19Critical Care
E Mercury
Dimercaprol can increase mercury concentrations in the blood and brain in cases of methylmercury poisoning. DMSA does not increase blood or brain mercury concentrations. (A) Lead chelation historically has been accomplished with EDTA or dimercaprol but now is accomplished with DMSA. (B) Arsenic chelation can be accomplished with dimercaprol, DMPS, or DMSA and less effectively with penicillamine. (C) Cadmium chelation can be accomplished with dimercaprol. (D) Chromium chelation can be accomplished with dimercaprol.
B Phenytoin
Side effects of phenytoin include lupus-like syndromes, Stevens-Johnson variant syndrome, hepatic granulomas, megaloblastic anemia, hirsutism, and gingival hypertrophy. In chronic use, there may be cerebellar degeneration. (A) Side effects of levetiracetam include psychiatric disturbances, somnolence, gait instability, anxiety, gastrointestinal disturbances, and skin pigmentation changes. (C) Side effects of primidone include drowsiness, ataxia, nystagmus, visual disturbances, nausea, and, rarely, Dupuytren contractures. (D) Side effects of valproic acid include dyspepsia and weight gain and, less commonly, peripheral edema and acne. Hair loss, tremors, and severe liver dysfunction also are possible side effects. (E) Side effects of lamotrigine include somnolence, dizziness, diplopia, and, rarely, severe rashes/Steven-Johnson syndrome in a subacute fashion.
C Febrile nonhemolytic
Febrile nonhemolytic transfusion reactions occur in about 1% of transfusions. They are characterized by fevers and rigors occurring within 6 hours of transfusion and are due to antibodies against donor white blood cells and cytokines released from cells in blood products. Febrile nonhemolytic transfusion reactions are treated with acetaminophen. (A) Acute hemolytic transfusion reactions occur in 1/250,000 transfusions and are characterized by fever, hypotension, flank pain, and renal failure within 24 hours of transfusion. These reactions are secondary to ABO incompatibility. (B) Delayed hemolytic transfusion reactions occur 5 to 7 days after a transfusion and are due to undetected alloantibodies against minor antigens. They occur in 1/10,000 transfusions. (D) Allergic transfusion reactions manifest as urticaria and rarely anaphylaxis (patients with an IgA deficiency are most prone to anaphylaxis). Bronchospasm and laryngeal edema also may occur. Allergic transfusion reactions occur in 1% of blood transfusions. (E) Transfusion-related acute lung injury (TRALI) complicates 1/5,000 blood transfusions. TRALI is characterized by noncardiogenic pulmonary edema due to donor antibodies binding recipient white blood cells, which then aggregate in the pulmonary vasculature.
D Vitamin B6
All patients taking isoniazid should be co-treated with vitamin B6 (pyridoxine). Isoniazid induces a state of functional pyridoxine deficiency by directly inactivating pyridoxine species and by inhibiting pyridoxine phosphokinase.
A Decreased right atrial pressure, decreased pulmonary capillary wedge pressure, decreased cardiac output, and increased systemic vascular resistance
The pattern described is reflective of decreased blood volume and thus hypovolemic shock. (B) This pattern is reflective of poor pumping capacity and thus cardiogenic shock. (C) This pattern is reflective of distributive shock, such as neurogenic or septic shock. (D) This pattern is reflective of acute shock in the setting of right ventricular failure or a massive pulmonary embolism. (E) This pattern is reflective of shock secondary to restrictive cardiac disease, such as cardiac tamponade.
A Desmopressin
Von Willebrand disease (vWD) is the most common congenital bleeding disorder and is characterized by a low level of von Willebrand factor (vWF) and subsequently a low level of factor VIII. Patients with vWD have bleeding patterns characteristic of a platelet deficiency. Treatment options include factor VIII concentrate or desmopressin administration, with the latter increasing levels of endogenous vWF by triggering its release from endothelial cells. (B) Von Willebrand factor concentrates should be given in conjunction with factor VIII, but would be helpful only at the time of surgery. (C) Factor VII is not deficient in the setting of vWD. (D) Intravenous crystalloids are not helpful in this situation. (E) Factor IX is not deficient in the setting of vWD.
