Fig. 6.1
The main nervous supply to the facet joints is from nerves arising from the medial branches of the dorsal rami of the spinal nerves. Articular branches are given off both to the facet joint at the same level and to the joint below the level of each spinal nerve
The L5 nerve differs because it is the dorsal ramus itself that runs along the sacral ala, while its medial branch arises opposite the inferolateral corner of the lowest facet joint. This anatomical difference has to be taken into account when treating at this level, because the dorsal ramus itself rather than its medial branch has to be the target of the therapeutic intervention.
6.1.3 Patients’ Selection for Percutaneous Procedures
The lumbar facet joint syndrome is the main indication for interventional procedures on zygapophysial joints. This condition mainly affects elderly people because osteoarthritis degenerative lesions, secondary to abnormal articular load or to repetitive stress injury, frequently cause it.
Other causes can determine facet joint syndrome such as synovitis and joint effusion (due to unspecific inflammation or post-trauma), chondromalacia, joint capsule mechanical trauma, entrapment of meniscal structures, synovial impingement, articular subluxation and compression.
Also the instability of posterior arch may be associated with lumbar pain.
From a clinical point of view, this syndrome is not easy to diagnose because of its similarity to other spinal painful condition and, above all, because lumbar pain is generally caused by several factors. The most common symptom is median lumbar pain, which may be irradiated to gluteal regions and posteriorly in the thigh, without a precise dermatomeric distribution. Usually it does not irradiate to the inferior limb below the knee.
It is described that in some patients para-articular synovial cysts occur and these can determine radicular compression; therefore in these cases it is suggested to aspirate under CT guidance. Patients with cervical facet joint disease more often complain of a para-vertebral pain that increase with twisting movements and may be irradiated to the shoulder and headache.
In typical cases, x-ray films show degenerative changes and a limitation in the range of flexion/extension, whereas CT and MRI scans show spondylitis and asymmetry in the articular rim orientation, when present. In patients with exacerbation of pain, MRI may show joint effusion (especially in patients with joint instability) and bone oedema. Paramagnetic contrast enhancement may show uptake not only in the involved joints but also in the surrounding soft tissue (Fig. 6.2). In patients with lumbar pain and joint instability MRI performed with the patient in standing position may reveal joint subluxation and/or join effusion.
Fig. 6.2
The MR after gadolinium shows the enhancement in the painful facet joint and in the closer soft tissues
To make a correct diagnosis is important to consider both clinical and imaging data. In dubious cases, it could be correct to perform a diagnostic anaesthetic nerve block. In most of cases, anaesthetic injections are performed to alleviate the pain, and they may be repeated in case of persistence or relapse of the pain. Anaesthetic nerve block is also a useful diagnostic tool in dubious cases. It is important to underline that medial branch neurotomy should be used in those patient with chronic pain derived from facet joints, in the attempt to achieve a long-lasting analgesia. This procedure always follows a positive diagnostic block [5]. Clear contraindications are uncommon and include coagulation disorders, local infections and hypersensitivity to the medication, whereas relative contraindications include those relative to iodine contrast enhancer (which may be avoided in the majority of cases) or steroids.
Injection procedures are performed in ordinary outpatient clinics or in day surgery, under local anaesthesia, and do not need particular patient preparation. Neurolysis procedures, on the other hand, may require sedation of the patient and therefore are better performed in a day hospital setting.
6.1.4 Diagnostic Blocks
Nerve block tests are usually performed by injecting 1 ml of lidocaine in correspondence of the tender joints; the relief of the pain in two repeated blocks, 1 week apart, is considered as a good prognostic factor for successful RFD procedure. Several guidelines and reviews have asserted that diagnostic blocks are very important in diagnosing facet-related pain [6–8], although false-positive and false-negative blocks were described [9, 10].
6.1.5 Radiofrequency Denervation (RFD)
The procedure should be performed in day surgery under CT or fluoroscopic guidance with the patient lying in prone position (Fig. 6.3). Oblique view under fluoroscopic guide allows a good visualisation of the target point for needle positioning, the groove between the transverse and the articular process. At that site lies the medial arm of the dorsal branch of the spinal nerve, before splitting in the two terminal nerves, allowing the positioning of the needle, parallel to the nerve in optimal position.
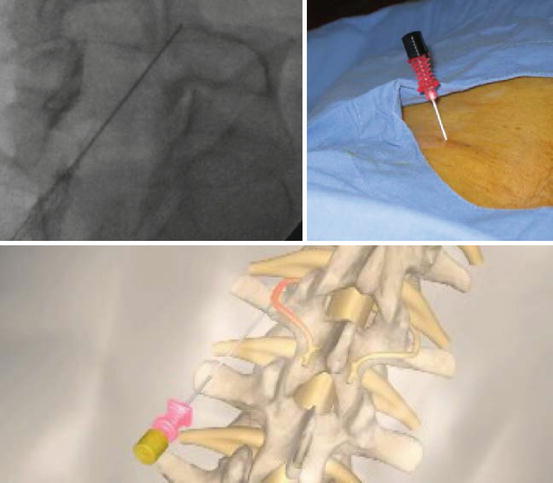
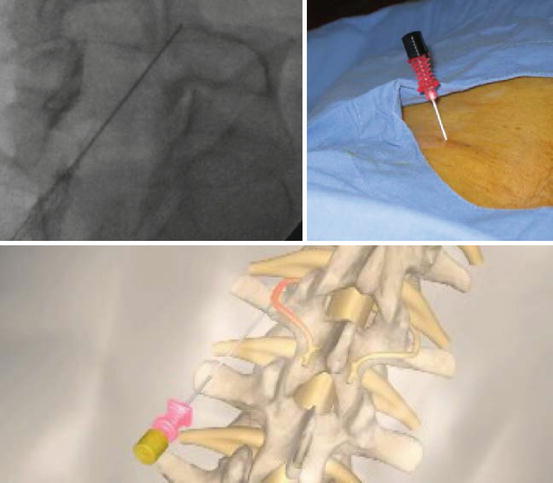
Fig. 6.3
Correct positioning of the needle under fluoroscopic guidance using the oblique view: in the groove between the transverse and the articular process, as parallel as possible to the nerve with caudal–cephalad direction
As we previously discussed in the anatomy paragraph, for L5 nerves, the dorsal ramus rather than its medial branch is approached on the ala of the sacrum just lateral to the articular process because of anatomical differences.
After that, 1 ml of lidocaine should be administered percutaneously before the introduction of the 22 gauge, 10 cm long with 10 mm exposed tip needle (Fig. 6.4). When the positioning of the needle is correct (with the confirmation of the AL and LL view under the fluoroscopic guide), the electrode is introduced and impedance values between 250 and 800 Ω indicate the correct position of the needle. In order to confirm the proximity to the medial branch, sensorial stimulation tests are performed using 50 Hz and 0.2–0.7 V, reproducing the typical pain of the patient. Motor stimulation tests (2 Hz, 1 V) are also performed in order to avoid motor lesions.


Fig. 6.4
Correct positioning of the needle under fluoroscopic guidance using the oblique and the AP views to approach the L5 dorsal ramus: on the ala of the sacrum just lateral to the articular process
After this check, paying particular attention to moving the electrode needle, the nerve is ablated by reaching 90 °C for 60 s. Thermoablation is then performed on the medial branch of the contiguous level, according to the neuroanatomy. In case of two close joints, three levels have to be treated (Fig. 6.5).


Fig. 6.5
After performing sensory and motor stimulation tests, it is possible to do safely the ablation. The recommended parameter for CRF is 90 °C for 60″
Some new-generation RF machines allow the ablation of more (maximum four) branches at the same time. Moreover, it is also possible to perform pulsed radiofrequency neurotomy by using 42 °C for 140 s. No statistically significant differences were demonstrated between the two techniques but usually greater improvement over time with CRF [11]. After the procedure the patients are monitored 2 h in hospital and then dismissed.
6.1.6 Complications
The occurrence of severe complications following facet joints procedures is quite uncommon, considering both intra-articular injections and diagnostic block, as well as radiofrequency denervation.
Sometimes it is possible to find metabolic and endocrine effects that are caused by the depot of steroids injection; however suppression of the hypothalamic–pituitary–adrenal axis has to be considered, as well as impaired insulin sensitivity causing elevated glucose levels [12].
Another complication of intra-articular injection is the occurrence of infection, even if septic arthritis, epidural abscess and meningitis rarely occur after facet joint injections [13, 14]. Goldstone et al. [15] reported the occurrence of anaesthesia and headache.
Further potential side effects after radiofrequency denervation could be numbness and/or dysaesthesias, although they tend to be transient and self-limiting [16]. Burning sensations are uncommon with radiofrequency procedures and may result from electrical faults or equipment malfunction [17].
Neuritis is considered as the commonest adverse reaction following facet joint radiofrequency, with a reported incidence of 5 % [18]. Authors have suggested that the administration of corticosteroid or pentoxifylline has been reported to be able to reduce the occurrence of post-procedure pain [19].
The prevalence of chronic, recurrent neck pain is approximately 15 % of the adult general population. Controlled studies have supported the existence of cervical facet or zygapophysial joint pain in 36–67 % of these patients. Cervical RFN can be performed as well under continuous fluoroscopic guidance, but the use of the CT could avoid injuries of the vertebral artery (Fig. 6.6).
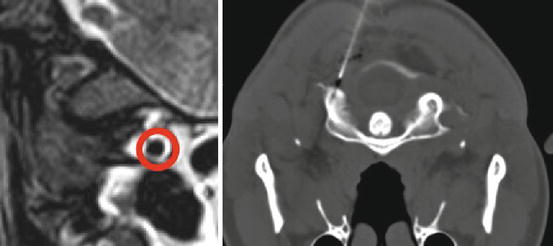
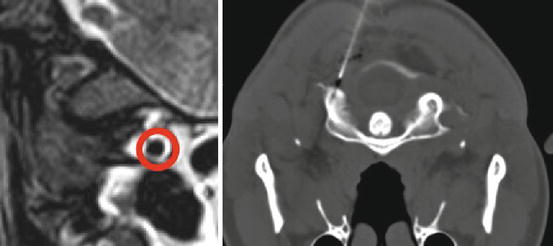
Fig. 6.6
CT guidance for cervical RFN allows a better visualisation of the vertebral artery
6.1.7 Follow-Up
It is important to remember that radiofrequency denervation, in patients with a positive response to at least a nerve block test, is generally followed by a prolonged therapeutic effect, both as pain relief and function improvement [20, 21]. Nevertheless, data from the past literature about this topic are conflicting. Many papers assessed the efficacy of lumbar RFN, but only few met the criteria for the clinical evidence: in fact, based on 6 positive randomised trials and 10 positive observational studies, the evidence for conventional radiofrequency neurotomy in managing of the chronic low back pain of facet joint origin in the lumbar spine is good for short- and long-term relief. Based on one randomised trial and one observational study meeting inclusion criteria, the evidence is limited for pulsed radiofrequency neurotomy for managing chronic low back pain of facet joint origin [22].
Several papers also showed the efficacy of cervical facet RF neurotomy [23–33]; similar to previous evaluations, radiofrequency neurotomy showed significant evidence even if it has not reached the good evidence level due to the lack of high-quality randomised trials for both short-term and long-term improvement. Data based from a prospective, randomised, double-blind trial and five moderate-quality observational studies suggested that the evidence for cervical radiofrequency neurotomy is fair [34, 35].
6.2 Sacroiliac Radiofrequency Neurotomy
6.2.1 Painful Sacroiliac Dysfunction
Low back pain has a high lifetime incidence, coming to affect between 80 and 90 % of the general population during their lifetime, and in up to 47 % of cases, it can be attributed to painful sacroiliac (SI) dysfunction. In case of pain suspected to originate from sacroiliac joints, several passive joint mobilisation tests are available, such as distraction test, compression test, Patrick’s (FABER) test, thigh trust, and Gaenslen’s test.
To effectively understand the concept of SI dysfunction, it is necessary to know the concepts of “form closure” and “force closure”, expressed for the first time by Snijders, Vleeming and Stoeckhart [36, 37]. The “form closure” consists in stabilising the joint that is realised at the SI level due to the friction present between the articular surfaces, obtained by the effect of (a) perfect complementarity between ridges (sacral slope) and trenches (pelvic side) facing each other on the articular surface, (b) different composition of the opposing surfaces (articular cartilage on the sacral side and fibrocartilage on the iliac), (c) almost perfectly vertical spatial orientation of the articular surfaces and (d) action of intrinsic and extrinsic ligaments. The “force closure” contributes to the dynamic stabilisation of the joint, creating at this level an additional force of closure of the articular chain of the pelvis. Three distinct systems participate, namely, (a) passive (capsule, ligaments), (b) active (stabilising muscles) and (c) control (purely neurological). Three major frameworks of joint dysfunction are distinct, which collect many different aetiologies with similar results (for each category of dysfunction) on joint biomechanics and different clinical manifestations; we can distinguish (a) Postural dysfunction: observed as a result of an alteration in length or in the pattern of muscle activation; an example of such pathogenetic mechanism is represented by the postural dysfunction of the SIJ that is realised in the cases of disproportion of the lower limbs. (b) Hypomobility dysfunction: arises as a result of microtrauma and degenerative or inflammatory processes that cause joint stiffness or malposition. (c) Instability dysfunction: derives from the impairment of one or more elements contributing to determine the form and/or force closure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








