Fig. 15.1
CSF findings
In 91 of 105 patients in this study had a CSF analysis, and in this group 34 out of 91 had abnormal CSF including 3 with pyogenic organisms seen at Gram stain, 11 had capsulated yeast cells and 1 had AAFB (atypical acid fast bacteria). In 54 % of these cases there were abnormal CSF results without meningeal enhancement at CT.
Density of Brain Lesions (Fig. 15.2 and Table 15.1)
Fig. 15.2
Density of brain lesions
Table 15.1
Behavior of IV contrast
Pattern | Number | Percentage |
|---|---|---|
Non enhancing | 25 | 47.2 |
Ring | 16 | 30.2 |
Nodular | 11 | 20.8 |
Not applicable | 1 | 1.9 |
Total | 53 | 100.0 |
Behavior with IV Contrast. In each case multiple lesions were a common feature and 50.5 % had detectable brain lesions. In these cases 83.0 % of lesions were hypo dense, with 39.6 % in white matter, 26. 4 % in the Basal ganglia. In the analysis of CT findings after iv contrast, Table 15.1, 47.2 % were non-enhancing, 30.2 % were ring shaped and 20.8 % were nodular in appearance. Patients with lymphomas usually had single lesions while patients with toxoplasmosis had multiple lesions.
Clinical Signs and Symptoms of HIV Infected Patients
Fever and headache are the most frequent symptoms in these HIV patients (Table 15.2). The clinical features listed in Table 15.2 may not be a specific symptom of CNS diseases with headache due to irritation of the meninges and arteries with their associated pain nerve fibers. The headache as a symptom is subjective, sometimes ambiguous and its severity difficult to assess. The fifth, ninth and tenth cranial nerves contain pain fibres are also found in the meninges and are recording the meningeal irritation and sending it into the brain. Headache may therefore be due to cranial neuralgias, meningeal irritation, vascular disturbances and traction of intracranial structures which have pain nerve fibers. Neck rigidity and positive Kerning’s sign are absent in 58.8 % of patients with abnormal cranial CT results. This may reflect subacute meningitides from Cryptococcal and TB infections which rarely give signs of meningeal irritation [2].
Table 15.2
Clinical features
Clinical features | No. abnormal | % abnormal |
|---|---|---|
Headache | 61 | 76.3 |
Vomiting | 16 | 55.2 |
Convulsions | 19 | 48.7 |
Photophobia | 7 | 53.8 |
Fever | 56 | 78.9 |
Neck rigidity | 23 | 82.1 |
Kernig’s sign | 20 | 90.9 |
Altered consciousness | 18 | 56.3 |
Focal neurological signs | 43 | 64.2 |
The brain parenchyma, pia-arachnoid, ventricular linings and choroid plexuses are insensitive [8].
Neurological Signs
Focal neurological signs (Table 15.3) were encountered in 63.8 % of the patients in this study and these are usually strong predictors of presence of structural lesions at CT (P value = 0.0004). It has been observed from other populations of AIDS patients that the frequency of CNS symptoms is about 30 % and at postmortem the occurrence of CNS abnormalities is as high as 80 % [2]. By the time of death many of these patients demonstrate more pathological lesions that were not detected by CT imaging.
Table 15.3
Focal CNS signs
Signs | Number | Percentage |
|---|---|---|
Focal CNS signs | 67 | 63.8 |
Altered consciousness | 32 | 30.5 |
Neck rigidity | 28 | 26.7 |
Kerning’s sign | 22 | 21.0 |
Altered consciousness is the second common predictor of presence of structural lesions (P value = 0.568) and Kerning’s sign the least. These neurological manifestations result from opportunistic infections or from primary involvement of the brain by the HIV and primary CNS lymphomas [9, 10]. Although CNS infections, including syphilis, bacterial meningitis, brain abscesses, and tuberculosis are seen in HIV infected individuals, cryptococcal meningitis and toxoplasmosis predominates [11–14]. Most patients present with severe persistent headache, fever and lethargy. Peculiar to toxoplasmosis is focal neurological abnormalities, confusion and seizures in addition to the general symptoms mentioned above (see Fig. 15.10).
Final Clinical Diagnosis
Final clinical diagnosis and clinical correlation in this study are listed in Fig. 15.3 , with Toxoplasmosis 28 % of the cases, cryptoccal meningitis 18 %, and bacterial meningitis 8 %. Tuberculous meningitis and viral encephalitis each form 4 % of the cases. Depression and cerebral malaria were each 3 % and PML, Hemorrhagic strokes, bacterial cerebritis, pyrogenic empyema, subacute subdural were 1–2 % of the cases,
Fig. 15.3
Final diagnosis
Abnormal CT Appearances
In the current study 63 % of the patient’s had focal CNS findings. The frequency of brain structural lesions in another study one study in Uganda in 1998 was 50.5 %. The available literature gives a lower percentage of between 20 and 40 % [15–17]. This high frequency of mass lesions in this study is probably related to the patients who were referred for CT examination were very ill thus with more obvious lesions including a higher rate of complicating opportunistic infection. Lesions also exhibit variable contrast enhancement depending on vascularization and brake down of the blood–brain barrier.
Appearance of Intracranial Infections
Opportunistic lesions (Fig. 15.4) of the CNS occur are caused directly by HIV infection and there can be other complications including dementia, cerebral toxoplasmosis, Cryptococcal meningitis (CM) and progressive multifocal leukoencephalopathy (PML).
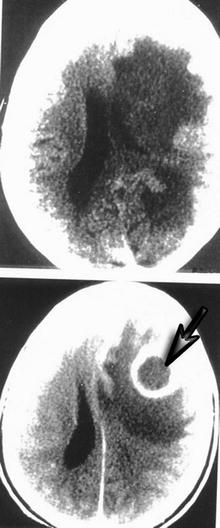
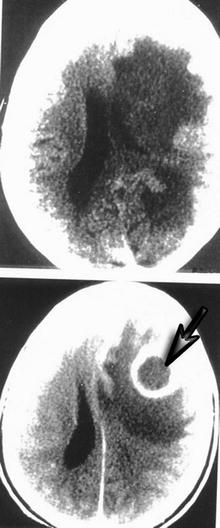
Fig. 15.4
A 29 year old female presented with right sided body weakness, fever and reduced level of consciousness. Enhanced CT scan results show a ring enhancing lesion in left frontal lobe with gross surrounding edema. The patient improved on antibiotic therapy and surgical drainage which confirmed a pyogenic abscess
Diffuse white matter hypodense non-enhancing lesions are seen in PML, CMV and HIV encephalitis.
Toxoplasmosis causes chronic necrotizing inflammation of the brain that appears as necrotic foci in which tachyzoites and/or cysts can be seen. At the edge of these foci, inflammatory infiltrates and multinucleated giant cells are found [2]. Calcifications often ensue later as well as atrophy and later small gliotic scars form.
The CT appearances of intracranial infections are characteristic [2, 18–20]. In this study the majority of lesions are hypo dense on CT without contrast administration as they are inflammatory. They appear hypo dense due to the edema which is of low attenuation (see Fig. 15.1 and Table 15.1).
Brain abscesses have a characteristic “doughnut” appearance. The pre-contrast scan shows a hypodense lesion (Fig. 15.4). The hypodense area in the center represents non-viable debris, while the ring enhancing and the peripheral hypodense area represent the capsule and edema respectively. The increased tissue water content in inflammatory lesions gives low attenuation co-efficiencies in comparison with normal brain. The normal brain grey and white matter Hounsfield readings are in the range of 36–46 and 22–32 respectively [20].
Figure 15.4 demonstrates ring and nodular lesions. The lesion shows ring enhancement post-contrast with marked surrounding edema. This was confirmed as a pyogenic abscess following surgical drainage.
Figure 15.5 illustrates the pathological features of meningitis at postmortem examination.
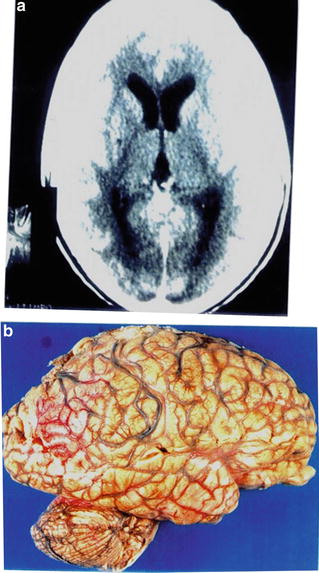
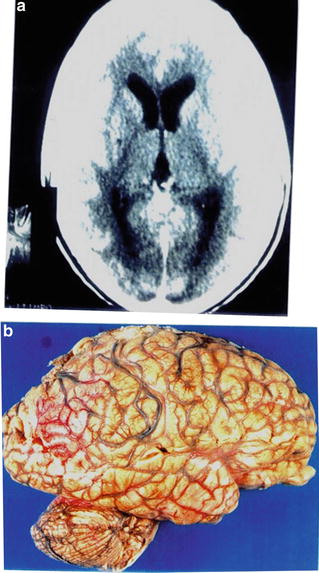
Fig. 15.5
A 31 y.o. male presented with history of fever, severe headache and left 6th cranial nerve palsy. Enhanced CT scans (a) show marked generalized meningeal enhancement. Patient passed away, and postmortem gross specimen (b) revealed mucoid whitish appearance over the brain most marked in the Sylvain fissures and post-central sulcus
Encephalitis (Figs. 15.6, 15.7, 15.8, and 15.9) is associated with little or no change in CT appearance of the brain. Ill-defined hypo dense areas without focal enhancement may be the only finding. Non-enhancing lesions are also highly prevalent accounting for 47.2 % is cases of CNS lesions. Intracerebral lesions do enhance with I.V. contrast medium if they are highly vascular or if there is breakdown of the blood brain barrier. There are patients with non-enhancing lesions who had toxoplasmosis. This is explained by the fact that failure of capsule formation around toxoplasmosis abscesses in extreme immune-suppression, 5 % of these lesions do not enhance. Lack of enhancement in cerebral toxoplasmosis encephalitis is a poor prognostic sign [21]. Hypodense periventricular white matter lesions without contrast enhancement are diagnostic of encephalitis. When these CT signs are clinically associated with rapidly progressing dementia, PML (progressive multifocal leukoencephalopathy) is the likely cause [22]. In one patient with PML we confirmed the diagnosis at postmortem with histological.