B PaCO2 of 65 mm Hg with a 20 mm Hg rise over the patient’s baseline after 12 minutes of testing with no spontaneous respirations
Hospital protocols may vary slightly, but almost all are based on the Harvard Brain Death Criteria. Although apnea testing is not part of these criteria, the test is relatively standardized. Apnea testing includes 15 minutes of preoxygenation with 100% FiO2, maintenance of normal blood pressure, preservation of oxygenation saturation greater than 80% with passive oxygen, and the absence of conditions that would prevent the patient from breathing at higher levels of PaCO2 (e.g., severe COPD, congestive heart failure).
C Opening pressure 30, 1,500 WBC with more than 80% PMN, protein 400, glucose 10
This profile represents bacterial meningitis characterized by an elevated opening pressure, low glucose, high protein, white blood cell count over 200 with a polymorphonuclear leukocyte dominance, and a turbid appearance.
D Opening pressure 21, 110 WBC with more than 50% lymphocytes, protein 80, glucose 50
This profile represents viral meningitis characterized by a slightly elevated opening pressure, normal glucose, normal protein, white blood cell count under 200 with a mononuclear dominance, and a clear appearance. (A) This profile represents a normal cerebrospinal fluid sample. (B) This profile represents tubercular meningitis characterized by a high opening pressure, low glucose, high protein, low white blood cell count, and a cobweb appearance.
A Its lack of analgesia
Although it is a poor analgesic, propofol has excellent properties including an ability to lower intracranial pressure, induce rapid anesthesia, and provide hypnotic and euphoric effects. Propofol does lower seizure thresholds and can mask the clinical signs of a patient being in status epilepticus.
A Stop the anesthetic agent.
The diagnosis in this case is malignant hyperthermia, and the first step in the management is to discontinue volatile anesthetic agents and succinylcholine. The patient should then be hyperventilated to 100% FiO2 in order to flush volatile anesthetics from her system and lower the end tidal PCO2. Intravenous dantrolene then should be given until the patient has a decrease in the end tidal PCO2. Calcium chloride, glucose, and insulin can be given for hyperkalemia resulting from malignant hyperthermia.
C Nitrous oxide
Nitrous oxide is a unique inhalational agent in that it greatly increases cerebral blood flow with only a small increase in cerebral metabolism. Most other agents lower cerebral metabolism. Nitrous oxide also can be associated with a risk of air embolism and pneumocephalus due to its high solubility.
A They suppress EEG activity.
All halogenated agents suppress EEG activity, which may be neuroprotective; however, the EEG effects must be considered when performing intraoperative neuromonitoring. Some anesthetics, such as enflurane, counterintuitively lower the seizure threshold despite EEG suppression. (B–D) All halogenated anesthetics tend to increase cerebral blood flow while reducing cerebral metabolism. This results in increases in intracranial pressure to some extent. (E) At high, and even normal, therapeutic doses, halogenated anesthetics can show signs of hepatotoxicity in some patients.
B No analgesic effect
Propofol is a sedative hypnotic that reduces cerebral metabolism and intracranial pressure without any analgesic effects.
D Nitroglycerin and nitroprusside raise intracranial pressure.
Nitroglycerin and nitroprusside raise intracranial pressure through their vasodilatory effects. (A) Nitroglycerin and nitroprusside have no significant effect on the seizure threshold. (B) Nitroglycerin and nitroprusside can cause neurologic symptoms as patients develop thiocyanate and cyanide toxicity with elevated doses or prolonged use. (C) Nitroglycerin and nitroprusside both have a vasodilatory effect, with the former having more of an effect on the venous system and the latter having a greater effect on the arterial system. (E) Nitroglycerin and nitroprusside have variable effects on cerebral perfusion pressure depending on the degree of intracranial pressure increase and decrease in mean arterial pressure.
B Colloids (e.g., dextran, hetastarch)
Colloids as a whole (but especially certain ones like dextran and hetastarch) have been shown to worsen coagulopathies.
A Obtaining a muscle biopsy for in vitro testing
The gold standard to test for the risk of developing malignant hyperthermia is contracture testing. It relies on the in vitro measurement of the muscle contracture response of a biopsied muscle to graded concentrations of caffeine, halothane, and other calcium-releasing agents. (B) More recently, two genes predisposing individuals to developing malignant hyperthermia have been identified, the most common of which is the RYR1 gene mutation (accounting for 70% of malignant hypothermia cases).
B Phenylephrine
In spinal shock, there is sympathetic dysfunction with an intact parasympathetic system. Bradycardia is a manifestation; therefore, an agent with positive inotropic effects is required. Phenylephrine (unlike the other choices) is non-inotropic and thus should be avoided.
D In primary adrenal insufficiency, both glucocorticoids and mineralocorticoids need to be replaced.
Primary adrenal insufficiency (adrenal gland failure) requires the replacement of both glucocorticoids and mineralocorticoids, whereas mineralocorticoid secretion tends to be preserved with secondary adrenal insufficiency. It is important to select a steroid with the appropriate properties.
A Hypertension and hypokalemia
Hypertension and hypokalemia may occur when cortisone is used in the setting of secondary adrenal insufficiency even when the steroid is dosed appropriately to provide glucocorticoid support. This is due to the mineralocorticoid effects of cortisone in addition to the adrenal glands’ endogenous production of mineralocorticoids.
A Thiopental
Thiopental is a short-acting barbiturate general anesthetic that decreases intracranial pressure in a fashion superior to pentobarbital. In addition, thiopental decreases cerebral blood flow and cerebral metabolic rate/oxygen consumption. Recently, propofol and etomidate have been used increasingly, as they have similar neuroprotective effects and a shorter duration of action.
C Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura (TTP) is characterized by severe thrombocytopenia, microangiopathic hemolytic anemia, fluctuating neurologic status, renal failure, and fever. (A) Idiopathic thrombocytopenic purpura is a diagnosis of exclusion; it occurs in patients with normal red blood cells. (B) Disseminated intravascular coagulation (DIC) has a presentation similar to that of TTP, with an elevation in the INR and partial thromboplastin time. Although in TTP the problem mainly is thrombocytopenia, in DIC there is a consumptive coagulopathy that manifests with decreased platelets and increased fibrin split products and d-dimers. DIC typically occurs following trauma or in the presence of sepsis. (D) Neurologic changes are rare in hemolytic uremic syndrome.
D The patient is volume depleted.
In both cerebral salt wasting (CSW) and syndrome of inappropriate antidiuretic hormone secretion (SIADH), the serum sodium concentration may be low due to salt loss (CSW) or hemodilution (SIADH). A patient with either condition may have accompanying cerebral edema due to the reduction in serum sodium concentration. Low urine output can occur because of high levels of antidiuretic hormone (SIADH) or volume depletion (CSW). Although volume status is low in CSW, it is normal to increased in SIADH.
B Central pontine myelinolysis
Central pontine myelinolysis (CPM) is the likely cause of a sudden quadriplegia with pseudobulbar palsies. Confusion and other mental status changes can occur. CPM has an acute onset when a hyponatremia is corrected rapidly (usually a correction of the serum sodium of more than 25 mEq/L within 48 hours). This patient’s acute alcohol use in the setting of chronic alcoholism would tend to cause hyponatremia in addition to a nutritional deficiency. With sudden nutritional supplementation in the form of regular meals and the likely sodium correction he received, the patient would be prone to developing CPM. (A) Beriberi is a syndrome due to thiamine deficiency. It can either be “dry,” characterized by wasting, peripheral neuropathies, and confusion, or “wet,” characterized by heart failure and peripheral edema. Although the patient may be deficient in thiamine due to his chronic alcoholism, this is a chronic condition unlikely to present acutely. (C) Pseudohyponatremia is a decreased serum sodium lab value in the setting of hyperglycemia. The clinical picture does not support a diagnosis of hyperglycemia in this patient. (D) Cerebral edema is possible in the setting of cerebral contusions and the likely hyponatremia, as explained above, but the patient was preparing for discharge home and was neurologically intact. Sudden cerebral edema is not expected with this clinical picture. (E) A missed cervical spinal cord contusion would not have a sudden onset, nor would it cause the confusion or pseudobulbar palsies described.
C Hyperventilation to achieve a PaCO2 of 30 to 35 mm Hg is appropriate to use as a temporizing measure for patients with signs of progressive neurologic deterioration when ICP monitoring is not yet established.
Hyperventilation to achieve a PaCO2 of less than 30 mm Hg should not be used, because it will reduce cerebral blood flow and exacerbate cerebral ischemia without a further reduction in intracranial pressure. (B) Level 2 guidelines indicate that prophylactic hyperventilation is not recommended.
D 10 mg/kg intravenous bolus over 30 minutes followed by a 1 mg/kg/h infusion
10 mg/kg intravenous bolus over 30 minutes followed by a 1 mg/kg/h infusion is the regimen for the treatment of intracranial hypertension using a pentobarbital coma. The dosing is modified to sustain the coma and is followed by serum pentobarbital levels. (A) 20 mg/kg intravenous bolus followed by 100 mg every 8 hours represents a phenytoin loading/maintenance dose for seizure prophylaxis. (B) 100 mg intravenously every 4 hours is a pentobarbital dosing regimen for increased intracranial pressure when used as a sedating agent (not to induce a pentobarbital coma). (C) 20 to 75 μg/kg/min intravenous continuous drip is a standard dosing range for propofol sedation.
A Clozapine
Agranulocytosis is a characteristic side effect of clozapine and occurs in 1 to 2% of patients; therefore, patients on clozapine need to be monitored with regular complete blood counts. Other side effects of clozapine include extrapyramidal symptoms and tardive dyskinesia, with a rarer side effect being sialorrhea (drooling). (B) Thioridazine can lead to pigmentary retinopathy and atropine-like effects. (C) Chlorpromazine can lead to abnormal skin pigmentation and “gray man” syndrome. (E) Quetiapine can lead to an increase in suicide attempts in major depression.
A Equivalent level = Observed level/(0.1(Albumin level) + 0.1)
The key to deriving the conversion equation is knowing that 90% of phenytoin is protein bound, and in the setting of hypoalbuminemia, the equivalent phenytoin level will be higher that the observed phenytoin level. The equation in answer A is the only one that would yield an equivalent level greater than the observed level.
C Nitrous oxide
The use of nitrous oxide has been linked to the development of tension pneumocephalus following surgery in the supine position. Nitrous oxide is known to increase cerebral blood flow and can diffuse into air-filled spaces and expand gaseous volume. On CT, a “Mount Fuji” sign (compression of the bilateral frontal lobes with separation of the frontal poles by air) is a characteristic feature of postoperative tension pneumocephalus.
A Noncollapsible vein and negative pressure in the vein
Injury to a noncollapsible vein (diploic vein or dural sinus) and negative pressure inside the vein are essential factors in the pathogenesis of air emboli. Negative pressure created by elevating the head above the level of the heart is necessary to entrain air into the venous circulation. A collapsible venous structure would collapse under negative pressure, which is why injury to a noncollapsible structure is another essential factor in the pathogenesis of air emboli. The presence of a patent foramen ovale or a pulmonary arteriovenous fistula can lead to paradoxical air emboli with the production of ischemic strokes.
C Streptococcus pneumoniae
Most posttraumatic meningitis in the setting of nonpenetrating and nondepressed skull injuries are pneumococcal in nature, and therefore empiric treatment should be targeted against these bacteria. Of note, the standard use of prophylactic antibiotics in such patients is debatable, and antibiotics should be used on a case-by-case basis.
A Calcium gluconate
The first step in the management of symptomatic hyperkalemia is to administer calcium gluconate for its cardioprotective effect. Only then should potassium levels be lowered with medications including insulin and glucose, Kayexalate, and β-agonists.
C Flumazenil
The reversal agent for benzodiazepines is flumazenil. It works as a competitive inhibitor competing with benzodiazepines for the binding site on GABA-A receptors.
F Naloxone
The reversal agent for morphine is naloxone. Naloxone is a mu-receptor competitive antagonist with a high affinity for the mu-opioid receptors in the central nervous system.
B Physostigmine
The antidote for anticholinergics is physostigmine. It is a reversible cholinesterase inhibitor.
E Phentolamine
The antidote for dopamine overdose is phentolamine. It works through α1-blockade. (A) Atropine is a competitive antagonist of muscarinic acetylcholine receptors. (D) Glucagon is a pancreatic peptide hormone that has an effect opposite that of insulin. Glucagon raises the blood glucose concentration. (G) Protamine is used to reverse the effects of heparin. (H) Dimercaprol is a chelating agent used to treat heavy metal poisoning.
