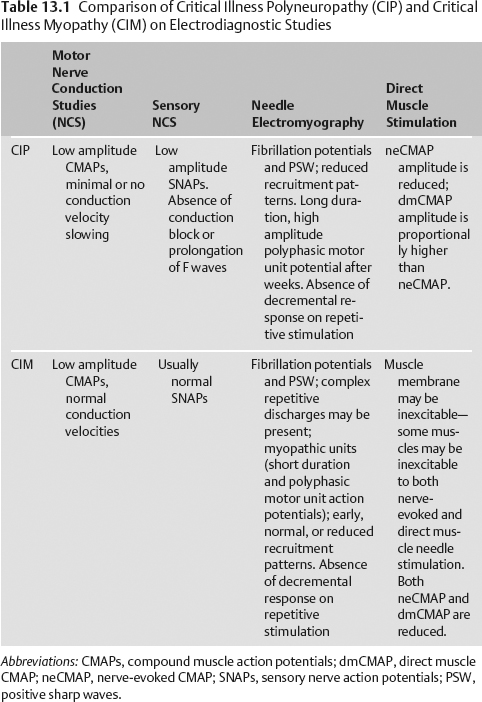
13 Critical Illness Polyneuropathy and Myopathy Valerie Dechant, Eduardo Adonias de Sousa, and Kiwon Lee Critically ill patients are at risk for developing severe weakness secondary to critical illness polyneuropathy (CIP) and/or critical illness myopathy (CIM). Weakness may progress to severe quadriparesis and muscle wasting.1 The incidence of CIP/CIM in critically ill patients has been reported as 33 to 44% of patients with prolonged admission to critical care settings. The incidence increases to nearly 70% when considering only patients with sepsis.1–5 Risk factors that have been suggested for CIP and CIM include: Assess for symmetry in the exam: gross asymmetry (hemiparesis, paraparesis, hemisensory loss or crossed signs) suggests an etiology other than CIP/CIM. Prominent mental status changes, cranial nerve involvement, pain, bowel or bladder involvement, cerebellar signs or a sensory level should prompt further work-up. Studies that have employed both biopsy and advanced electrodiagnostic studies suggest that CIM is as common as CIP and that the two often coexist. Differentiation between the two based on physical exam or even basic electrodiagnostic testing can be extremely difficult.5,6 Direct muscle stimulation (DMS) has been suggested as a technique to differentiate CIP and CIM. Compound muscle action potential (CMAP) amplitudes derived from direct muscle stimulation (DMS) may be inexcitable (absent) or decreased (<2 mV) in CIM, while they remain normal in CIP. However, nerve-evoked CMAPs are reduced in both CIP and CIM. Thus, a ratio of nerve-evoked CMAP to DMS CMAP would be >0.5 in patients with CIM and <0.5 in patients with CIP (Table 13.1).
History and Examination
History
Physical Examination
Neurologic Examination
Differential Diagnosis
Life-Threatening Diagnoses Not to Miss
Diagnostic Evaluation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree