(1)
Department of Neurosurgery, University Medicine Greifswald, Greifswald, Germany
Abstract
Endoscope-assisted microsurgery combines the advantages of the microscope with those of the endoscope. For dissection of structures which are visible in a straight line, the microscope with high resolution, excellent color fidelity, and stereoscopic vision is used. For working “around a corner,” the endoscope is applied to reduce the amount of retraction and skull base drilling.
For endoscope-assisted procedures, endoscopes with angulated eye pieces are preferred to bring the video camera away from the surgical field and avoid interference with the surgical instrument. Various angles of view (0°, 30°, 45°, and 70°) are available to be able to inspect any corner. The endoscope outer diameter should not exceed 4 mm. For the cerebellopontine angle 2.7 mm scopes are recommended because of the narrow spaces between the cranial nerves in this area. Angulated instruments are required for removing tumor tissue around a corner.
In endoscope-assisted microsurgery, usually the major part of the procedure is performed under microscopic view because of the better image quality and the 3D view. However, certain steps of the surgery are carried out under endoscopic view. The endoscope is mostly used to look around bony or dural corners as well as neurovascular structures to avoid extensive skull base drilling and retraction. Furthermore, the endoscope is applied in deep and narrow surgical corridors to improve illumination and viewing field. Frequently, the endoscope is used freehand simply for inspection. However, when bimanual dissection is required, the endoscope is fixed to a self-retaining holding device, and the surgeon has both hands free for manipulation.
The endoscope-assisted technique has proven useful in skull base tumor surgery (acoustic neuromas, epidermoids), aneurysm clipping, and trigeminal microvascular decompression.
6.1 Introduction
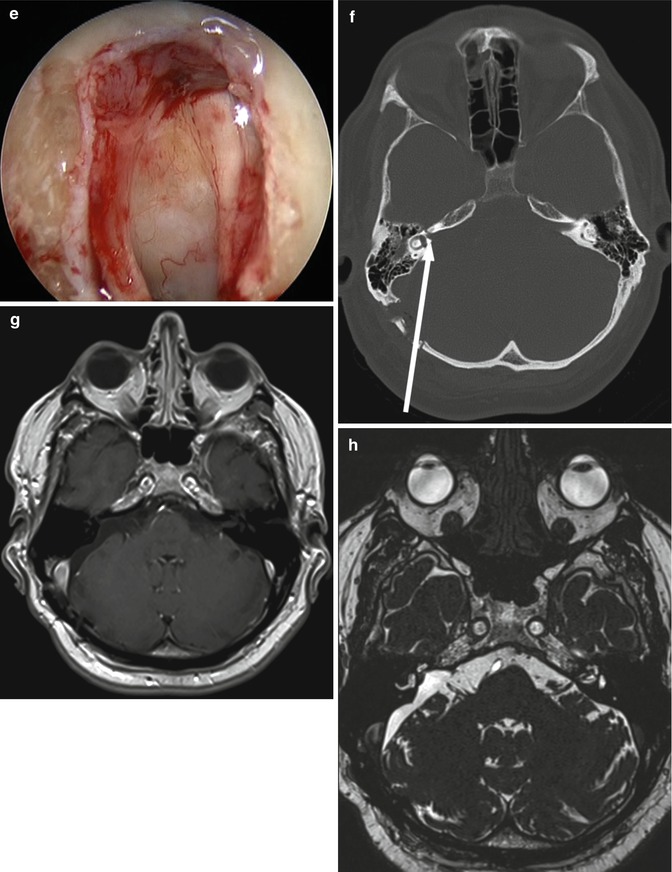
The use of the operating microscope in neurosurgery has been well established since more than 30 years. A major improvement in surgical results has been obtained by using microsurgical techniques. Especially in complex skull base and vascular surgery, the microscope is a prerequisite to achieve excellent outcomes for the patients. The microscope provides a superb stereoscopic view. However, in deep and narrow surgical corridors, there is a considerable loss of light at the entry site (Fig. 6.1a). Furthermore, the surgeon is working within the light beam which further decreases the light intensity in the surgical field. With the microscope, only structures which are visible in a straight line can be explored.
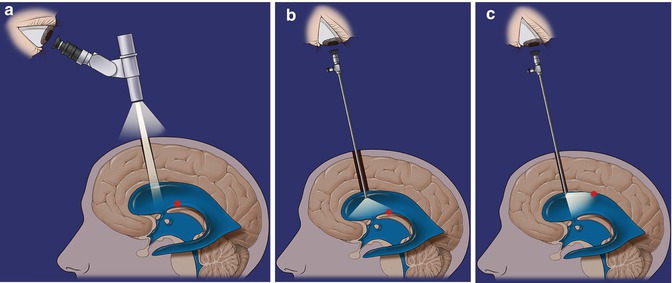
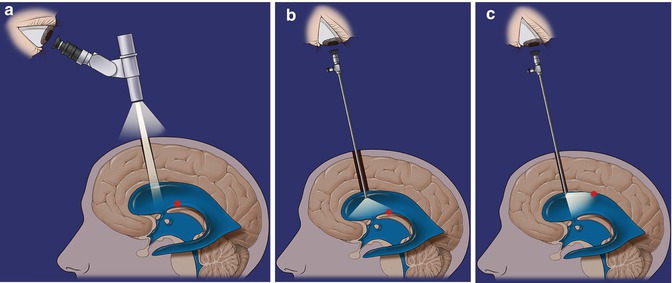
Fig. 6.1
Schematic drawing of microscopic and endoscopic visualization. (a) Microscopic visualization. (b) Endoscopic 0° visualization. (c) Endoscopic 45° visualization
6.2 Rationale of Endoscope-Assisted Microsurgery
Compared with the operating microscope, the endoscope provides a completely different view. “State-of-the-art” endoscopes containing a Hopkins II® rod lens have a wide angle viewing field resulting in a panoramic view (Fig. 6.1b). Therefore, even lesions which are not located in front of the endoscope tip can be recognized early. This is a major advantage in narrow and deep surgical approaches. Using endoscopes with angulated optics gives the ability to look around a corner or behind neurovascular structures which is very useful in skull base surgery (Fig. 6.1c). With the use of the endoscope, the surgeon brings the eye close to the target area with perfect illumination even in the depth. Another important advantage of the endoscope compared with the microscope is the excellent depth of field. Refocusing which is frequently required with the microscope particularly with high magnification is rarely necessary.
Of course, the endoscope has also limitations. The major drawback of the endoscope is the lack of true 3D viewing. However, because of the fish-eye effect, the endoscopic image is distorted and provides a pseudo 3D impression. Furthermore, motion parallax which means closer objects move more than distal objects contributes to the pseudo 3D impression of an endoscopic image. Therefore, the lack of stereopsis is usually compensated for with some training. Another disadvantage of the endoscope is the lower resolution compared to the microscope. Because of the smaller lens diameter of the endoscopes used in neuroendoscopy, the operating microscope has still better resolution than the endoscope. Furthermore, when using the operating microscope, the surgeon has a very good resolution because he is looking directly through the lens system. The sensor is the retina which is much better then CCD chips in the mini video cameras which are attached to the endoscope. Although recently introduced high-definition cameras generate images with 1080 lines and over two million pixels, the image quality is still inferior when comparing with the direct look of the human eye through the microscope.
In conclusion, microscope as well as endoscope has advantages and disadvantages. Therefore, it sounds reasonable to combine the advantages of both optical instruments during neurosurgery.
6.3 Endoscopic Equipment
For endoscope-assisted procedures endoscopes with angulated eye pieces are preferred to bring the video camera away from the surgical field and avoid interference with the surgical instruments (Fig. 6.2). Various angles of view (0°, 30°, 45°, and 70°) are available to be able to inspect any corner. The endoscope outer diameter should not exceed 4 mm. For the cerebellopontine angle 2.7 mm scopes are recommended because of the narrow spaces between the cranial nerves in this area. Angulated instruments are required for removing tumor tissue around a corner (Fig. 6.3). Xenon light sources provide the best illumination, since the color temperature of xenon light resembles that of sunlight (6,000 K) which improves the color fidelity. High-definition (HD) video cameras should be used whenever possible as the image quality is much better compared with the standard cameras [12].

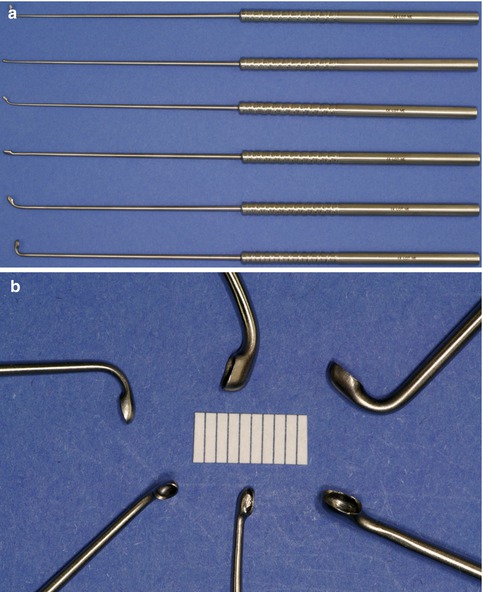

Fig. 6.2
Endoscopes with angulated eyepiece with 0°, 30°, and 70° of view
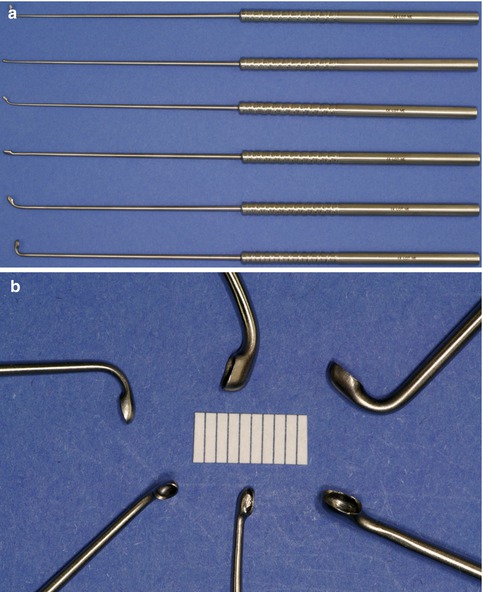
Fig. 6.3
Instruments for endoscope-assisted surgery with angulated tips. (a) Curettes of various sizes. (b) Close-up view of the tips
6.4 Surgical Technique
In endoscope-assisted microsurgery, usually the major part of the procedure is performed under microscopic view because of the better image quality and the 3D view. However, certain steps of the surgery are carried out under endoscopic view. The endoscope is mostly used to look around bony or dural corners as well as neurovascular structures to avoid extensive skull base drilling and retraction. Furthermore, the endoscope is applied in deep and narrow surgical corridors to improve illumination and viewing field.
Frequently, the endoscope is used freehand simply for inspection (Fig. 6.4a). However, when bimanual dissection is required, the endoscope is fixed to a self-retaining holding device, and the surgeon has both hands free for manipulation (Fig. 6.4b, c). The monitor is placed straight in front of the surgeon for ergonomic purposes (Fig. 6.4d).
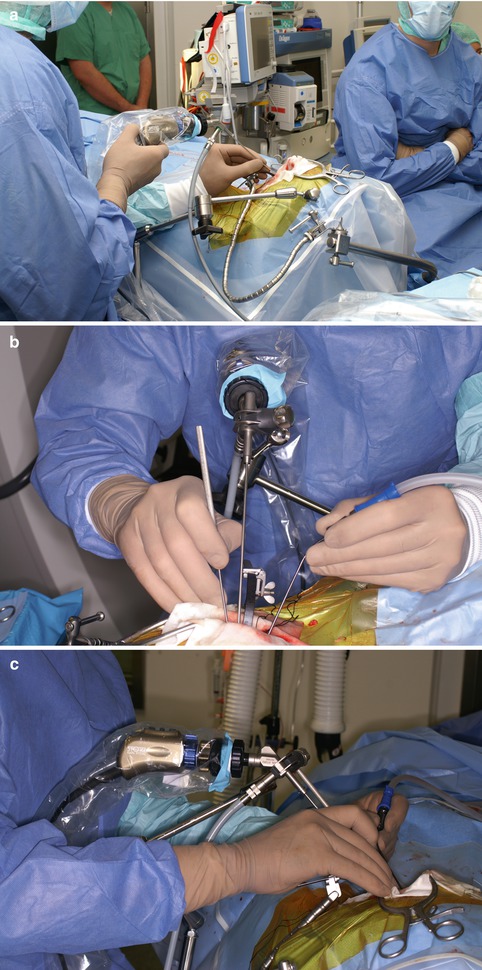

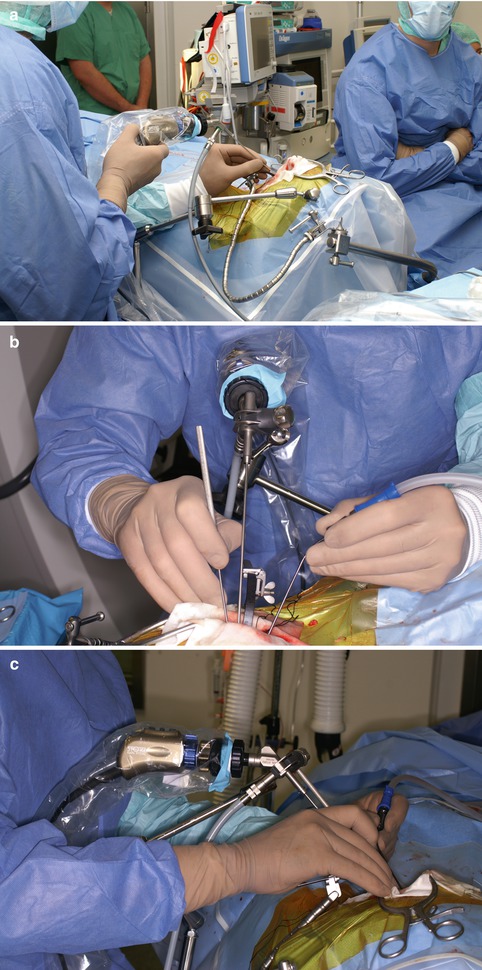

Fig. 6.4
Use of endoscopes in endoscope-assisted procedures. (a) Freehand endoscopic inspection. (b, c) Bimanual endoscopic dissection. Endoscope with self-retaining holding arm. (d) Ergonomic positioning of the screen in straight line in front of the surgeon