B Nonselective β-adrenergic agonism
Isoproterenol is a β1– and β2-adrenoreceptor agonist and a trace amine associated receptor 1 (TAAR1) agonist. It has a positive inotropic and chronotropic effect. It also leads to arrhythmias and vasodilation that is more accentuated in skeletal muscles compared with cerebral vessels. Isoproterenol should not be administered for a patient with myocardial ischemia.
A Breaths are patient- or time-triggered with a constant tidal volume for each breath.
Assist control ventilation is patient-triggered. If a patient fails to breathe, the ventilator machine will take over at a specified rate. Each breath taken has a preset tidal volume. (B) Synchronized intermittent mandatory ventilation is similar to assist control ventilation except that patient-initiated breaths are not supported. (C) Pressure support ventilation can be a stand-alone ventilation mode or combined with synchronized intermittent mandatory ventilation. The concept is to deliver additional pressure for patient-initiated breaths. (D) This answer represents continuous positive airway pressure (CPAP) ventilation where the patient must breathe independently of the ventilator.
B Metabolic acidosis
A low pH indicates acidosis, whereas a low bicarbonate level and a relatively normal PCO2 is indicative of a metabolic origin.
A Respiratory alkalosis
A high pH indicates alkalosis, whereas a low PCO2 and normal bicarbonate level is indicative of a respiratory origin. (C) A high pH indicates alkalosis, whereas a combined low PCO2 and high bicarbonate level is indicative of a combined respiratory and metabolic origin. (D) A low pH indicates acidosis, whereas a high PCO2 is indicative of a respiratory origin. There is partial metabolic compensation as indicated by the rise of the bicarbonate level above normal. Compensatory mechanisms never fully reverse the primary acid/base abnormality.
Normal target labs values are as follows:
pH: 7.40
PCO2: 40 mm Hg
HCO3−: 24 mEq/L
B Age greater than 40 years, systolic blood pressure less than 90 mm Hg, and posturing on motor exam
In a patient with a normal head CT following a concussion, if two or more risk factors are present, there is a 60% risk of developing intracranial hypertension. This risk decreases to 4% if one or no risk factor is present.
A1 mm Hg = 1.36 cm H2O
An intracranial pressure of 15 mm Hg is approximately 20 cm H2O (exact is 20.4 cm H2O).
C Normothermia
To this day, there is no definitive evidence in favor of hypothermia (whether it is induced or permissive) in a patient with a traumatic brain injury. There have been at least four meta-analyses that concluded that there is no evidence suggesting that hypothermic patients have better outcomes than normothermic patients. (D, E) Hyperthermia should be avoiding in patients with a traumatic brain injury.
C Etomidate
Etomidate is used for induction and can produce adrenal insufficiency. (A) Propofol’s exact mechanism of action is unknown. It is a good agent for total intravenous anesthesia and can be used for burst suppression. (B) Dexmedetomidine is an α2-agonist that can be used for sedation. (D) Ketamine is an NMDA antagonist that produces a dissociative anesthesia and increases intracranial pressure.
A Bilateral absence of the N20 waveform
The N20 waveform reflects activity in the thalamocortical radiations and sensory cortex. Bilateral absence of the N20 waveform at least 3 days after CPR, therefore, is a predictor of a poor neurologic outcome. (B) The N9 waveform reflects peripheral nerve activity and usually is expected to be present. It does not indicate the state of the central nervous system. (C) The N13 waveform reflects activity in the dorsal horns of the spinal cord and would be expected to remain present in the described patient.
C Breaths are patient-triggered, and inspiratory pressure is added to patient-initiated breaths.
Pressure support ventilation can be a stand-alone ventilation mode or combined with synchronized intermittent mandatory ventilation. The concept is to deliver additional pressure for patient-initiated breaths. (A) Assist control ventilation is patient-triggered. If a patient fails to breathe, the ventilator machine takes over at a specified rate. Each breath taken has a preset tidal volume. (B) Synchronized intermittent mandatory ventilation is similar to assist control ventilation except that patient-initiated breaths are not supported. (D) This represents continuous positive airway pressure (CPAP) ventilation where the patient must breathe independently of the ventilator.
D Toxoplasmosis
Toxoplasmosis is one of the most common neurologic complications of AIDS. Patients present with fever, headaches, seizures, and possibly focal neurologic deficits. Multiple ring-enhancing lesions are seen in 70% of patients with toxoplasmosis. Distinguishing toxoplasmosis from lymphoma can be difficult, and a trial of antitoxoplasmosis medications may be used for 2 weeks to confirm the diagnosis.
F JC virus
JC virus leads to progressive multifocal leukoencephalopathy (PML). This fatal disease has no effective treatment. Symptoms develop over several weeks and include clumsiness, progressive weakness, and vision, speech, and personality changes. Characteristic imaging findings include multifocal hypointense T1 and hyperintense T2 lesions.
E West Nile virus
West Nile virus causes poliomyelitis and meningitis, with poliomyelitis being the most common manifestation. Patients typically have fever, myalgias, and encephalopathy along with asymmetric weakness that quickly can progress to quadriplegia. Cerebrospinal fluid studies show pleocytosis and elevated protein. (A) Tenia solium is a tapeworm found in pigs that causes neurocysticercosis. Symptoms include seizures, decreased vision, papilledema, and parkinsonism. Although the pork supply in the United States is free of the organism, pork in Central and South America may be colonized. (B) Herpes simplex causes temporal encephalitis and temporal epileptiform discharge on electroencephalogram. (C) Central nervous system Cryptococcus infection can manifest with multiple focal mass lesions called cryptococcomas. The opening pressure during a lumbar puncture is high, cryptococcal antigen titer is positive, and cerebrospinal fluid India ink staining is positive with this condition, which is common in patients with HIV. Treatment is with amphotericin B and flucytosine.
C Needle thoracotomy
This patient developed a right-side tension pneumothorax most likely secondary to the rupture of a lung bulla precipitated by mechanical ventilation. Because he is unstable, emergent needle decompression of the right lung should be performed at the bedside to decompress the intrapleural space and enable adequate venous return. (A) A chest tube will be needed in this patient with a tension pneumothorax, but needle decompression should be done first. (B) The diagnosis in this case is obvious. Obtaining a chest radiograph will only delay a lifesaving treatment. (D) Ultrasounds are readily available in most intensive care units. They can be used to diagnose pneumothorax effectively; however, in this patient, an ultrasound will only delay a lifesaving treatment. (E) Decreasing the respiratory rate and tidal volume help to prevent tension pneumothoraces in predisposed patients.
C Fat embolism
Fat emboli occur 1 to 3 days following long bone or pelvic fractures. Patients develop tachypnea, tachycardia, hypotension, mental status changes, thrombocytopenia, and petechiae. The petechial rash is pathognomonic for a fat embolism. (A) Although subdural hematoma expansion cannot be ruled out, it is unlikely to occur in a patient stable for 2 days. (B) A pulmonary embolism is a possibility; however, a long bone fracture with a petechial rash in a young patient favors a diagnosis of fat embolism. (D) Myocardial contusions usually manifest with arrhythmias. (E) Pulmonary contusions are most likely to appear on a chest radiograph.
B Aseptic meningitis
Penicillins and cephalosporins have been linked to aseptic meningitis, with the exact pathophysiology being unknown. Other medications linked to aseptic meningitis are trimethoprim-sulfamethoxazole, ciprofloxacin, metronidazole, and isoniazid.
A Benign intracranial hypertension
Amphotericin B can lead to benign intracranial hypertension.
C Cerebellar ataxia
Ethambutol is known for causing optic neuritis; however, another side effect of this antituberculous drug is cerebellar ataxia. Patients need routine ophthalmologic exams while on the medication. (D) Vancomycin can cause cochlear and vestibular dysfunction. (E) Side effects of temozolomide include nausea, vomiting, constipation, diarrhea, blurred vision, sleep problems, unusual or unpleasant tastes, and headaches. Patients also may have temporary hair loss.
A In a patient with central DI, DDAVP will cause a 50% increase in urine osmolality, whereas it will cause an increase of 5% in a normal individual.
