26 | Cranicervical Injuries |
 | Case Presentation |
History and Physical Examination
A 79-year-old male was airlifted from an outside facility after being found at the bottom of an elevator shaft asystolic and with head lacerations. He had been resuscitated at the outside facility but, given his history and constellation of injuries, he was airlifted to our level I trauma center. He had been transferred intubated but reportedly had been moving his upper extremities. The lateral radiograph of his C-spine on arrival (Fig. 26–1) showed posterior translation of his head relative to the cervical spine, a C1 fracture, and degenerative changes of the lower C-spine. He was intermittently moving his upper extremities purposefully and was noted to grimace with painful stimuli. No detailed neurological exam could be obtained given the patient’s sedated status.

Figure 26–1 Lateral trauma radiograph taken upon arrival to the emergency room in a 79-year-old male with atlanto-occipital dissociation. Note the posterior translation of the clivus in relationship to the dens.
The patient was taken for computed tomography (CT) and magnetic resonance imaging (MRI) of his cervical spine after initial stabilization and then taken to the intensive care unit for further care. He was not cleared by the general surgeons and intensivists for surgical management until 3 days after his admission.
Radiological Findings
Emergency room (ER) CT scan demonstrated on sagittally reformatted views the clivus to be 13 mm posteriorly translated relative to the dens. On sagittal and coronal reformats, obvious occipital-C1 joint disruption in conjunction with a C1 Jefferson fracture was seen (Fig. 26–2).
His MRI showed a significantly displaced C1 Jefferson fracture with 14 mm of anterior displacement of the tip of the dens in relation to the basion and high signal in the occipital-C1 joints consistent with an atlanto-occipital dissociation. There was no evidence of high signal within the cord to suggest a cord injury (Fig. 26–3A,B).
Diagnosis
This patient had a traumatic atlanto-occipital dissociation combined with a type 3 occipital condyle fracture and atlas bursting type fracture, an injury constellation that falls into the larger category of craniocervical dissociation. These are extremely unstable injuries and have a very high mortality rate. It is imperative that an early diagnosis be made and the patient’s spine be carefully protected to avoid any spinal cord damage.
This patient was placed in a halo in the ER to stabilize his neck and protect him for transfers. It is important that the head is “pushed” into the body while the halo is tightened to compress the head onto the shoulders. It should be pointed out that a halo vest is a highly insufficient means of sustaining a compressive effect on the craniocervical junction. Of all the other temporizing alternatives this, however, remains preferable to other external immobilization attempts. In the case of a halo ring being contraindicated or not desirable the patient’s head may be sandbagged and taped down until definitive care can be rendered. A neck collar is usually highly undesirable due to a distractive effect of such a device. It should be very clearly emphasized that any patient with craniocervical dissociation is at very high risk of secondary neurological deterioration until definitive care is rendered.
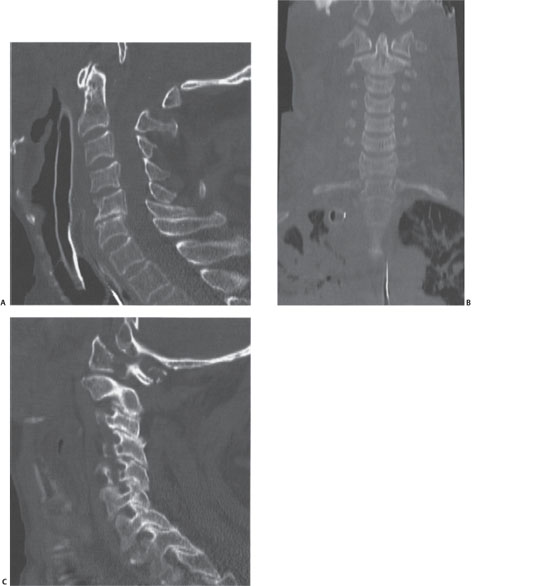
Figure 26–2 (A) Sagittal reformat in computed tomographic (CT) C-spine demonstrating posterior translation of the occiput in relation to the C-spine with posterior position of the clivus with respect to the dens. (B) Coronal reformat in CT C-spine demonstrating subluxation of the occiput-C1, particularly on the left. (C) Sagittal reformat in CT C-spine demonstrating malreduced occiput-C1 consistent with atlanto-occipital dissociation.
When the patient in question was cleared for surgery on postinjury day 3, he was transferred onto the Jackson table in a supine transfer under full spine precautions. His halo vest was then removed and baseline somatosensory evoked potentials (SEPs) and motor evoked potentials (MEPs) were recorded. Using the turning mechanism of the Jackson table with a halo ring attachment the patient was turned into a prone position. C-arm fluoroscopy was on standby and was brought into a lateral trajectory at the earliest point in time upon completion of prone positioning to ensure the best possible craniocervical alignment. Repeat SEPs and MEPs were checked. In the case of deterioration of preturning signals the patient would have been turned back into the supine position for reevaluation.
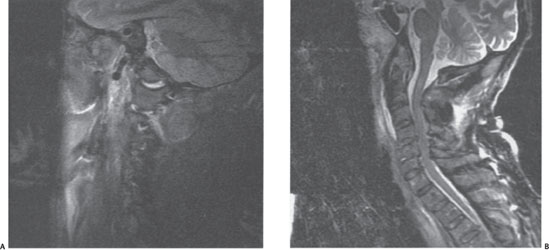
Figure 26–3 (A) Sagittal image in Short-tau inversion recovery (STIR) magnetic resonance imaging (MRI) demonstrating increased signal at the occiput-C1 joint suggestive of atlanto-occipital dissociation and joint injury. (B) Sagittal T2-weighted MRI at midline showing a relatively benign-appearing cord but lower C-spine baseline stenosis and degeneration.
After prepping and draping the posterior neck and occiput, midline exposure from the basion to C4 was performed. A top-loading plate-rod system allowing for a segmental fixation system was molded and pedicle screws were placed at C2, with lateral mass screws placed at C3. The plates were deviated toward the midline to take advantage of increased midline skull thickness (Fig. 26–4). Structural allograft and iliac crest graft for facet arthrodesis was used to achieve fusion. After closing the wound, the patient was placed in a hard collar and freely mobilized. A postop CT scan was obtained to check the final implant placement and reduction (Fig. 26–5). Final radiographs showed anatomical reduction was maintained with upright positioning (Fig. 26–6).
 | Background |
The craniocervical junction represents the most mobile region of the human spine with relatively fragile osteoligamentous components providing structural support.1,2 This results in craniocervical junction injuries accounting for almost one quarter of all cervical spine injuries.3 The relative frailty of the upper cervical spine is also reflected in the consistent findings in several autopsy studies of up to 90% of traumatic fatalities having injuries to the upper cervical spine.4–6
Although bony injuries in the upper cervical spine constitute relatively well understood entities from a diagnostic and treatment perspective, more complex injuries involving the occipital condyles and the ligamentous support structures of the upper cervical spine remain more obscure due to their lower incidence, highly variable injury severity, and occasionally daunting management challenges. The age range of patients with craniocervical trauma extends from young children typically injured during high-speed deceleration trauma to elderly patients presenting with low-impact injury mechanisms along with medical comorbidities.7 With improved medical care patients can survive even severe upper cervical spine injuries. Despite these medical advances craniocervical injuries of all severity grades are relatively easily missed due to a variety of circumstances. Low suspicion in patients presenting with multiple comorbidities, distractions caused by concurrent life-threatening injuries, and lack of familiarity with screening parameters of the craniocervical junction all contribute to missed injuries, which disproportionately affect the upper cervical spine.7–9 With its lack of inherent stability a delay in diagnosis of high-grade injuries to the craniocervical junction, however, can have potentially devastating consequences. As a result, systematic implementation of effective clinical and radiographic screening parameters can reduce the incidence of missed injuries.9
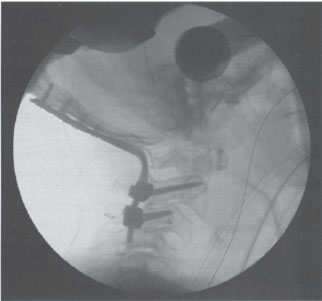
Figure 26–4 Intraoperative lateral fluoroscopy image showing anatomical reduction of atlanto-occipital dissociation and occiput to C3 fixation with a plate-rod construct in top-loading screws.
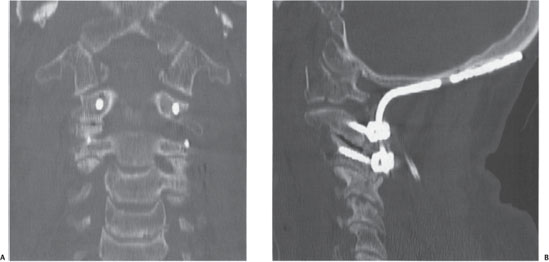
Figure 26–5 (A) Postoperative coronal computed tomographic (CT) scan demonstrating a reduced occiput-C1 joint after occiput screws, C2 pedicle screws, and C3 lateral mass screws. (B) Postoperative sagittal CT scan demonstrating reduced occiput-C1 joints.
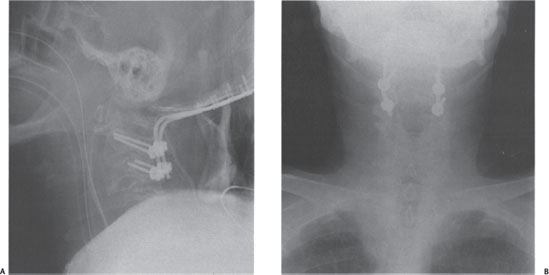
Figure 26–6 (A) Lateral postoperative upright radiograph demonstrating anatomical alignment. (B) Anteroposterior postoperative upright radiograph demonstrating C2 pedicle screws and C3 lateral mass screws with occipital plate.
The upper cervical spine forms a functional unit from the skull base through the axis, which allows for a significant range of motion at the cost of limited inherent biomechanical stability. The mass of the cranium attached to the rostral end of the very mobile yet relatively smallish upper cervical spine poses a significant load on the relatively frail ligaments of this transition region.1,10,11 Fortunately, the relatively capacious spinal canal affords the spinal cord some leeway in regard to spinal cord injury. The upper cervical spine also provides a conduit for the arterial supply to the cranium. Although clinically relevant arterial injuries due to craniocervical fractures are fortunately relatively rare, increasing availability of noninvasive diagnostic modalities has increased awareness of this pathological entity.12
 | Assessment for Vascular Injuries |
Vascular injuries are not infrequent with upper cervical spine trauma. The incidence of these injuries remains unclear and depends on the diagnostic modalities used.13 Vertebral artery disruption should be specifically considered in any distractive upper cervical spine injury, such as atlantoaxial dissociation, or in patients with type III or IV atlantoaxial rotary subluxation. In addition, vertebral artery injuries should be considered in any displaced fracture involving the transverse foramen of the atlas or axis. Despite the vertebral artery running in close proximity to the rostral lamina of the posterior ring of the atlas, fractures to the atlas ring have not been commonly associated with local vertebral artery trauma.
 | Assessment for Upper Cervical Spine Injury |
There are few if any specific clinical findings indicative of upper cervical spine injuries. In an awake patient headache or suboccipital tenderness may be encountered. Neurological deficits may range from isolated lower cranial nerve injuries to unusual incomplete upper cervical spinal cord injuries or high tetraplegia with absence of spontaneous respiratory trigger function.14–18
Radiographic evaluation continues to revolve around the use of a lateral C-spine radiograph and, if possible, an open-mouth odontoid view. A coned-down view of the upper cervical spine centered at the C1 lateral mass may offer improved visualization of the radiographic bony interrelationships of this area by avoiding a parallax view. Primary dynamic radiographic testing of this area, such as flexion-extension radiographs and traction testing, is potentially dangerous in an acute setting and therefore not recommended in many centers.
Primary lateral and open-mouth odontoid views remain a mainstay to assess structural stability of the upper cervical spine. The lateral cervical spine radiograph remains the most effective screening tool for cervical spine injuries. In this context, several specific radiographic screening parameters warrant description. Presence of prevertebral swelling beyond 4 mm width rostral to the C4-5 disk space remains a highly significant but nonspecific abnormality worthy of further scrutiny.19 Wackenheim line is a caudally directed extension of the clivus and should lie in close proximity to the tip of the odontoid.19,20 Harris lines describe the distance of the basion to the tip of the odontoid, or the basion-dens interval (BDI), and should be 12 mm or less in adults. The rostral propagation of the posterior wall of the axis should also lie within 12 mm of the basion [i.e., the basion-axis interval (BAI)].21,22 These two reference lines, which have been referred to as the rule of twelves, have been shown to be more sensitive and specific toward identifying craniocervical injury compared with the previously more popular Power’s ratio. This quotient is calculated from the distances of the basion relative to the posterior arch of C1 and the opisthion relative to the anterior arch of C1. A ratio greater than 1.0 implies presence of an anterior occipitoatlantal dislocation. However, this test is meaningless for assessment of posterior or rotational atlanto-occipital injuries and is of questionable value for vertically distracted injuries.23
Dziurzynski and Anderson et al found that a BDI, defined as abnormal when greater than 10 mm, was more sensitive (1.0) and specific (0.995) and had a higher positive predictive value (1.0) and negative predictive value (1.0) than the Power’s ratio, X-line, Harris method, or condylar gap method.24
Structural insufficiency of the transverse atlantal ligament (TAL) can be demonstrated by pathologically increased ADI on upright lateral radiographs or flexion-extension radiographs in a posttraumatic setting. Similarly, loss of parallelism of the anterior cortex of the odontoid to the posterior cortex of the anterior arch of the atlas can be an important sign of TAL insufficiency.25 The space available for the spinal cord (SAC) should not be less than 13 mm. Open-mouth odontoid radiographs are assessed for centering of the odontoid process between the atlantal lateral masses and widening of the lateral masses. Eccentricity of the odontoid or 7 mm or more of lateral mass overhang of the atlas relative to the lateral masses of the axis are cause for concern toward instability.19,20,26
Increasingly, primary CT scans are implemented as the primary diagnostic tool in any patient with head injury in the presence of multiple injuries.27 High-speed image acquisition and improved visualization of the transition zones at the craniocervical and cervicothoracic junction have led to a gradual change of the workup paradigm toward the use of CT scans with sagittal and coronal reformatted views.28
Special attention ought to be directed toward the sagittal reformats of the CT scan looking at the occipital condyles as they articulate with C1 to ensure that the condyles are seated in the saddle. An increased or asymmetrical distance can also be seen on the coronal reformats in patients with craniocervical injuries.
MRI scans have become routine imaging modalities for any patient with cervical spinal cord injury or for assessment for ligamentous injuries in an acute setting.29 Patients with fracture disruption of the transverse processes or distractive craniocervical injuries may have to be considered for a vertebral artery injury. CT angiography (CTA) has become a valuable tool in screening for vertebral artery injury in high-risk patients. More specific assessment of vertebral artery perfusion can be obtained with MR angiography and transcranial Doppler assessment. With these improved imaging tests an increased incidence of vertebral artery injuries has been identified.12,13,30 The clinical relevance of variations in types of intimal vertebral damage, however, remains to be determined.
Although prediction of injury stability can usually be accomplished with the aforementioned static studies, occasionally, dynamic testing may be required. Patient-performed flexion-extension radiographs can be considered for patients who are awake, neurologically intact, and show no spinal fracture-dislocation and are particularly effective in establishing atlantoaxial stability. This technique is, however, precarious and is contraindicated in patients with known or suspected fractures or dislocations of the upper cervical spine. Physician-performed traction radiographs can effectively establish craniocervical stability using sequential lateral radiographs with comparison of initial neutral radiographs to films taken with 5 lb of traction and subsequent increases in 5 lb increments up to 20 lb.13,24 If there is no pathological widening noted on imaging modalities up to that load, relative integrity of the key ligamentous support structures may be safely inferred. Similarly, in the presence of a known fracture of the upper cervical spine, upright lateral cervical radiographs can establish maintenance of stability with external immobilization in place.31
It is imperative to remember to obtain adequate imaging of the remaining spine so as not to miss any other associated injuries.
 | Occipital Condyle Fractures |
Presentation
This injury entity has been notoriously overlooked due to diagnostic limitations. The injury spectrum ranges from trivial incidentally noted fractures to major osteoligamentous craniocervical disruptions with the occipital fracture being just a minor component. Accordingly, the clinical presentations can vary widely. In clinically awake patients neck pain and pain with range of motion may be the sole findings.16 Cranial nerve impairment of the abducens, the glossopharyngeus, and the vagus nerves have been described in association with up to a third of patients with occipital condyle injuries.17 The majority of patients with occipital condyle fractures, however, have concurrent traumatic brain injury. Due to the resultant limitation of the patient examinability, increased diagnostic emphasis is placed on a meaningful diagnostic algorithm.
Classification
Occipital condyle fractures have been increasingly identified with common utilization of CT scans in the primary workup of trauma patients.32,33 The majority of occipital condyle fractures result from compressive or shear forces and are fortunately inherently stable. Anderson and Montesano have provided a simple three-part classification system as an evolution of a more comprehensive but also complex system used in the forensic sciences.34,35 Type I fractures result from axial compression loading and are usually inherently stable. Most type II injuries are usually stable and result from shear mechanisms, with an oblique fracture pattern that extends from the condyle into the skull base. Type III injuries usually have a transverse fracture line through the occipital condyle and represent an avulsion injury of the alar ligament. This injury category should be viewed with a great deal of suspicion because it may represent a globally unstable craniocervical ligamentous disruption, similar to the “tip of an iceberg.” However, regardless of its subtype, any occipital condyle fracture should be evaluated as a possible component of craniocervical dissociation. Similarly, the presence of bilateral occipital condyle fractures, regardless of perceived subtype, should be strongly considered to be indicative of craniocervical disruption.20
Management
Historically the vast majority of occipital condyle fractures were presumably treated with benign neglect or some form of bracing due to lack of diagnosis. Because the diagnostic incidence of occipital condyle fractures has increased with improved diagnostic pathways, the need to predict injury stability and pursuant specific treatment needs has risen accordingly.32 Sadly, there are no larger-scale studies comparing various forms of occipital condyle fracture treatment and respective patient outcomes available to date. It appears that simple brace treatment for 2 to 3 months is sufficient in the management of the majority of type I and II occipital condyle fractures. Type I fractures with substantial comminution may benefit from halo vest immobilization. In the setting of an isolated type I or II occipital condyle fracture surgical stabilization should rarely be necessary. Because type III occipital condyle fractures are indicative of a distractive injury pattern the strong possibility of a craniocervical dissociation should be considered. In that setting, the best possible external craniocervical immobilization of the patient should be implemented and urgent definitive surgical stabilization pursued. Truly isolated type III occipital condyle fractures, however, can be effectively treated similarly to a unilateral alar ligament tear using halo vest immobilization for 2 to 3 months, followed by flexion-distraction radiographs for structural stability assessment.
Complications and Outcomes
There have been very few studies addressing the morbidity associated with occipital condyle fractures.32 Outcome is likely to depend on the potential presence of various comorbidities, such as associated head injury. The outcome of type III fractures that are components of distractive injuries is better represented in the subsequent discussion of craniocervical dissociation outcomes. Although the incidence of posttraumatic arthritis is unknown, given the often displaced intra-articular nature of these injuries, patient outcome is presumably contingent on the presence or absence of symptoms of posttraumatic arthritis such as neck pain, occipital headaches, and restriction in craniocervical motion. Torticollis may result from chronic atlanto-occipital subluxation.16 Cranial nerve deficits of the cranial nerves VI, IX, X, XI, and XII in isolation or combination have been described.17,18
 | Craniocervical Dissociation |
Presentation
There is a notorious paucity of clinical findings affecting patients with craniocervical trauma. In the absence of large-scale epidemiological data it appears that the majority of patients with craniocervical injuries are children below the age of 6 years.36,37 This again places an added emphasis on implementing an appropriate diagnostic algorithm and paying attention to the subtleties of radiographic abnormalities around the craniocervical junction, especially in skeletally immature patients.38 Pertaining to adults, a majority of survivors of this injury present with significant cognitive impairment. Conscious patients will usually complain of severe neck pain or occipital headache. Clinical assessment of cranial nerve function should again be part of routine clinical evaluation.
Classification
Traynelis et al have differentiated craniocervical dissociation patterns according to the direction of displacement of the cranium relative to the cervical spine.39 Although this classification system has been widely accepted it is of limited usefulness due to the inherent craniocervical instability, which leaves the position of the head relative to the neck subject to manipulation.14,40 Moreover, this classification system does not provide a severity scale nor does it provide for inclusion of spontaneously reduced dislocations or bear relevance to the definitive treatment.
Objective signs of insufficiency of the craniocervical ligaments are present with translation or distraction of the respective bony components of the upper cervical spine of more than 2 mm in any plane,1 and neurological injury or concomitant cerebrovascular trauma.13 Using this paradigm we have suggested using a three-stage severity-based injury classification system for atlanto-occipital injuries. Stage 1 injuries represent incomplete ligamentous disruption of the craniocervical junction, which leave the overall functional integrity of the craniocervical junction intact. Isolated alar ligament tears are an example of this injury category. Stage 2 injuries present with borderline radiographic parameters but functionally insufficient or disrupted craniocervical osseoligamentous structures. Partial soft tissue preservation may induce a partial spontaneous injury reduction and thus produce an “occult” craniocervical disruption. This injury category poses a significant challenge to treating medical facilities and may require dedicated imaging tests for diagnosis, such as cranial traction tests (Table 26-1). Stage III injuries are obviously displaced craniocervical separations, usually accompanied by severe neurological injury. This injury stage has been subdivided into category (a) survivors and category (b) non-survivors of primary resuscitation. The latter category has been added for epidemiological purposes. Vertically distracted atlantoaxial dislocations should be considered a form variant of craniocervical dissociations and should be managed accordingly. Similarly vertically distracted odontoid fractures and atlas fractures with horizontal cleavage fracture of the anterior arch of the atlas should be scrutinized for the presence of an underlying craniocervical dissociation.41–46
Stage | Description of Injury |
1 | MRI evidence of injury to craniocervical osseoligamentous stabilizers |
Craniocervlcal alignment within 2 mm of normal | |
Distraction of 2 mm or less on provocative traction radiograph | |
2 | MRI evidence of injury to craniocervical osseoligamentous stabilizers |
Craniocervical alignment within 2 mm of normal | |
Distraction of more than 2 mm on provocative traction radiograph | |
3a | Craniocervical distraction of more than 2 mm on static lateral cervical spine radiographs |
3b | Craniocervical distraction with fatality within 24 hours of injury |



