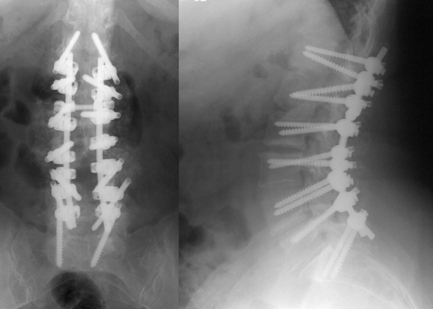
49 A 59-year-old woman complains of mechanical back pain with radiculopathy that has been ongoing for a year, despite nonsurgical treatment. On examination she had antalgic weakness of the right hip flexors and extensors and limited lumbosacral flexion. Magnetic resonance imaging (MRI) (T2-weighted sagittal, Fig. 49-1) showed degenerative scoliosis from L1 to S1 with degenerative disc disease. Postoperative lumbar x-ray (Fig. 49-2) reveals T12-S1 pedicle screw fixation with cross-linkage. FIGURE 49-1 MRI of the lumbar spine shows a scoliotic spine with spondylostenosis. Degenerative scoliosis A multilevel decompression and T12 to S1 pedicle screw fixation using iliac crest graft and a bone stimulator were completed. The patient’s preoperative pain resolved. Mechanical back pain has many etiologies, including sco-liosis. Degenerative scoliosis is the end result of advanced degenerative spine disease. As wear and tear increases on the discs, excessive motion ear stress a preexisting deformity. It is not uncommon for people to present with unilateral multilevel radiculopathies secondary to the biomechanics of the concavity. Treatment options for degenerative scoliosis depend on the patient’s symptoms. Mechanical lower back pain, the presence of neurologic symptoms or radiculopathy, the type of curve, and the overall clinical condition are factors to consider. If the main presentation is that of radiculopathy, decompression alone or with a short segmental fusion may suffice in an elderly patient with focal instability and suboptimal health status. On the other hand, in a younger, healthier patient presenting with significant mechanical low back pain and instability (a lateral, anterior, or rotational listhesis), a reconstructive multilevel segmental fusion is a good option. Either way, assessment of sagittal balance will drive the treatment plan. A posterior approach alone is appropriate in a milder, less rigid curve and when severe canal stenosis is encountered. An anteroposterior (AP) approach has the advantages of restoring anatomic balance and disc and foraminal height, and achieves a superior fusion rate. This combined approach is recommended in stiff, less reducible curves with somewhat more osteopenic bone quality. A dramatic increase in surgical risk is encountered in patients over 60 years of age. For this population, the nutritional status pre- and postfusion should be optimized. Beware of the use of any anticoagulation (Coumadin, heparin, Lovenox, etc.), and encourage early mobilization. Intraoperative monitoring as well as the intraoperative wake-up test are valuable resources. Special attention to the caudal aspect of arthrodesis is necessary, as there is a pattern of failure relating to the lower part of the fusion.
Degenerative Scoliosis
Presentation
Radiologic Findings

Diagnosis
Treatment
Discussion
Degenerative Scoliosis
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