Patients with central diabetes insipidus (DI) have an impaired production of antidiuretic hormone, and therefore have a significant response to the injection of DDAVP. Patients with nephrogenic DI do not show a response to DDVAP injection.
B Neuroblastoma
Opsoclonus-myoclonus is composed of involuntary arrhythmias and chaotic multidirectional saccades with myoclonic jerks of the limbs and trunk as well as cerebellar ataxia, tremors, and encephalopathy. In children, 50% of cases are secondary to a neuroblastoma, whereas in adults the condition can be secondary to small cell lung, ovarian, or breast cancer.
A Hodgkin lymphoma
Paraneoplastic cerebellar degeneration is characterized by a loss of Purkinje cells. Symptoms include gait unsteadiness that evolves into ataxia, diplopia, and dysarthria. This condition most commonly is seen in patients with lung, ovarian, or breast cancer, and Hodgkin lymphoma.
D Thymoma
Limbic encephalitis presents with mood and sleep disturbances, seizures, hallucinations, and short-term memory loss. Electroencephalography shows foci of epileptic activity in the temporal lobes, and MRI demonstrates hyperintense T2 and FLAIR sequence signals in the mesial temporal lobes. Most commonly, the condition involves tumors including small cell lung cancer, germ cell tumors, thymomas, and teratomas. Of these tumors, thymomas are associated with myasthenia gravis.
C Small cell lung cancer
Lambert-Eaton myasthenia syndrome involves the muscles of the trunk, shoulder and pelvic girdles, and lower extremities. It is most commonly associated with small cell lung cancer and is due to antibodies against the presynaptic calcium channels at neuromuscular junctions. (E) Carcinoid tumors can secrete hormones such as serotonin, resulting in carcinoid syndrome (characterized by flushing, wheezing, diarrhea, abdominal cramping, and peripheral edema).
C 28 mm Hg
Decreasing PCO2 leads to cerebral vasoconstriction, and with decreased cerebral blood volume, intracranial pressure can be reduced significantly. When PCO2 decreases below 28 mm Hg, the cerebral blood volume can decrease to a level at which ischemia occurs. A recommended typical long-term goal for hyperventilated patients is a PCO2 of 35 mm Hg. A PCO2 of 28 to 32 mm Hg can be tolerated for 4 to 8 hours in the acute setting.
A Asystole or pulselessness will occur within 1 hour of withdrawal of care.
When proceeding with attempted donation after cardiac death, the expectation is that the potential donor will progress rapidly to cardiac arrest. This criterion is intended to minimize warm ischemia time. The convention is that warm ischemia time of up to 1 hour can be tolerated. If cardiac arrest does not occur within 1 hour after withdrawal of care, organ donation is cancelled. (B) Patients who undergo donation after cardiac death do not meet brain death criteria and are declared deceased by cardiac criteria before proceeding with donation. (C) The transplant surgeons usually are excluded from the donation after the cardiac death procedure until arrest is declared. (D) The heart cannot be donated after asystole.
C 800 mL
The estimated blood volume in infants and children is approximately 8% of total body weight or 80 mL of blood per kilogram of body weight.
C Carbamazepine
Although all of the options are used as first-line therapies for trigeminal neuralgia, carbamazepine alone provides complete or tolerable relief in almost 70% of patients. Its common side effect is mild leukopenia with a lesser frequency of rash and even Stevens-Johnson syndrome in rare cases.
A Alcoholic hallucinosis
Patients experiencing alcohol withdrawal can start developing minor symptoms within 6 hours of their last drink. These symptoms include tremulousness, anxiety, sweating, and palpitations. This initial stage of alcohol withdrawal is followed by alcoholic hallucinosis, which occurs between 24 and 48 hours following the last drink. Symptoms include visual, auditory, or tactile hallucinations without autonomic changes. (E) The last stage of alcohol withdrawal is delirium tremens, with symptoms including hallucinations, disorientation, tachycardia, hypertension, low-grade fever, agitation, and diaphoresis. Delirium tremens occurs 3 to 10 days following the last drink.
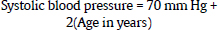
A 70 mm Hg + 2(Age in years)
The lower limit of a normal systolic blood pressure (fifth percentile) for a given age may be estimated by this formula:
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree