3 Current context
neurological rehabilitation and neurological physiotherapy
Introduction
Neurological conditions are those conditions which affect parts of the nervous system. The causes of these conditions are varied and may include trauma, vascular disruption, infection, tumour or degeneration of the nervous system. Conditions may affect the central nervous system, consisting of the brain and spinal cord, or the peripheral nervous system, consisting of the peripheral nerves (Table 3.1). Neurological conditions are often complex, and people with these conditions may require support from many different services. Acupuncture may provide benefits for people with neurological conditions, but it represents just one possible option among many. An awareness of the important aspects of a comprehensive service for people with neurological conditions is important. This chapter aims to outline the various components that are required for effective management of people with neurological conditions.
Table 3.1 Examples of common neurological conditions
| Central nervous system | Peripheral nervous system |
|---|---|
Prevalence and incidence of neurological conditions
Neurological conditions are common. Around 10 million people in the UK live with a neurological condition which substantially affects their life [1]. Stroke is by far the commonest neurological condition. Each year, around 125 000 people in the UK, 700 000 in the USA and 1 million in the European Union have a stroke [2]. In the UK, of those individuals with neurological conditions, around 350 000 require help for most of their daily activities, and over 1 million require assistance with some daily tasks [1]. Each year 1% of the UK population are newly diagnosed with a neurological condition and 19% of hospital admissions are for a neurological problem requiring treatment from a neurologist or neurosurgeon [1].
Models of health care
Medical model
The medical model assumes that all illnesses are explained by disease and that the treatment of disease will restore the individual to health [3]. This model was originally developed in the late 19th and early 20th centuries following the scientific discoveries of infectious disease by Pasteur and cellular pathology by Virchow [4]. The medical model is based on reductionism and a dualistic notion of the mind and body. It evaluates individuals in isolation from their environment and takes no account of the social, psychological or behavioural aspects of illness or the patient’s experience of that illness [5, 6]. It was originally developed for the management of severe medical conditions. In these situations treatment of the disease may indeed result in substantial improvements in health. However, with the growing prevalence of chronic disease, the inadequacies of this model are highlighted. The model cannot explain symptoms for which there is no underlying pathology. It also fails to appreciate the complex interaction of social, psychological and environmental factors and their impact on the overall experience of illness by the individual.
Biopsychosocial model
The biopsychosocial model considers individuals as well as their health problem and the social context. It recognizes that health, disease, illness and disability result from complex interactions of biological, emotional, cognitive, social and environmental factors. It recognizes that psychological and social factors influence the person’s perceptions and actions, and therefore the experience of illness. This model suggests that effective treatment of the disease may not automatically result in the resolution of illness and disability. This model has been adopted by the World Health Organization as the basis for the International Classification of Function (ICF) [7].
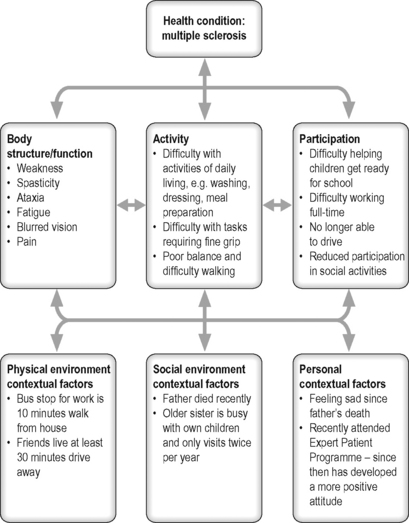
Presentation of neurological conditions and ICF
Neurological conditions may result in a wide range of difficulties. These may include problems with physical ability, sensation, cognition, communication, behaviour and psychological functioning. The ICF developed by the World Health Organization [7] provides a useful framework to classify the consequences of disease (Figure 3.1) [8]. It is based on the biopsychosocial model of disability and supports the consideration of an individual’s situation within the context of biological factors and also the social and physical environment.
