♦ Preoperative
Imaging
- Magnetic resonance imaging: ± contrast mandatory, variable T1 signal, heterogeneous T2 signal of solid tumor component, fluid attenuated inversion recovery (FLAIR) sequence is useful in delineating cystic portions versus loculated cerebrospinal fluid (CSF) spaces or epidermoid tumors
- Computed tomography: better assessment of calcifications which is present in 90% of pediatric tumors and 70% of adult tumors
- Hydrocephalus: patients may need CSF diversion prior to definitive craniotomy
Endocrine
- Full hormonal analysis is mandatory prior to surgery
- Growth hormone deficiency is most common in children; useful in distinguishing from germinoma which presents with diabetes insipidus; consider serum markers to narrow differential diagnosis
Ophthalmologic
- Formal visual field testing and visual acuity assessment are necessary
Surgical Approaches
- Choose approach based on tumor location and surgeon experience
Pterional
- Advantages: direct route to sella region; good visualization of anterior cranial fossa and retrosellar region
- Disadvantages: unilateral perspective; difficult visualization of contralateral optic nerve and carotid artery
Transsphenoidal or Extended Approach
- Advantages: avoids craniotomy; excellent exposure for pure intrasellar or infrasellar tumors; decompression of chiasm from below
- Disadvantages: risk of CSF leak; poor visualization of tumor lateral or posterior to clivus
Transcallosal
- Advantages: direct route to third ventricle and hypothalamus
- Disadvantages: risk of injury to fornix and corpus callosum
- Advantages: good visualization of the optic apparatus and carotid artery; can be performed with a supraorbital keyhole craniotomy for small tumors
- Disadvantages: limited exposure with prefixed chiasm; poor visualization of the tumor within the third ventricle
Endoscopic
- Advantages: minimally invasive; allows visualization of tumor fragments remote from the surgical corridor; can be used alone or in conjunction with standard approaches
- Disadvantages: not useful for large, solid tumors; poor three-dimensional visualization
Equipment
- Craniotomy tray
- Endoscope instruments
- Mayfield or Sugita (Mizuho OSI) head holder
- Retractor system (Yasargil, Greenberg, Budde halo, or Sugita)
- High-speed drill
- Ultrasonic aspirator
- Microscope
Operating Room Set-up
- High power magnification (loupes and microscope)
- Bipolar and monopolar cautery
- Nondominant approach unless tumor location or surgeon preference
Anesthetic Issues
- Intravenous access (may need central venous access in difficult or very young patients)
- Intraarterial line, blood pressure monitoring
- Antibiotics (cephalosporin, clindamycin, or vancomycin (for penicillin allergies) should be given 30 minutes prior to incision
- Dexamethasone (10 mg) or weight-adjusted dose at time of surgery
- Mannitol 0.5 to 1.0 g/kg for large tumors
- Lumbar drainage for certain large tumors and surgical approach
Intraoperative
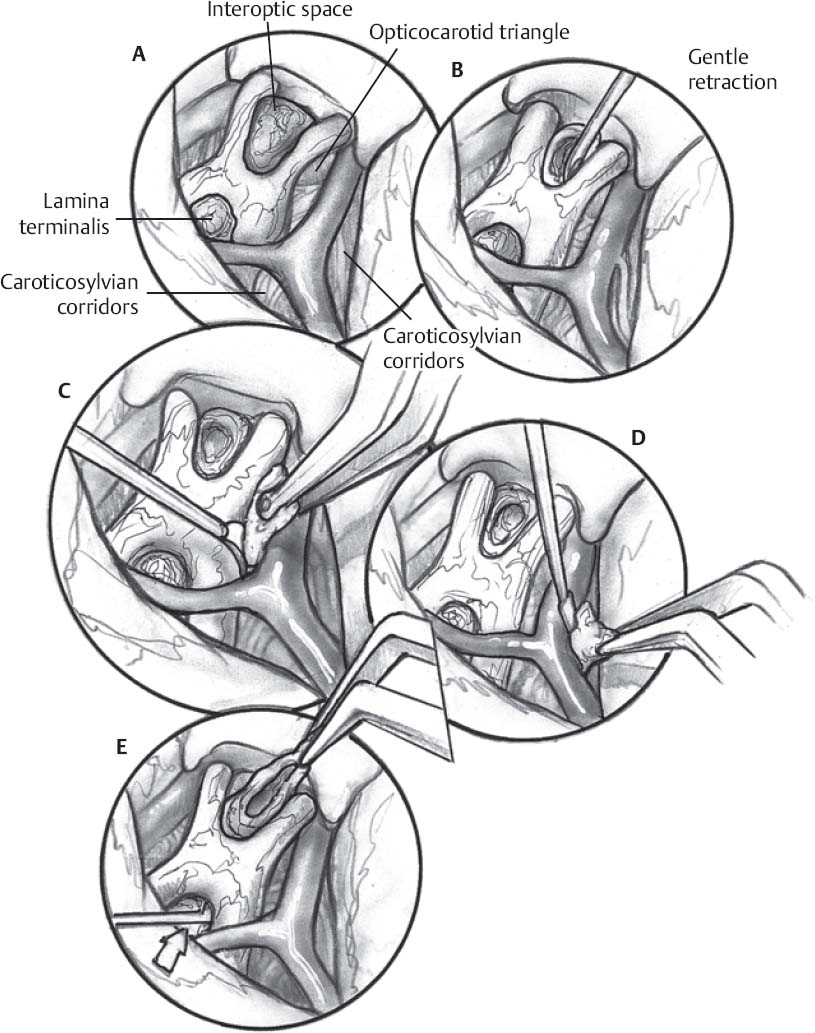
Pterional (Fig. 50.1)
- Nondominant is the preferred side of approach, but final determination depends on the lateral extent of the tumor and visual acuity.
- Early identification of the ipsilateral optic nerve, carotid artery, and pituitary stalk. Be aware of the potential displacement of the optic nerve and chiasm.
- Open arachnoid at sphenoid ridge and optic nerves to allow for CSF drainage
- Tumor capsule then opened along the arachnoid plane
- Internal debulking of solid or cystic tumor with suction or ultrasonic aspirator
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue