Demyelinating Disease
A. Multiple sclerosis
Multiple CNS demyelinating attacks, disseminated in time and space.
1. Definitions:
a. Attack (exacerbation, relapse): Inflammatory and demyelinating lesion lasting >24 h, objective clinical findings, separated by 30 d between onset of attacks.
b. Course: Relapsing-remitting, secondary progressive, primary progressive.
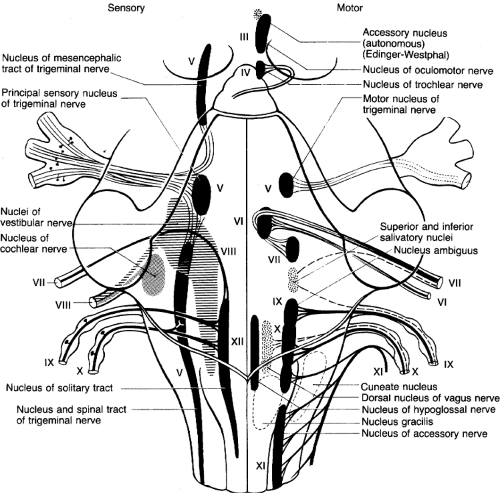
Figure 6. Cranial nerve nuclei. (Reprinted with permission from Duus P. Topical Diagnosis in Neurology. New York: Thieme; 1983:105.)
c. MRI Criteria: Three of the following: at least one gad+ lesion or nine T2 lesions, one infratentorial lesion, one juxtacortical lesion, at least three periventricular lesions. Spinal cord lesions considered equivalent to infratentorial lesion, enhancing brain lesion, and T2 lesion.
d. % criteria: Diagnostic criteria for “MS,” “possible MS,” and “not MS.”
2. H&P:
a. Common presenting sx: Optic neuritis, weakness and numbness, diplopia, vertigo, myelitis, urinary retention. Sx worse with heat (Uthoff’s phenomenon).
b. Other MS sx: Urinary retention, pain, fatigue, Lhermitte’s phenomenon (tingling on neck flexion), internuclear ophthalmoplegia, cognitive changes. Weakness frequently worst in hands and hips.
c. MS flare: Usually subacute (>1 wk) deterioration. Acute (1-3 d) deterioration suggests an infection that is briefly exacerbating MS sx. Does the pt. use catheters?
Table 6. McDonald criteria for diagnosis of MS.
MCDONALD CRITERIA FOR DIAGNOSIS OF MS
Clinical Presentation
Additional Data Needed for DX
≥2 attacks, and ≥2 lesions with
objective clinical evidence
None
≥2 attacks and 1 lesion with
objective clinical evidence
Dissemination in space, by MRI or ≥2
MRI lesions plus + CSF or 2nd clinical
attack at different site
1 attack, and ≥2 lesions with
objective clinical evidence
Dissemination in time, by MRI or 2nd
clinical attack
1 attack, and 1 lesion with objective
clinical evidence (clinically
isolated syndrome)
Dissemination in space, by MRI or ≥2
MRI lesions plus + CSF and
dissemination in time (disseminated by
MRI or second clinical attack)
Insidious neurological
progression suggestive of MS
One year of progression and 2 of the
following 3: (A) + Brain MRI (9 T2
lesions or 4+T2 lesions with +VEP);
(B) + spinal cord MRI (2 T2 lesions);
(C) + CSF
3. Tests:
a. Initial workup:
1) MRI brain + contrast: see p. 188. Pts. with a first MS-like neurological event and significant white matter lesions on MRI have a 5-year incidence of MS of about 80%. If no lesions, risk is about 5%.
2) MRI spinal cord + contrast only if clinically suspicious.
3) If unusual clinical picture or criteria not fulfilled: CSF for elevated IgG index or oligoclonal bands (WBC should be <50) and VEP (delayed but preserved wave form).
4) Consider Lyme titer, RPR, B12 level, HIV, ESR, ANA, ACE, HTLV.
b. MS attack: CBC, urinalysis, CXR and ESR to help r/o infection that could mimic an attack; consider tests to r/o disc herniation or entrapment neuropathy.
4. DDx:





