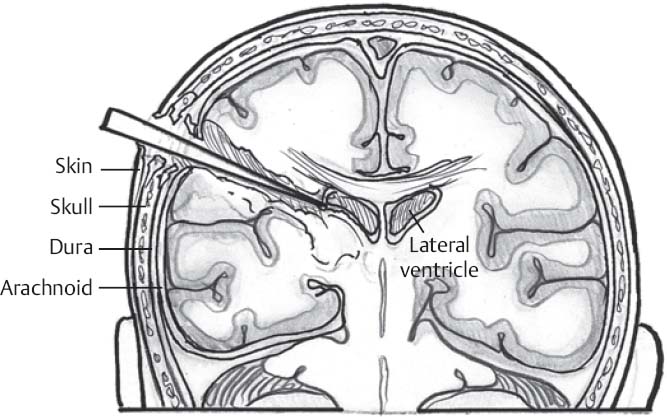
Fig. 72.1 Schematic illustrating a stab wound to the head with associated brain injury.
Operative Planning
- Goals of surgery are as follows:
- Débridement of devitalized tissue
- Removal of a retained weapon lodged in the skull
- Removal of hematoma causing mass effect
- Exclusion from the circulation of any traumatic intracranial aneurysms. Either surgical or endovascular options may be considered.
- Hemostasis
- Adequate closure of dura
- Meticulous closure of galea and scalp
- Débridement of devitalized tissue
- Placement of external ventricular drain or intraparenchymal intracranial pressure (ICP) monitor in patients with Glasgow Coma Scale (GCS) ≤ 8
Equipment
- Major craniotomy tray
- Foam headrest versus Mayfield pins
Anesthetic Issues
- Preparation for severe hemorrhage or disseminated intravascular coagulopathy with central venous access, arterial blood pressure monitoring, and readily available blood products
- Management of ICP and cranial perfusion pressure
♦ Intraoperative
Positioning
- Patient positioned supine with head on a foam headrest or Mayfield head holder with head turned to allow access to the surgical site. A shoulder roll may be placed to facilitate positioning.
- Occipital and suboccipital wounds may require placement in a prone position on bolsters or a Wilson frame and pinning in the Mayfield head holder.
- Head is elevated 15 to 20 degrees to facilitate venous drainage.
Planning of Shave and Preparation
- Hair is widely removed.
- Extracranial debris is flushed and removed from superficial aspects of wound.
- Preparation is completed in standard fashion.
Planning of Incision
- Strategies are based on nature of injury. Mass lesions with midline shift may require a large craniotomy flap.
- Localized injuries may allow for a limited flap encompassing the entry site.
- In localized injuries, scalp lacerations may be incorporated into a linear or curvilinear incision and then closed primarily after débridement. Care should be taken to preserve the vascular supply.
Bone Exposure
- For mass lesions with midline shift, a standard large frontotemporoparietal bone flap to allow for a large decompressive hemicraniectomy should be elevated.
- For localized lesions, wide exposure of the bony defect is essential. Additional bone should be removed to allow for visualization of intact dural edges.
- Bone edges should be débrided, and depressed fractures should be elevated. Bony fragments in the proximity of dural sinuses should be treated with extreme caution.
- Once the bone flap is completely removed, any retained weapon may be removed. The trajectory of removal must follow precisely that of the weapon’s entry to avoid further injury to the brain.
- Avoid use of electrocautery in the vicinity of a retained metal weapon to avoid heat transfer to the brain.
Débridement and Hemostasis
- The dural defect should be completely visualized. The wound tract should be extensively irrigated removing necrotic tissue and accessible bone fragments and foreign bodies.
- Removal of deeper fragments or foreign bodies is not recommended as this may injure potentially functional brain tissue.
- Provision for proximal and distal vascular control should be employed if a vascular lesion is suspected.
- Traumatic intracranial aneurysms often involve distal branches that may need to be trapped proximally and distally.
- Meticulous hemostasis of the wound tract should be obtained with bipolar cautery. Hemostatic agents left in the cavity should be minimized to reduce the infection risk, given the foreign body contamination.
Closure
- Primary dural closure should be attempted. When primary dural closure is not possible, autologous grafts such as temporalis fascia, pericranium, or fascia lata are recommended to minimize infectious risk.
- The bone should not be replaced in instances of diffuse brain swelling.
- The temporalis fascia should be approximated.
- Meticulous closure of the galea is crucial for preventing possible cerebrospinal fluid leakage and minimizing infectious risk.
- Devitalized scalp edges should be débrided.
- Skin edges of simple wounds may be reapproximated with staples.
- More complex wounds will require closure with nylon suture.
- The temporalis fascia should be approximated.
Postoperative
- An external ventricular drain or intraparenchymal ICP monitor should be placed in all patients with a GCS ≤ 8 (see indications for ICP monitoring).
- Advanced neuromonitoring (brain tissue oxygen, jugular venous saturation, cerebral blood flow) should also be considered.
- Seizure prophylaxis is indicated for at least 7 days.
- Postoperative antibiotic coverage is indicated. The optimal duration of postoperative antibiotic coverage following cranial stab wounds is unconfirmed.
< div class='tao-gold-member'>