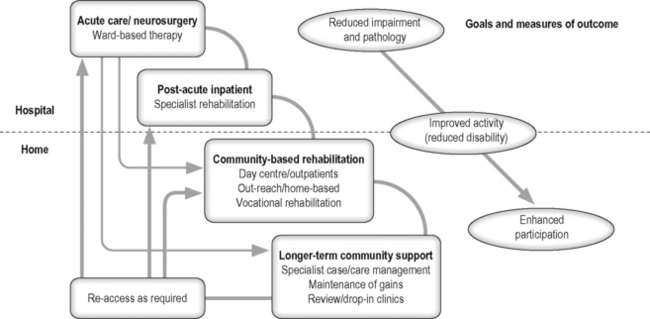
General principles of rehabilitation
Rehabilitation has been defined as: ‘the use of all means aimed at reducing the impact of disabling and handicapping conditions and at enabling people with disabilities to achieve optimal social integration’ [10]. Rehabilitation is a continuous and coordinated process which starts at the onset of an illness or injury and aims to support individuals to achieve roles in society consistent with their aspirations [8]. Many individuals with neurological conditions will require access to rehabilitation services. Support needs to be provided for individuals throughout their life. Clear mechanisms for individuals to re-access relevant services are required (Figure 3.2). In addition palliative care is required to support individuals coming to the end of their lives [11].
Key aspects of effective rehabilitation
Person-centred service
The person should be at the centre of the service provided. Individuals should be provided with sufficient information about treatment options to allow them to be actively involved in all decisions regarding their management [9]. Information provided needs to take account of any communication difficulties that the individual may have. Attention should be paid to the person’s emotional needs as well as practical needs. Support should also be provided to family members and carers [9].
Specialist multidisciplinary team
Access to a coordinated specialist rehabilitation team is an important factor in effective management of the wide range of difficulties an individual may report [12, 13]. The specialist team members should include a doctor, nurse, physiotherapist, occupational therapist, speech and language therapist, clinical psychologist and social worker. Access to the expertise of other services is also important. Such services include dietetics, continence advisory service, orthotics, chiropody, pain management and spasticity management services, ophthalmology and liaison psychiatry.
Goal-setting
Goal-setting is an integral part of rehabilitation and allows the person and the specialist team to focus on key aspects identified as important by the individual [14]. Goals are specific time-bound measurable outcomes relating to a desired or expected future state. Goals are set by the individual, with support from the relevant team members. They guide and inform therapy, as well as providing a structure for the individual regarding future targeted outcomes [15]. Goals need to be challenging but achievable and include long-term (weeks/months) and short-term goals (days/weeks) [12].
Outcome measures
Outcome measures provide information regarding the outcome for an individual following rehabilitation. The use of validated standardized outcome measures is required within rehabilitation services to provide information on individual outcomes, as well as to allow service evaluation [16]. A wide range of outcomes measures have been validated, and they include those that reflect the perspective of the person as well as the clinician [17].
Evidence-based practice
Management programmes for people with neurological conditions need to be based on best available evidence. Evidence-based practice involves the integration of individual clinical expertise with the findings from the best available research [18]. A range of clinical guidelines have been developed to support improved care of people with conditions such as stroke or multiple sclerosis. Guidelines have been based on an extensive review of available research evidence combined with expert opinion [12, 13, 19, 20].
Chronic disease management
Chronic disease
Chronic diseases are diseases of long duration and usually slow progress. They are the leading cause of death and disability worldwide [21]. Many neurological conditions are chronic diseases requiring management over time. These diseases often have a range of persistent symptoms with no cure and the potential for significant impact on the individual’s quality of life [22]. Successful management requires an effective collaboration between the person and relevant health and social care professionals.
The ‘expert patient’
Over time individuals with chronic conditions develop considerable knowledge and experience about their condition and how it affects their life. This expertise has not always been utilized fully within management decisions. There is now a shift in emphasis to support these individuals to be key decision-makers in collaboration with health care professionals [23]. Self-management programmes are supporting this process of the development of ‘expert patients’ [24].