Care has to be taken when moving the endoscope and inserting or removing the instruments from the surgical field to avoid damage to neurovascular structures which are behind the tip of the endoscope and therefore not under endoscopic view. It is important to keep in mind that the tip of the endoscopes may become really hot which may damage neurovascular structures especially during prolonged dissections under endoscopic view. Therefore, frequent irrigation is recommended.
6.5 Indications
The endoscope-assisted technique has turned out to be particularly useful in skull base tumor surgery, aneurysm clipping, and microvascular decompression [1–11, 13, 14].
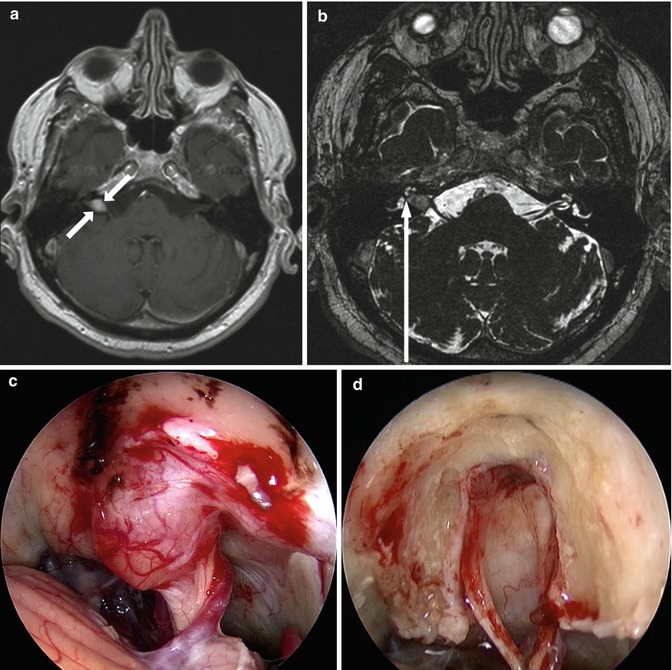
6.5.1 Vestibular Schwannomas
Vestibular schwannomas with tumor extension deeply into the internal auditory canal are good indications for an endoscope-assisted retrosigmoid approach (Fig. 6.5). When hearing preservation is demanded, the extent of drilling of the posterior wall of the internal auditory canal is limited by the vestibule and the posterior semicircular canal. The angle of viewing does not allow the direct inspection of the fundus of the internal auditory canal with the aid of the microscope even after extensive drilling of the posterior wall of the internal auditory canal (Fig. 6.5f). Therefore, very often a blind dissection of the distal tumor pole is performed with the aid of a hook dissector. Using a 30°, 45°, and 70° endoscope enables a perfect visualization of the fundus (Fig. 6.5e). The endoscope can be used freehand for inspection after tumor removal to make sure that the tumor is totally removed or for dissection of the tumor in the fundus. After tumor removal, the drilled area of the internal auditory canal is inspected to find open air cells which might cause CSF leak (Fig. 6.5d).