Delta Activity
▲ Polymorphic Delta Activity
Other Names
Slow activity
Abnormal slowing
Arrhythmic delta activity
Anterior bradyrhythmia
Broad sharp waves
Types
Zeta waves
Description
Delta activity currently is defined as any rhythmic activity with a frequency less than 4 Hz, individual waves with durations greater than 250 millisecond, and any combination of individual waves that each has a duration longer than 250 millisecond. This differs from the original definition of delta activity, introduced by Grey Walter in 1936, that defined delta activity as all activity below the alpha frequency range (Niedermeyer, 1999c). Walter later modified the definition with the insertion of the theta range between alpha and delta activities, which lowered the upper frequency limit for the delta range. Polymorphic delta activity (PDA) arises from the combination of individual delta waves of differing durations, and this results in arrhythmic activity because of the differences among the waves. PDA is a common finding on EEGs, and PDA may be either normal or abnormal, depending on its features and circumstances. Abnormal PDA commonly and characteristically has consistent asymmetric frequency, distribution, amplitude, or superimposed faster frequencies. It also may lack an increase in frequency with alerting stimulation from touch or noise. Normal PDA is symmetric in all of these features and usually demonstrates a frequency increase with alerting, but abnormal PDA also may have several of these normal features and even have only one of the features indicating abnormality. Focal PDA is a clear abnormality and typically has a minimal amount of superimposed faster frequencies. It indicates a focal lesion in the white matter that is deep to the EEG region with maximal PDA (Blume et al., 2002). Anterior bradyrhythmia indicates bilateral frontal PDA.
Normal PDA is a characteristic finding of nonrapid eye movement (NREM) sleep. With progression of sleep into its deeper sleep stages, the PDA has decreasing frequency and increasing presence in the recording. Slow-wave sleep (NREM stage 3) is defined as when 20% or more of each 30-second epoch consists of waves with frequencies between 0.5 and 2 Hz and amplitudes greater than 75 μV (Silber et al., 2007). The PDA of sleep disappears with alerting and is not present in a persisting presence in full wakefulness. However, some residual PDA may persist temporarily during awakening. Waves with delta duration may occur in full wakefulness as specific patterns, including posterior slow waves of youth (PSWY) and cone waves. These delta-wave patterns are discussed in other chapters.
Zeta waves are a type of delta wave with a distinctive, sharply diphasic waveform. Broad sharp wave is a term for what appears to also be zeta waves. The essential waveform is a “Z” turned counterclockwise onto its side. This produces an alternating saw-toothed shape that comprises a rise followed by an overshooting fall below the baseline and then a rise back to the baseline. This waveform varies somewhat between waves, even within a run of several individual zeta waves. When zeta waves occur in runs, the total duration is usually 1.5 to 3 seconds and includes two or three waves (Magnus and Van der Holst, 1987). Zeta-wave amplitude usually is greater than 100 μV and may reach 400 μV. Although zeta waves most commonly have a focal frontal field, they may occur over any region of the scalp and also may occur bisynchronously. As such, they may be bifrontal.
Distinguishing Features
• Compared to Intermittent Rhythmic Delta Activity
PDA and intermittent rhythmic delta activity (IRDA) may occur in similar clinical circumstances and may occur independently within the same EEG. However, they have clear distinguishing features with differences in rhythmicity, persistence, and distribution. As the name indicates, PDA is not regular and does not occur
with the rhythm characteristic of IRDA. Furthermore, IRDA’s rhythms are intermittent, brief, monomorphic bursts that stand apart from the background, which usually comprises faster frequencies and appears less abnormal. This differs from PDA, which is persistent as ongoing background activity with varying frequency and waveform. Bilateral PDA also is more likely to be generalized with extension across the coronal midline; however, generalized IRDA also occurs.
with the rhythm characteristic of IRDA. Furthermore, IRDA’s rhythms are intermittent, brief, monomorphic bursts that stand apart from the background, which usually comprises faster frequencies and appears less abnormal. This differs from PDA, which is persistent as ongoing background activity with varying frequency and waveform. Bilateral PDA also is more likely to be generalized with extension across the coronal midline; however, generalized IRDA also occurs.
• Compared to Polymorphic Theta Activity
Irregular slowing may occur across a spectrum of frequencies and include both the theta and delta frequency ranges. The division between these two ranges is arbitrary but useful for quickly describing an EEG’s general appearance. Nevertheless, the duration of the individual waves is the essential distinguishing feature, with waves of longer than 250 millisecond indicating delta activity.
Co-occurring Patterns
The normal PDA of NREM sleep is accompanied by other EEG signs of NREM sleep, including vertex sharp transients, sleep spindles, K complexes, and positive occipital sharp transients of sleep (POSTS); however, these other patterns occur more often in NREM stages 1 and 2 than in 3. Indeed, NREM stage 3 may include only PDA and have no electrographic features that would distinguish it as normal sleep and not severe encephalopathy. Conversely, encephalopathy may be distinguished through the occurrence of abnormalities, such as epileptiform discharges, focal slowing, superimposed focal or generalized fast activity, and attenuations or electrodecrements.
Clinical Significance
Generalized PDA indicates either encephalopathy or sleep, and encephalopathy in this context is a nonspecific state of broad cerebral dysfunction with associated diffuse cognitive impairment. PDA is so intrinsic to NREM sleep that the amount of PDA is the defining factor for distinguishing stage 2 from stage 3, and it also leads to the term slow wave sleep, which is a synonym for stage 3.
An encephalopathy with accompanying generalized PDA may be reversible or irreversible. Reversible states are due to transient physiologic abnormality or due to endogenous or exogenous sedatives. Physiologic abnormalities with potential to produce PDA include migraine, syncope, ischemia, hypothermia, and recovery from an epileptic seizure (Ammirati et al., 1998; Ganji et al., 1993; Ramelli et al., 1998; Visser et al., 1999). Metabolic dysfunction is the principal source for endogenous sedation and may be produced by endocrine, liver, and kidney diseases. Exogenous sedatives are specific toxins and pharmaceuticals, such as narcotics and anesthetics (Sebel et al., 1981). Generalized PDA also may be irreversible as from a diffuse cerebral insult such as anoxia, infection, hypoglycemia, and inflammation; developmental abnormality usually with global cognitive impairment; or some of the degenerative or dementing illnesses such as advanced forms of cerebrovascular disease, Alzheimer disease, and sometimes schizophrenia (Gibbs and Gibbs, 1941; Inui et al., 2001; Matsuura et al., 1994; Naidu and Niedermeyer, 1999; Niedermeyer, 1999a; Schauble et al., 2003; Thumasupapong et al., 1995). PDA occurs when serum glucose is less than 35 mg/100 mL, and all other frequencies are absent when the glucose drops to 18 mg/100 mL (Gibbs and Gibbs, 1941). Serum glucose concentrations that are even lower will produce generalized attenuation. Inflammatory causes of PDA include encephalitis, purulent meningitis, and some autoimmune diseases such as Sydenham’s disease and Behcet’s disease (Westmoreland, 1999).
Regardless of its cause, generalized PDA is similar to focal PDA as a sign of cerebral white matter abnormality (Sharbrough, 1999; Zifkin, 1990). This abnormality must be significant and include either cellular toxicity or mechanical compression. Interstitial edema alone is unlikely to be capable to produce abnormal slowing (Whittle et al., 1992). Often, the white matter pathology is accompanied by cerebral cortical abnormality, but abnormality limited to the cerebral cortex does not produce slowing. Instead, purely cortical abnormality produces attenuation and loss of the faster frequencies (Schaul, 1990). PDA with a more paroxysmal pattern typically is more deeply situated (Bauer, 1999). With clinical worsening, frontal IRDA (FIRDA) and occipital IRDA (OIRDA) may progress to PDA (Sharbrough, 1999).
Compared to generalized PDA, focal PDA typically is more persistent, more polymorphic, and less reactive to stimulation or the behavioral state (Sharbrough, 1999). Furthermore, it is more clinically specific by usually indicating a similarly localized structural or functional abnormality (Huppertz et al., 2001). However, it also may occur with diffuse abnormalities or from a lesion at a distant site in the posterior fossa (Martinius et al., 1968; Maytal et al., 1993). Regardless of location, structural abnormalities usually have more continuous PDA. Among such lesions, abscesses typically have a larger field and higher amplitude than similarly sized tumors (Fischer-Williams and Dike, 1999). Transient and fluctuating focal PDA may indicate migraine, mild trauma, recovery from a focal seizure, and a cerebral ischemia or a transient ischemic attack (Fisch, 1999).
Zeta waves most commonly occur in the context of acute cerebral lesions. They usually disappear with recovery but may persist for years. In a series of 33 patients, 87% of EEGs demonstrating zeta waves had a structural lesion on neuroimaging, and the positive predictive value of zeta waves for a lesion was found to be 96% (Dunne and Silbert, 1991). Moreover, zeta waves are more likely to occur from a tumor, hematoma, or focal trauma than from infarction (Westmoreland and Klass, 1990). They also have a high association with seizures and have been proposed to be an interictal epileptiform abnormality. In a series of 48 patients, 47 had seizures, which equates to a positive predictive value of 98% (Bauer et al., 2008).
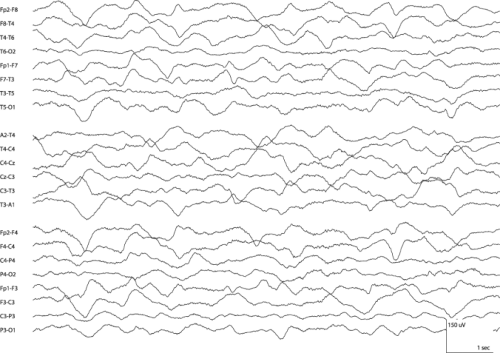
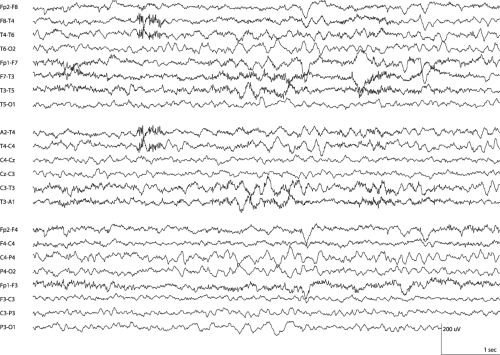
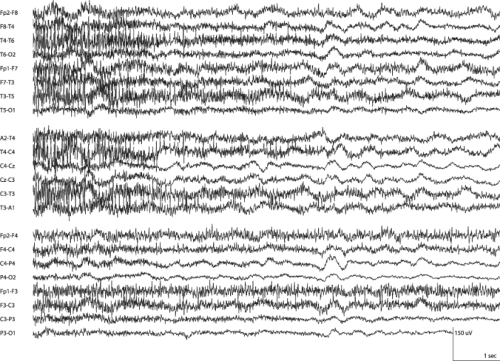 Figure 10-3 Polymorphic Delta Activity • The EEG segment originated from the same recording as Figure 10-2 and is set to the same gain, but preceded administration of a paralytic medication. Diffuse muscle artifact obscures the generalized slowing to varying extents and prevents accurate interpretation of some portions of the EEG. The patient required intubation and ventilation, so temporary paralysis was a reasonable means to improve the EEG’s sensitivity for seizures. (LFF 1 Hz, HFF 70 Hz) |
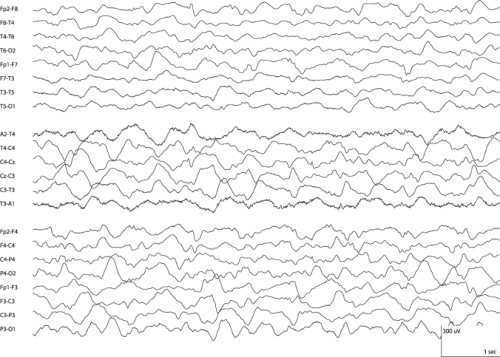
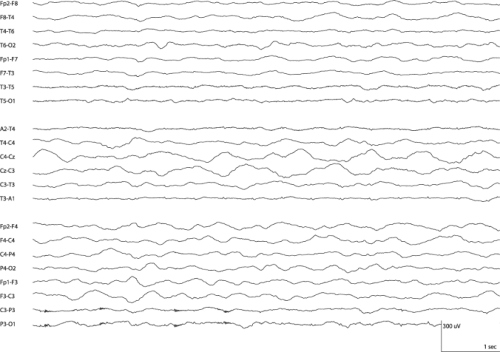 Figure 10-5 Polymorphic Delta Activity • This segment was recorded from the patient whose EEG is Figure 10-4. Compared to Figure 10-4, which was recorded 10 days earlier, this segment has greater generalized slowing, lower amplitude, and a decrease in superimposed faster frequencies. The two figures have the same gain setting. Medical and neurologic deterioration had occurred. (LFF 1 Hz, HFF 70 Hz) |