Delirium, Dementia, and Amnestic and Other Cognitive Disorders and Mental Disorders Due to a General Medical Condition
Cognition includes language, memory, judgment, orientation, conducting interpersonal relationships, performing actions (praxis), and problem solving. Cognitive disorders reflect disruption in one or more of these domains, and are frequently complicated by behavioral symptoms. These disorders include delirium, dementia, and amnestic disorders. Although other psychiatric disorders can exhibit some cognitive impairment as a symptom, with the aforementioned disorders, cognitive impairment is the cardinal symptom.
Delirium is marked by short-term confusion and changes in cognition. It is a life-threatening yet potentially reversible disorder of the central nervous system that often involves perceptual disturbances, abnormal psychomotor activity, sleep cycle impairment, and a waxing and waning level of consciousness. It is not a disease but rather a syndrome and has many causes, all of which result in similar patterns of signs and symptoms relating to the patient’s level of consciousness and cognitive impairment.
Dementia is marked by severe impairment of memory, judgment, orientation, and cognition. Unlike delirium, deficits in dementia occur in the context of a clear sensorium. The critical clinical points of dementia are the identification of the syndrome and the clinical workup of its cause.
Amnestic disorder is marked by memory impairment and forgetfulness. Memory impairments are associated with significant deficits in social or occupational functioning. Amnestic disorders are causally related to general medical conditions, such as head trauma. This characteristic distinguishes them from the dissociative disorders involving memory impairments.
The questions and answers below can test knowledge of the subject.
Helpful Hints
Students should be able to define the signs, symptoms, and syndromes listed below.
Addison’s disease
AIP
ALS
amnestic disorders
anxiety disorder due to a general medical condition
auditory, olfactory, and visual hallucinations
beclouded dementia
beriberi
black patch
catastrophic reaction
cognitive disorders
confabulation
cretinism
Creutzfeldt-Jakob disease
Cushing’s syndrome
delirium
delusional disorder
dementia
dementia of the Alzheimer’s type
diabetic ketoacidosis
Down syndrome
dysarthria
epilepsy
general paresis
granulovacuolar degeneration
Huntington’s disease
hypnagogic and hypnopompic hallucinations
hypoglycemic, hepatic, and uremic encephalopathy
interictal
intoxication and withdrawal
intracranial neoplasms
Korsakoff’s syndrome
kuru
Lilliputian hallucinations
memory
mild cognitive impairment
mood disorder due to a general medical condition
multiple sclerosis
myxedema
neurofibrillary tangles
normal aging
normal-pressure hydrocephalus
parkinsonism
partial versus generalized seizures
pellagra
pernicious anemia
personality change due to a general medical condition
Pick’s disease
prion disease
pseudobulbar palsy
pseudodementia
retrograde versus anterograde amnesia
senile plaques
short-term versus longterm memory loss
sundowner syndrome
systemic lupus erythematosus
tactile or haptic hallucinations
transient global amnesia
transient ischemic attack
vascular dementia
vertebrobasilar disease
Questions
Directions
Each of the questions or incomplete statements below is followed by five suggested responses or completions. Select the one that is best in each case.
10.1. Which statement below about the interrelationship between delirium and dementia is true?
A. Delirium is a risk factor for the development of dementia.
B. Fully two-thirds of cases of dementia occur in patients with delirium.
C. The vulnerability of the brain in patients with dementia may predispose the patient to delirium.
D. Dementia contributes to a loss of independence among patients with delirium.
E. Dementia can alter the course of an underlying delirium.
View Answer
10.1. The answer is C
Delirium and dementia are highly interrelated. Dementia is the leading risk factor for delirium (not vice versa), and fully two-thirds of cases of delirium occur in patients with dementia (not vice versa). Thus, the underlying vulnerability of the brain in patients with dementia may predispose them to the development of delirium as a result of insults related to acute medical illnesses, medications, or environmental perturbations.
Delirium is defined by the acute onset of fluctuating cognitive impairment and a disturbance of consciousness. The hallmark symptom is an impairment of consciousness, usually occurring in association with global impairments of cognitive functions. Dementia is defined as progressive impairment of cognitive functions occurring in clear consciousness (i.e., in the absence of delirium). Global impairment of intellect is the essential feature, manifested as difficulty with memory, attention, thinking, and comprehension. Although it is not likely that delirium itself causes the pathological change in dementia, there is no question that delirium (not dementia) contributes to worsening functional status, loss of independence, and poorer outcome among patients with dementia. Delirium can alter the course of an underlying dementia, with dramatic worsening of the trajectory of cognitive decline, resulting in more rapid progression of functional losses and worse long-term outcomes.
10.2. Alzheimer’s dementia is
A. associated with hypoactive levels of acetylcholine
B. associated with pathognomonic neurofibrillary tangles
C. more common in men
D. linked to chromosome 7
E. a clinical diagnosis
View Answer
10.2. The answer is A
The neurotransmitters that are most often implicated in the pathophysiological condition of Alzheimer’s disease are acetylcholine and norepinephrine, both of which are hypoactive in the disease. The disease has shown linkage to chromosomes 1, 14, and 21, not chromosome 7. Although it is commonly diagnosed in the clinical setting after other causes of dementia have been excluded, the final diagnosis of Alzheimer’s disease requires a brain biopsy. The classic gross neuroanatomical observation of the brain from patients with this disease is diffuse atrophy. The classic microscopic findings are senile plaques, neuronal loss, synaptic loss, and granulovascular degeneration of the neurons. Neurofibrillary tangles are not unique to Alzheimer’s disease but also occur in Down syndrome, dementia pugilistica, Parkinson-dementia complex of Guam, and the brains of normal people as they age. The risk factors for developing Alzheimer’s dementia include being female, having a first-degree relative with the disorder, and having a history of head injury.
10.3. Creutzfeldt-Jakob disease is characterized by
A. rapid deterioration
B. myoclonus
C. diffuse, symmetric, rhythmic slow waves and sharp spikes in EEG
D. postmortem definitive diagnosis
E. all of the above
View Answer
10.3. The answer is E (all)
Creutzfeldt-Jakob disease is an infection that causes a rapidly progressive cortical-pattern dementia. The infectious agent, a prion, is a subviral replicative protein that is now known to cause a variety of so-called spongiform diseases in animals and humans. The age at onset of Creutzfeldt-Jakob disease is usually in the sixth or seventh decade of life, although onset can occur at any age. The incidence is one in 1,000,000. The clinical symptoms vary with progression of the illness and depend on the regions of the brain that become involved. Patients may present initially with nonspecific symptoms, including lethargy, depression, and fatigue. Within weeks, however, more fulminant symptoms develop, including progressive cortical-pattern dementia, myoclonus, and pyramidal and extrapyramidal signs. Although blood, cerebrospinal fluid, and imaging studies are unremarkable, the electroencephalogram (EEG) may demonstrate a characteristic pattern of diffuse, symmetric, rhythmic slow waves and sharp spikes. A presentation with rapid deterioration, myoclonus, and the characteristic EEG pattern should raise suspicion of Creutzfeldt-Jakob disease. The definitive diagnosis is made by postmortem microscopic examination, which demonstrates spongiform neural degeneration and gliosis throughout the cortical and subcortical gray matter; white matter tracts are usually spared. Prion disease can incubate for decades before the emergence of clinical symptoms and subsequent rapid progression. Reported routes of transmission include invasive body contacts, such as direct tissue transplantation (e.g., corneal transplants) or hormonal extracts (e.g., human growth hormone before synthetic supplies were developed). Familial patterns have also been reported, which suggests that there may be genetic susceptibility to infection or vertical transmission of the disease agent. No antiviral agents have been shown to be effective in retarding or slowing disease progress, although amantadine (Symmetrel) has been reported occasionally to have had some success. Death usually ensues within 6 months to 2 years of onset.
10.4. The core features of dementia with Lewy bodies include
A. disturbance of consciousness
B. recurrent detailed visual hallucinations
C. cognitive decline caused by cerebrovascular disease
D. progressive language dysfunction
E. gradual changes in personality
View Answer
10.4. The answer is B
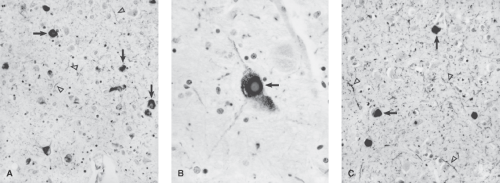
The core features of dementia with Lewy bodies include (1) fluctuating cognition with pronounced variations in attention and alertness; (2) recurrent visual hallucinations, which are typically well formed and detailed; and (3) spontaneous motor features of parkinsonism. At least one core feature must be present for clinical diagnosis, although the presence of two core features leads to a higher sensitivity. Dementia with Lewy bodies is a neurodegenerative dementia characterized by progressive cognitive decline of sufficient magnitude to interfere with normal social or occupational function. It is now considered to be the second most common cause of dementia after Alzheimer’s disease. Figure 10.3 shows cortical Lewy bodies. Table 10.1 lists the pathological features of dementia with Lewy bodies, and Table 10.2 includes recently developed consensus guidelines for clinical diagnosis.
The core symptoms of delirium include a disturbance of consciousness that is accompanied by a change in cognition that develops rapidly, usually over hours or days, and tends to fluctuate during the course of the day.
Vascular dementia refers to cognitive decline caused by ischemic, hemorrhagic, or oligemic injury to the brain as a consequence of cerebrovascular and cardiovascular disease. The diagnosis is made if dementia is associated with focal neurological signs and symptoms and neuroimaging evidence of cerebrovascular disease is present. Frontotemporal dementia is a progressive change in personality and behavior, with variable degrees of language and other cognitive impairment. There are two core clinical patterns: (1) gradual changes in personality and behavior and (2) progressive language dysfunction. The hallmark of the behavioral presentation is typically a combination of disinhibition, apathy, and limited insight.
Table 10.1 Pathological Features Associated with Dementia with Lewy Bodies | ||
|---|---|---|
|
10.5. Transient global amnesia
A. is more common in women
B. is more common in young people
C. is associated with loss of self-identity
D. has a characteristically abnormal EEG pattern
E. has been linked to vascular instability
View Answer
10.5. The answer is E
Transient global amnesia is a syndrome characterized by the sudden onset of a profound anterograde amnesia and retrograde amnesia for the past weeks or months. There is an association with migraine in about 15 percent of cases, leading to etiologic speculation of vascular instability. It occurs in men more than women, and typically after age 50 years. The patient is generally able to recall his or her own identity and that of relatives or close associates but is not able to retain his or her immediate context even when explained to the patient repeatedly. There is no disturbance of consciousness and no detectable seizure activity on electroencephalogram obtained during the event.
Table 10.2 Consensus Criteria for the Clinical Diagnosis of Probable and Possible Dementia with Lewy Bodies | ||
|---|---|---|
|
10.6. Which of the following is a true statement about Parkinson’s disease?
A. It is the result of the degeneration of the substantia nigra, globus pallidus, putamen, and caudate.
B. It cannot be distinguished from parkinsonian syndromes that arise from a variety of causes.
C. Dementia is more common in early-onset disease.
D. It is a prototype of a cortical degenerative disease.
E. The only cells affected are those containing dopamine.
View Answer
10.6. The answer is A
Described by James Parkinson in 1817, Parkinson’s disease is a prototype of a subcortical, not cortical, degenerative disease. It is idiopathic and must be distinguished from parkinsonian syndromes that arise from a variety of causes.
Parkinson’s disease is the result of the degeneration of subcortical structures, primarily the substantia nigra but also the globus pallidus, putamen, and caudate. Cells containing dopamine are predominantly affected, although serotonergic and other systems are disrupted as well. Medication-induced parkinsonism presumably involves only a dysfunction of the basal ganglia structures without any obvious pathoanatomical abnormality. The typical age at the onset of Parkinson’s disease is between 50 and 60 years but may vary widely with the onset sometimes occurring 1 to 2 decades earlier. The clinical course is chronic and progressive with severe disability attained after approximately 10 years. A smaller proportion of patients have a more rapidly progressive disease, and a yet smaller group has a slowly progressive disorder in which deterioration plateaus or remains minimal for 2 to 3 decades.
In general, subcortical diseases are thought to impinge on the three Ms—movement, mentation, and mood. In Parkinson’s disease, all three of these areas are affected, although not always uniformly. The movement abnormalities are characterized by the triad of tremor, rigidity, and bradykinesia. The tremor and rigidity may be unilateral or bilateral. Bradykinesia is manifested by slowness in the initiation and execution of movement. The typical presentation, with a masklike facies, minimal blink, and monotonic speech, is a concomitant of the rigidity and slowness of movement. Other prominent characteristics include postural changes such as chin-to-chest flexion and gait abnormalities. The gait is characteristically slow and shuffling, and the patient has difficulty turning (en bloc turning) and trouble initiating and stopping walking. Seborrhea, sialorrhea, excessive fatigue, and constipation are also common.
Mentation or cognition in Parkinson’s disease is an area of controversy. Most patients complain of slowed thinking, sometimes called bradyphrenia. In general, approximately 20 to 30 percent of patients with Parkinson’s disease are found to have dementia, with the likelihood greater in those with late-onset disease (after age 70 years). Neuropathologically, cases intermediate between Parkinson’s disease and Alzheimer’s disease exist, with Lewy bodies in the substantia nigra suggesting the former. There is no clear line of division as yet between a process resembling dementia of the Alzheimer’s type on which abnormal parkinsonian movements are superimposed and a clinical presentation of Parkinson’s disease in which the patient slowly develops a global progressive dementia.
10.7. Clinical characteristics of vascular dementia
A. are the same regardless of the area of infarction
B. are the same regardless of the number of infarctions
C. are the same regardless of the type of vasculature involved
D. are the same regardless of whether or not deficits accumulate or resolve quickly after small strokes
E. none of the above
View Answer
10.7. The answer is E (none)
The clinical characteristics of a vascular dementia depend on the area of infarction. As such, there is a wide variability in the possible presenting features of a vascular dementia. Single infarctions may result in the discrete loss of one particular function (e.g., language) without dementia per se. However, some strategically located infarctions can affect more than one domain of cognitive function and mimic the clinical picture of a global dementia. An example is the angular gyrus syndrome that can occur with large posterior lesions in the dominant hemisphere. It has been characterized as manifesting with alexia with agraphia, aphasia, constructional disturbances, and Gerstmann syndrome (acalculia, agraphia, right-left disorientation, and finger agnosia). Although the findings are similar to those of dementia of the Alzheimer’s type, angular gyrus syndrome can be distinguished by its abrupt onset; the presence of focal neurological, electroencephalographic, and imaging abnormalities; and preservation of memory and ideomotor praxis.
Vascular dementia is more commonly associated with multiple infarctions. The infarctions may take the form of numerous large infarctions accompanied by widespread cognitive and motor deficits. Tiny, deep infarctions—lacunae—result from disease of the small arteries that usually involves subcortical structures, such as the basal ganglia, thalamus, and internal capsule. Lacunar strokes are frequently associated with hypertension. The neurological and cognitive deficits may resolve quickly after each of the small strokes; however, the deficits may accumulate, leading to a persisting functional and intellectual decline. In the past, a stepwise pattern of deterioration was described for that type of vascular dementia, but it was dropped from the text revision of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) criteria because no specific pattern of deterioration has been reliably demonstrated for vascular dementias. Similarly, the description of patchy deficits has been deleted in light of the marked variability in presentation of vascular dementia, depending on the type of vasculature and the site and extent of infarction.
10.8. Huntington’s disease
A. is linked to the long arm of chromosome 4
B. is associated with “boxcar” ventricles on brain scanning
C. is not usually associated with emotional symptoms
D. shows striatal hypermetabolism on positron emission tomography (PET)
E. affects men only
View Answer
10.8. The answer is B
In Huntington’s disease, computed tomography and magnetic resonance imaging scans show caudate atrophy and characteristic “boxcar” ventricles. Functional imaging, such as positron emission tomography (PET), may show striatal hypometabolism. It is transmitted by a single autosomal dominant gene found on the short arm of chromosome 4. It is usually diagnosed in the late 30s or early 40s and affects men and women equally. Emotional symptoms often appear early and include irritability, depression, or psychosis.
10.9. The criteria for mild cognitive impairment includes all of the following except
A. memory complaints
B. objective memory impairment
C. preserved general cognitive function
D. intact daily living activities
E. dementia
View Answer
10.9. The answer is E
The criteria proposed by the Mayo Clinic Alzheimer’s Disease Research Center (MCADRC) for mild cognitive impairment are (1) memory complaint, preferably qualified by an informant; (2) objective memory impairment for age and education; (3) preserved general cognitive function; (4) intact activities of daily living; and (5) not demented.
10.10. Which of the following is a prion disease?
A. Creutzfeldt-Jakob disease
B. Variant Creutzfeldt-Jakob disease
C. Kuru
D. Fatal familial insomnia
E. All of the above
View Answer
10.10. The answer is E (all)
Prion disease is a group of related disorders caused by a transmissible infectious protein known as a prion. Included in this group are Creutzfeldt-Jakob disease (CJD), Gerstmann-Straussler syndrome (GSS), fatal familial insomnia (FFI), and kuru. A variant of CJD (vCJD), also called “mad cow disease,” appeared in 1995 in the United Kingdom and is attributed to the transmission of bovine spongiform encephalopathy (BSE) from cattle to humans.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree