Developmental Anomalies
 Arachnoid Cysts
Arachnoid Cysts
1. Characterize intracranial arachnoid cysts. |
| G7 p.222:100mm |
a. Origin: c_____ | congenital |
|
b. C_____ _____ _____ produce _____. | cells of lining; CSF |
|
c. age: y_____ _____ | young patients |
|
d. incidence per 1000 autopsies_____ | 5 |
|
e. symptoms of s_____, h_____ | seizures, headache |
|
f. treatment: s_____, d_____, f_____ | shunt, drain, fenestrate |
|
g. path: s_____ a_____ m_____ | split arachnoid membrane |
|
2. True or False. Acute deterioration in patients with known arachnoid cysts usually signifies |
| G7 p.223:65mm |
a. rapid increase in cyst size | false |
|
b. postictal state | false |
|
c. rupture into subdural space | false |
|
d. rupture of bridging veins and cyst bleed | true |
|
3. Complete the following about arachnoid cysts: |
| G7 p.222:177mm |
a. The location of the only extradural type of arachnoid cyst is in the_____ cyst. | intra sellar |
|
b. A retrocerebellar arachnoid cyst might mimic a_____ _____syndrome. | Dandy-Walker |
|
c. The most common location for an arachnoid cyst is the_____ _____. | sylvian fissure |
|
d. The next most common location is the _____ _____. | cerebellopontine angle |
|
e. They are associated with ventriculo megaly in _____%. | 64% | G7 p.224:45mm |
f. The best treatment is probably_____ of_____. | shunting of cyst | |
4. Complete the following regarding intraspinal cysts: |
| G7 p.224:70mm |
a. If you find one ventrally think_____ _____. | neurenteric cyst |
|
b. If you find one dorsally think_____ _____. | arachnoid cyst |
|
 Intracranial Lipomas
Intracranial Lipomas
5. Intracranial lipomas |
| G7 p.225:130mm |
a. are usually found in the_____ _____ | midsagittal plane |
|
b. especially in the_____ _____. | corpus callosum |
|
c. They are frequently associated with _____ | agenesis |
|
d. of the_____. | corpus callosum |
|
e. They may less frequently involve the |
| |
i. _____ _____ | tuber cinereum |
|
ii. and the_____ _____. | quadrigeminal plate |
|
6. True or False. Characteristics of intracranial lipomas include |
| G7 p.225:145mm |
a. Association with_____abnormalities | congenital |
|
b. On CT they have a _____density. | low |
|
c. Differential diagnosis is |
|
|
i. d_____ c_____ | dermoid cyst |
|
ii. t_____ | teratoma |
|
iii. g_____ | geminoma |
|
d. On MRI they have a _____intensity on T1 | high (like fat) |
|
e. On MRI they have a _____intensity on T2. | low |
|
7. Intracranial lipomas may present clinically with |
| G7 p.225:178mm |
a. s_____ | seizures |
|
b. h_____ d_____ | hypothalamic dysfunction |
|
c. h_____ | hydrocephalus |
|
d. m_____ r_____ | mental retardation |
|
 Hypothalamic Hamartomas
Hypothalamic Hamartomas
8. Hypothalamic hamartomas |
| G7 p.226:50mm |
a. are frequent or rare? | rare |
|
b. are neoplastic or nonneoplastic? | nonneoplastic |
|
c. consist of a mass of_____ _____ | neuronal tissue |
|
d. that arises from the |
|
|
i. in_____ h_____ or | inferior hypothalamus |
|
ii. t_____ c_____ | tuber cinereum |
|
9. Hypothalamic hamartomas clinically |
| G7 p.226:98mm |
a. may present with a special type of seizure called _____, which means _____ seizure | gelastic; laughing | |
b. may also have_____ attacks | rage |
|
c. |
| G7 p.226:125mm |
i. may also present with p_____ p_____ | precocious puberty |
|
ii. due to release of g_____ r_____ h_____ | gonadotropin releasing hormone |
|
iii. formed within the_____ cells | hamartoma |
|
 Neurenteric Cysts
Neurenteric Cysts
10. Complete the following about neurenteric cysts: |
| G7 p.227:100mm |
a. A neurenteric cyst is a central nervous system (CNS) cyst lined with_____ | endothelium |
|
b. resembling the_____ or_____ tract. | gastrointestinal or respiratory |
|
c. Regions affected are usually the_____ or_____ areas. | cervical or thoracic | G7 p.227:115mm |
d. Histology is a cyst lined with c_____- c_____ e_____ | cuboidal-columnar epithelium |
|
e. with m _____-s_____ g_____ c_____. | mucin-secreting goblet cells | G7 p.228:34mm |
 Craniofacial Development
Craniofacial Development
11. Complete the following about craniofacial development: |
| G7 p.228:105mm |
a. The anterior fontanelle closes by age _____. | 2.5 years |
|
b. Head size is 90% of adult size at age _____ | 1 year |
|
c. The head stops enlarging by age _____ | 7 years | G7 p.228:130mm |
d. The skull is_____ at birth. | unilaminar |
|
e. Diploë appears by the _____year and | fourth |
|
f. reaches a maximum at age_____ | 35 years |
|
g. Diploic veins form at age_____. | 35 years |
|
h. Air cells in the mastoid occur in _____ year. | sixth |
|
12. True or false. Craniosynostosis |
| G7 p.228:172mm |
a. has been proven to occur after shunting. | false |
|
b. of one suture does not cause ↑ ICP. | false—11 % have ↑ ICP |
|
13. Complete the following about craniofacial development: |
| G7 p.229:157mm |
a. The most common craniosynostosis is _____. | sagittal |
|
b. The male to female ratio is | 80:20 |
|
c. The resulting skull shape is | dolichocephalic/scaphocephalic/boat shape | |
d. Surgery should be done within the age range of_____. | 3 to 6 months |
|
e. The strip craniectomy should be_____ cm wide. | 3 |
|
14. Complete the following regarding coronal synostosis: |
| G7 p.230:28mm |
a. Incidence of patients with craniosynostosis who have coronal synostosis is _____%. | 18% |
|
b. In which is it more common, males or females? | females |
|
15. Coronal suture synostosis (CSS) |
| G7 p.230:35 mm |
a. plus syndactyly is called_____ syndrome. | Apert |
|
b. Unilateral CSS is called_____. | plagiocephaly |
|
c. CSS plus hypoplasia of the face is called_____ disease. | Crouzon |
|
d. Plagiocephaly has an unusual orbit appearance on x-ray called the_____ _____ _____. | harlequin eye sign |
|
e. Plagiocephaly |
|
|
i. Forehead on affected side is _____ or _____ | flattened or concave |
|
ii. Supraorbital ridge has a _____margin. | higher |
|
16. Harlequin eye sign |
| G7 p.230:40mm |
a. occurs in u_____ c_____ suture closure | unilateral coronal |
|
b. seen on_____ _____ _____. | anteroposterior skull x-ray |
|
c. The abnormal bony structure is the_____ _____ | supraorbital margin |
|
d. and is_____ than on the normal side. | higher |
|
17. Complete the following about craniofacial development: |
| G7 p.230:80mm |
a. What suture is closed to produce trigonocephaly? | metopic |
|
b. It is usually associated with an abnormality of the_____ chromosome. | 19p |
|
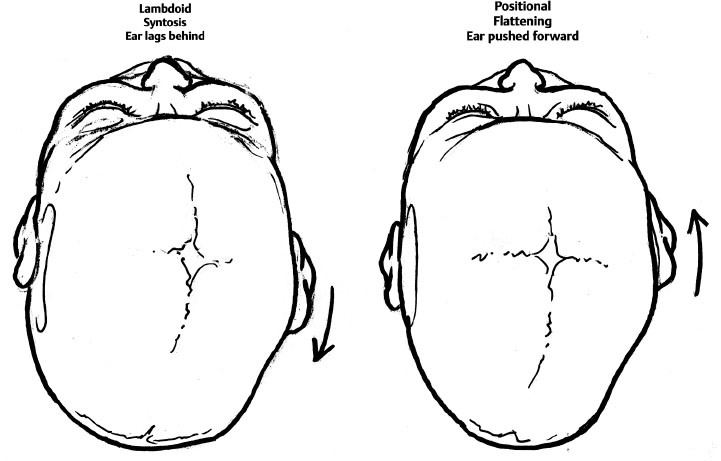
18. Characterize lambdoid synostosis. |
| G7 p.230:100mm |
a. Male to female ratio is_____. | 4:1 |
|
b. Side involved most frequently is_____. | right side |
|
c. The frequency of involvement is_____% right. | 70% |
|
d. Does it have a ridge or an indentation to palpation? | not a ridge like the sagittal or coronal synostosis, but it has an indentation | |
19. Considering lambdoid synostosis: |
| G7 p.230:160mm |
| ||
Fig. 8.1 |
| illustration by Tony Pazos |
a. Differentiate from positional flattening by looking at the ears from the_____ _____ _____ _____. | top of the head |
|
b. In lambdoid synostosis you will see the ipsilateral ear_____ _____. | lags behind |
|
c. In positional flattening you will see the ipsilateral ear is _____ _____. | pushed forward (If flat side of occipital bone is same side as the posteriorly positioned ear it is a case of lambdoid synostosis; if not it is a case of positional flattening.) |
|
20. Answer the following concerning lambdoid synostosis treatment: |
| G7 p.231:85mm |
a. True or False. All require surgery. | false (Only 15% won’t respond to repositioning.) |
|
b. True or False. Surgery is indicated early (i.e., in 3 to 6 months). | false (One can observe for 3 to 6 months for improvement.) |
|
c. Ideal age for surgery is_____ to_____ months. | 6 to 18 |
|
d. Early surgery is indicated for s_____ d_____ and e_____ i_____ p_____. | severe disfigurement and elevated intracranial pressure | |
21. Describe oxycephaly. |
| G7 p.231:155mm |
a. Definition:_____ _____ | tower skull |
|
b. Occurs if there is fusion of_____ _____ | multiple sutures |
|
c. Is there elevated ICP? | yes |
|
d. What is the status of the sinuses? | underdeveloped sinuses |
|
22. Complete the following about craniofacial development: |
| G7 p.232:60mm |
a. Cranium bifidum is another name for _____ or_____. | encephalocele or meningocele |
|
b. What type does not produce a visible soft tissue mass? | basal encephalocele |
|
c. Definition: an extension of_____ structures outside the normal_____ of the skull | normal, confines | G7 p.232:75mm |
d. A nasal polypoid mass in a newborn should be considered an_____ until proven otherwise. | encephalocele | G7 p.232:75mm |
23. Complete the following about encephalocele: |
| G7 p.232:130mm |
a. Incidence of the basal form of encephalocele is _____%. | 1.5% |
|
b. May exit the skull via a defect in |
|
|
i. c_____ p_____ | cribriform plate |
|
ii. f_____ c_____ | foramen cecum |
|
iii. s_____ o_____ f_____ | superior orbital fissure |
|
c. Treatment is by a combined i_____ and t_____ approach | intracranial and transnasal |
|
 Chiari Malformation
Chiari Malformation
24. Compare Chiari types I and II. |
| G7 p.233:100mm |
a. medulla-caudal dislocation | Chiari I, no |
|
| Chiari II, yes |
|
b. into cervical canal | Chiari I, tonsils Chiari II, vermis, medulla, fourth ventricle |
|
c. myelomeningocele | Chiari I, no Chiari II, yes |
|
d. hydrocephalus | Chiari I, no Chiari II, yes |
|
e. medullary kink | Chiari I, no Chiari II, 55% |
|
f. cervical nerves | Chiari I, normal Chiari II, upward |
|
g. age at presentation | Chiari I, adult Chiari II, infant |
|
h. symptoms | Chiari I, neck pain Chiari II, hydrocephalus, respiratory distress | |
25. Complete the following about Chiari malformation: |
| G7 p.234:25mm |
a. Chiari I has how many abnormalities? | 1—with many names |
|
b. List four names this abnormality has been called. |
|
|
i. t_____ h_____ | tonsillar herniation |
|
ii. c_____ d_____ of c1 | caudal displacement of cerebellum |
|
iii. p_____ e_____ of t_____ | peglike elongation of tonsil |
|
iv. c_____ e_____ | cerebellar ectopia |
|
26. Chiari I |
| G7 p.234:25mm |
a. has how many deformities? | 1 |
|
b. is known by the following names |
|
|
i. e_____ | ectopia |
|
ii. e_____ | elongation |
|
iii. d_____ | displacement |
|
iv. h_____ | herniation |
|
c. symptoms |
|
|
i. o_____ h_____ | occipital headaches |
|
ii. c_____ p_____ | cervical pain |
|
27. What is the particular eye sign associated with Chiari I? | Downbeat nystagmus is considered a characteristic of this condition in 47%, but it can also occur in Chiari II. | G7 p.235:130mm |
28. What percentage of Chiari I patients have hydrosyringomyelia? | 20 to 30% of Chiari I patients have a syrinx. | G7 p.236:1 5mm |
29. Characterize the location of tonsils and Chiari I. | G7 p.236:1 5mm | |
a. Normal range related to foramen magnum | ||
i. high | 8 mm above |
|
ii. low | 5 mm below |
|
iii. mean | 1 mm above |
|
b. Chiari I range is |
|
|
i. high | 3 mm below |
|
ii. low | 29 mm below |
|
iii. mean | 13 mm below |
|
c. Symptoms can occur with tonsils at _____ mm below. | 2 |
|
d. Usual level considered cutoff for diagnosis is_____ mm below. | 5 |
|
30. Possible better correlation with symptoms of tonsillar herniation is the degree of brain stem compression |
| G7 p.236:100mm |
a. at the_____ _____ | foramen magnum |
|
b. as seen on the_____ | axial |
|
c. T_____ W1 MRI. | 2 | |
31. The best results from surgery occur if treated within years of onset of symtoms. | 2 | G7 p.237:160mm |
32. Complete the following concerning Chiari I: |
| G7 p.237:182mm |
a. The most common postop complication is | ||
i. _____ _____ | respiratory depression |
|
ii. in _____%. | 15% |
|
b. Occurs within how many days of surgery? | 5 |
|
c. Occurs mostly at what time of day? | night |
|
d. Death can occur from s_____ a_____. | sleep apnea |
|
e. Other risks of surgery include |
| |
i. c_____ f_____ l_____ | cerebrospinal fluid leak |
|
ii. injury to_____ _____ | posterior inferior cerebellar artery (PICA) |
|
iii. h_____ of c_____ h_____ | herniation of cerebellar hemispheres |
|
33. Complete the following concerning Chiari I: |
| G7 p.238:30mm |
a. Operative results |
|
|
i. Main benefit may be to_____ progression | arrest |
|
ii. Best results in patients with syndrome_____ syndrome | cerebellar |
|
iii. which consists of |
| G7 p.238:55mm |
t_____ a_____ | truncal ataxia |
|
l_____ a_____ | limb ataxia |
|
n_____ | nystagmus |
|
d_____ | dysarthria |
|
b. Which responds better: pain or weakness? | pain | G7 p.238:55mm |
34.Factors that correlate with a worse outcome are |
| G7 p.238:63mm |
a. a_____ | atrophy |
|
b. s_____ | scoliosis |
|
c. symptoms that are lasting more than_____ _____ | 2 years |
|
35. Which Chiari malformation is associated with myelomeningocele? | Chiari II | |
36. Study Chart. Chiari II anatomical abnormalities: A to Z. | atlas assimilation beaking of tectum bony abnormalities cerebellar folia poorly myelinated cervical medullary junction compression craniolacunia corpus callosum agenesis degenerated lower CN nuclei enlarged massa intermedia falx hypoplasia fourth ventricle trapped fusion of cervical vertebrae gyri miniaturized hydrocephalus heterotopia hydromyelia Klippel-Feil deformity low attachment of tentorium massa intermedia enlarged medulla oblongata “z” bend microgyria nuclei of lower CN degenerated platybasia peg of cerebellar tonsils septum pellucidum absent syringomyelia tectum beaking (fusion) tentorium low attachment Z-shaped bend of medulla | G7 p.238:137mm |
37. Considering Chiari II, presenting symptoms are due to dysfunction of |
| G7 p.239:15mm |
a. b_____ s_____ | brain stem |
|
b. l_____ c_____ n_____ | lower cranial nerves |
|
38. Finding on presentation of Chiari II Hint: n2 chiari two |
| G7 p239:30mm |
a. n_____ | nystagmus—down beat |
|
b. n_____ _____ | nasal regurgitation |
|
c. c_____ | cyanosis |
|
d. h_____ | hoarseness |
|
e. i_____ _____ _____ | impaired ventilatory drive |
|
f. a_____ _____, _____ | apneic spells, aspiration |
|
g. r_____, _____ _____ | regurgitation, respiratory arrest |
|
h. i_____ _____ | inspiratory stridor |
|
i. t_____ _____ _____ _____ _____ | tenth nerve (vagus) vocal cord paralysis |
|
j. w_____ _____ | weak arm—weak cry |
|
k. o_____ | opisthotonus | |
39. Complete the following regarding Chiari II: |
| G7 p.240:68mm |
a. The most common cause of mortality is_____ _____. | respiratory arrest |
|
b. The mortality at 6 years follow-up is _____%. | 40% |
|
c. Range of mortality |
|
|
i. Infants in poor condition (i.e., cardiopulmonary arrest, vocal cord paralysis, and/or arm weakness mortality) is _____%. | 71% |
|
ii. There is gradual onset of symptoms in _____%. | 23% |
|
iii. The worst prognostic factor for response to surgery is b_____v_____ c_____ p_____. | bilateral vocal cord paralysis |
|
 Dandy-Walker Malformation
Dandy-Walker Malformation
40. Complete the following regarding Dandy-Walker malformation (DWM): |
| G7 p.240:138mm |
a. It is caused by a_____ of the f_____ of L_____ and M_____. | atresia of the foramina of Luschka and Magendie (old theory) |
|
b. Results in |
|
|
i. agenesis of_____ | vermis |
|
ii. large_____ _____ _____, which communicates with the | posterior fossa cyst |
|
iii. _____ _____, which becomes | fourth ventricle |
|
iv. _____. | enlarged |
|
41. To differentiate DWM from retrocerebellar arachnoid cyst observe for |
| G7 p.241:28mm |
a. v_____ a_____ | vermian agenesis |
|
b. cyst opens into f_____ v_____ | fourth ventricle |
|
c. enlarged p_____ f_____ | posterior fossa |
|
d. elevation of the t_____ H_____ | torcular Herophili |
|
42. What is Dandy-Walker pathogenesis? |
| G7 p.241:50mm |
a. D_____ | Dilation of fourth ventricle |
|
b. A_____ | Agenesis of vermis |
|
c. N_____ | Membrane of fourth ventricle |
|
d. D_____ | Dysembryo genesis |
|
e. Y_____ | Hydrocephalus |
|
43. DWM patients |
| G7 p.241:60mm |
a. |
|
|
i. Hydrocephalus is present in_____% | 70 to 90% |
|
ii. and _____% of hydrocephalus patients have DWS. | 2 to 4% | |
b. A common associated abnormality is |
| G7 p.241:92mm |
i. _____ of the_____ _____ in | agenesis of the corpus callosum |
|
ii. _____%. | 17% |
|
c. and c_____ a_____ | cardiac abnormalities |
|
d. If treatment is necessary, you must shunt the ventricle, the cyst, or both? | cyst |
|
e. If aqueductal stenosis you should shunt _____also. | ventricle |
|
f. But shunting the lateral ventricle alone |
| G7 p.241:122mm |
i. is _____ | contraindicated |
|
ii. because it might cause_____ _____. | upward herniation |
|
g. To avoid _____ herniation | upward | G7 p.241:125mm |
h. you must not shunt the _____ alone. | ventricle | G7 p.241:125mm |
44. What is the prognosis in DWM? |
| G7 p.241:152mm |
a. Seizures occur in _____%. | 15% |
|
b. Mortality occurs in _____to _____%. | 12 to 50% |
|
c. Normal IQ is _____%. | 50% |
|
 Aqueductal Stenosis
Aqueductal Stenosis
45. True or False. Aqueductal stenosis is seen only in children. | false (Adults can present with symptoms as well.) | G7 p.241:179mm |
46. What are the causes of aqueductal stenosis? Hint: aqectal |
| G7 p.242:20mm |
a. a_____ | astrocytoma of brain stem |
|
b. q_____ | quadrigeminal plate mass |
|
c. e_____ | inflammation, infection |
|
d. c_____ | congenital atresia |
|
e. t_____ | tumors |
|
f. a_____ | arachnoid cysts |
|
g. l_____ | lipoma |
|
47. Complete the following concerning aqueductal stenosis: |
| G7 p.242:45mm |
a. It is associated with congenital hydrocephalus in _____%. | 70% |
|
b. MRI may show absence of |
|
|
i. n_____ f_____ v_____ in the | normal flow void |
|
ii. a_____ of S_____. | aqueduct of Sylvius |
|
c. MRI with contrast should be used to rule out_____ | tumor |
|
d. Follow-up should be for at least _____ | 2 years |
|
e. in order to rule out_____. | tumor | |
48. True or False. A patient with aqueductal stenosis of adulthood may have the following symptoms: |
| G7 p.242:100mm |
a. headache | true |
|
b. visual disturbances | true |
|
c. decline of mental function | true |
|
d. gait disturbance | true |
|
e. papilledema (sign) | true |
|
f. ataxia | true |
|
g. urinary incontinence | true |
|
49. What are the treatment options for aqueductal stenosis? |
| G7 p.242:175mm |
a. ventriculoperitoneal_____ _____ | CSF shunting |
|
b. T_____ _____ _____ _____ | Torkildsen shunt in adults |
|
c. ETV = _____ _____ _____ | endoscopic third ventriculostomy |
|
 Neural Tube Defects
Neural Tube Defects
50. With neural tube defects there are classification systems. Give examples of |
| G7 p.243:45 mm |
a. neurulation defects |
|
|
i. a_____ | anencephaly |
|
ii. m_____ | myelomeningocele |
|
b. postneurulation defects |
|
|
i. m_____ | microcephaly |
|
ii. h_____ | hydranencephaly |
|
iii. h_____ | holoprosencephaly |
|
iv. l_____ | lissencephaly |
|
v. s_____ | schizencephaly |
|
c. spinal defects |
|
|
i. d_____ | diastematomyelia |
|
ii. s_____ | syringomyelia |
|
51. Complete the following about neural tube defects: |
| G7 p.243:45mm |
a. Failure to fuse the anterior neuropore results in_____. | anencephaly |
|
b. Failure to fuse the posterior neuropore results in_____. | myelomeningocele |
|
c. The definition of microcephaly is head circumference_____ _____ _____ below the mean. | 2 standard deviations |
|
d. In hydranencephaly the cortex is replaced by_____. | CSF |
|
e. Failure to cleave can result in_____. | holoprosencephaly | |
52. Complete the following about neural tube defects: |
| G7 p.243:45mm |
a. Give examples of neurulation defects. |
|
|
i. a_____ | anencephaly |
|
ii. c_____ | craniorachischisis |
|
iii. m_____ | myelomeningocele |
|
b. These defects are due to _____ of the neural tube | nonclosure |
|
53. Complete the following about neural tube defects: |
| G7 p.243:70mm |
a. Name five postneurulation defects. |
|
|
i. h_____ | hydranencephaly |
|
ii. l_____ | lissencephaly (most severe) |
|
iii. h_____ | holoprosencephaly |
|
iv. a_____ of_____ _____ | agenesis of corpus callosum |
|
v. d_____ | diastematomyelia |
|
b. Which is the most severe? | lissencephaly |
|
54. Complete the following regarding lissencephaly: |
| G7 p.243:120mm |
a. It is an example of an abnormality of neuronal_____. | migration |
|
b. It results in an abnormality of the _____ convolutions | cortical |
|
c. called_____. | agyria |
|
55. Name the key features of schizencephaly. |
| G7 p.243:155mm |
a._____ which communicates with _____ | cleft; ventricle |
|
b. lined with_____ _____ | gray matter |
|
c. Two types are |
|
|
i. o_____ l_____ | open lipped |
|
ii. c_____ l_____ | close lipped |
|
56. Complete the following about neural tube defects: |
| G7 p.243:160mm |
a. In schizencephaly, the cleft wall is lined with cortical_____ _____. | gray matter |
|
b. In porencephaly, a cystic lesion is lined with _____ or _____ tissue. | connective or glial |
|
57. Hydranencephaly |
| G7 p.244:49mm |
a. is a _____-neurolation defect. | post- |
|
b. Cranium is filled with_____. | CSF |
|
c. Is there a small or large head? | macrocrania |
|
d. Most common etiology is_____ _____ _____. | bilateral ICA infarcts |
|
58. Angiography |
| G7 p.244:137mm |
a. of anterior circulation shows_____ _____. | no flow |
|
b. of posterior circulation shows _____. | normal | |
59. Complete the following about neural tube defects: |
| G7 p.244:150mm |
a. What are the three types of holoprosencephaly? Please list in order of decreasing severity. |
|
|
i. a_____ | alobar (single ventricle) most severe |
|
ii. s_____ | semilobar |
|
iii. l_____ | lobar (least severe) |
|
b. They occur because of |
|
|
i. failure to_____ | cleave |
|
ii. of the_____ _____ | telencephalic vesicle |
|
60. List the risk factors for neural tube defects. |
| G7 p.245:120mm |
a. B_____ i_____ | B12 insufficiency |
|
b. c_____ | cocaine—maternal use |
|
c. D_____ | Depakene—use during pregnancy |
|
d. f_____ a_____ i_____ | folic acid insufficiency |
|
e. f_____ | fever in first trimester |
|
f. h_____e_____ | heat exposure—maternal hot tub, sauna |
|
g. o_____ | obesity before and during pregnancy |
|
h. v_____ a_____ | valproic acid use during pregnancy |
|
i. v_____ | vitamins—prenatal up folic acid and B12 |
|
61. What are the tests for prenatal detection of neural tube defects? |
| G7 p.245:160mm |
a. serum _____ _____ (If high at 15 to 20 weeks be suspicious for neural tube defects.) | alfa fetoprotein (If high at 15 to 20 weeks be suspicious for neural tube defects.) |
|
i. u_____, | ultrasonography |
|
ii. which can detect what % of spina bifida cases? | 90% |
|
b. a_____ | amniocentesis |
|
62. For prenatal detection of neural tube defects |
| G7 p.245:168mm |
a. test mother’s serum for_____ _____. | alpha fetoprotein |
|
b. Has a success rate for |
|
|
i. spina bifida open _____% and | 91% |
|
ii. anencephaly_____ %. | 100% may be missed |
|
iii. Closed spinal dysraphism_____ _____ _____. | may be missed |
|
c. An overestimate of gestational age will make us think that a high alpha fetoprotein level is _____. | normal |
|
d. Real-time imaging is by_____. | ultrasonography | |
e. Identifies _____% of s_____ b_____. | 90% of spinal bifida |
|
f. Obtaining fluid from the womb is called _____. | amniocentesis |
|
g. It carries a risk of fetal loss of _____%. | 6% |
|
63. Characterize agenesis of the corpus callosum. |
| G7 p.246:70mm |
a. On computed tomographic scan the typical appearance is as follows: |
|
|
i. Third ventricle is_____ | expanded |
|
ii. Lateral ventricles are_____. | separated |
|
iii. Atria and occipital horns are _____. | dilated |
|
b. Corpus callosum forms at age_____ _____ after conception and forms from_____ to_____. | 2 weeks; rostral to caudal |
|
64. Complete the following concerning the bundles of Probst: |
| G7 p.246:115mm |
a. They are aborted beginnings of the_____ _____ | corpus callosum |
|
b. bulging into the_____ _____. | lateral ventricles |
|
65. Complete the following regarding agenesis of the corpus callosum: |
| G7 p246:155mm |
a. Does it always have clinical significance? | no, it may be an incidental finding |
|
b. Underlying cause may be an abnormality of a_____. | chromosome |
|
66. List the features of spina bifida occulta. Hint: bifidaocculta |
| G7 p.247:145mm |
a. b_____ | bifida |
|
b. i_____ | incidental |
|
c. f_____ | foot deformity |
|
d. i_____ | innocuous |
|
e. d_____ | diastematomyelia |
|
f. a_____ | atrophy of leg |
|
g. o_____ | occurs in 20 to 30% of people |
|
h. c_____ | cutaneous stigmata |
|
i. c_____ | clinical importance often nil |
|
j. u_____ | urinary incontinence |
|
k. l_____ | lipoma, leg weakness |
|
l. t_____ | tethered cord |
|
m. a_____ | absent spinous process |
|
67. Complete the following regarding myelomeningocele: |
| G7 p.248:28mm |
a. The anterior neuropore closes at gestational age day_____. | 25 |
|
b. The posterior neuropore closes at gestational age day_____. | 28 | |
68. Complete the following concerning myelomeningocele (MM): |
| G7 p.248:40mm |
a. Incidence if no previous child has a MM equals_____ % or_____ per 1000. | 0.2%, 2 |
|
b. One previous MM child equals _____% or_____ per 1000. | 2%, 20 |
|
c. Two previous MM children equals _____ %or _____ per 1000. | 6%, 60 |
|
d. Associated hydrocephalus equals incidence of _____%. | 80% |
|
e. Associated Chiari II occurs in_____ children with MM. | most |
|
69. Answer the following about myelomeningocele: |
| G7 p.248:40mm |
a. What is the incidence of meningocele or myelomeningocele? | 1 to 2/1000 live births (0.2%) |
|
b. Does the risk increase in families with one affected child? | yes (The risk does increase to 2 to 3% in families with one previous myelomeningocele child.) |
|
c. Does the risk increase in families with two affected children? | yes (It further increases to 6 to 8% in families with two previous affected children.) |
|
70. True or False. All children born with myelomeningocele have an associated Chiari II malformation. | false (Not all, but most, have Chiari II.) | G7 p.248:72mm |
71. True or False. Closure of myelomeningocele may result in the need for CSF shunting. | true | G7 p.248:77mm |
72. Meningomyelocele patients develop allergy to_____. | latex | G7 p.248:80mm |
73. True or False or Uncertain. Intrauterine closure of mm defect reduces |
| G7 p.248:120mm |
a. Chiari II defect | true |
|
b. hydrocephalus | uncertain |
|
c. neurological dysfunction | false |
|
74. Complete the following concerning myelomeningocele: |
| G7 p.248:140mm |
a. If ruptured start_____ (n_____ and g_____). | antibiotics (nafcillin and and gentamicin) |
|
b. Perform surgery within_____ to_____ hours. | 24 to 36 hours |
|
c. Better functional outcome occurs if children have spontaneous _____ of _____ _____. | movement of lower extremities |
|
d. Do multiple anomalies occur in myelomeningocele? | yes (average 2 to 2.5 additional anomalies in myelomeningocele) | |
75. Complete the following about myelomeningocele and early closure: |
| G7 p.248:140mm |
a. True or False. Results in improvement of neurological functions. | false (Early closure does not result in improvement of neurological function.) |
|
b. True or False. Results in lower infection rate | true (It does result in a lower infection rate.) |
|
c. Myelomeningocele should be closed within 12, 24, or 36 hours? | 24 |
|
76. Considering late problems in myelomeningocele repair, possible late problems include |
| G7 p.250:145 mm |
a. brain _____ | hydrocephalus— malfunctioning shunt |
|
b. cervicomedullary junction_____ | Chiari II compressing medulla |
|
c. cord_____ | syrinx |
|
d. cauda_____ | tethered cord |
|
77. Characterize myelomeningocele outcome without treatment and with treatment. |
| G7 p.251:25mm |
a. survive infancy without treatment ____% with treatment ____% | 15 to 30%, 85% |
|
b. normal IQ without treatment ____% with treatment____% | 70%, 80% |
|
c. ambulatory without treatment ____% with treatment ____% | 50%, 40 to 85% |
|
d. continence without treatment _____ with treatment ____% | rare, 3 to 10% |
|
78. For each of the following what are the facts to know concerning lipomeningocele? |
| G7 p.251:90mm |
a. age for surgery | 2 months is appropriate for surgery |
|
b. band | thick fibrovascular band constricts |
|
c. conus | is split |
|
d. dura | is dehiscent |
|
e. epidural fat versus | lipoma is distinct from epidural fat |
|
f. placode | lipoma attached to neural placode |
|
g. neuro exam | is normal 50% |
|
h. sensory loss | most common neurological abnormality |
|
i. stigmata | cutaneous |
|
j. urologicexam | should be done preop |
|
79. True or False. Lipomyelomeningocele is associated with tethered cord. | true | |
80. Study Chart. | lipomeningocele steps in surgical treatment: untether the cord Xomed CUSA (Cavitron Ultrasonic Surgical Aspirator) recording from anal sphincter free up sides from attachment to dura reduce bulk of fat using CUSA in the midline tie dura open to sides place bovine pericardial graft as dural substitute | G7 p.251:90mm Courtesy of Dr. David Frim |
81. True or False. The most common location of a dermal sinus tract is the |
| G7 p.252:130mm |
a. occipital region | false |
|
b. cervical region | false |
|
c. thoracic region | false |
|
d. lumbosacral region | true |
|
82. What is the most likely cause of dermal sinus? |
| G7 p.252:115 mm |
a. Failure of the_____ ectoderm | cutaneous |
|
b. to_____ | separate |
|
c. from the_____ -ectoderm | neuro |
|
d. at the time of_____ | closure |
|
e. of the_____ _____. | neural groove |
|
83. Dermal sinus items to know include |
| G7 p.252:115mm |
a. Location most common is the_____ area | lumbosacral |
|
b. Results from _____ of_____ of _____ _____ | failure of separation of cutaneous ectoderm |
|
c. from_____ _____ | neural ectoderm |
|
d. appears as a_____ | dimple: |
|
i. hair? | with or without hairs |
|
ii. midline? | close to midline |
|
iii. skin stigmata? | yes |
|
e. First manifestation is_____ dysfunction | bladder |
|
f. Tract always courses_____ from lumbosacral area | cephalad |
|
84. True or False. An epidermoid cyst contains hair follicles and sweat glands. | false (An epidermoid cyst contains stratified squamous epithelium with keratin from desquamated epithelium. A dermoid cyst is lined with dermis and contains sebum and hair.) | |
85. What is a major difference between epidermoid cyst and dermoid cyst? |
| G7 p.251:145mm |
a. Epidermoid cyst is |
|
|
i. lined with s_____ s_____ e_____ | stratified squamous epithelium |
|
ii. and contains only_____. | keratin (from desquamated epithelium) |
|
b. Dermoid cyst is |
|
|
i. lined with_____ | dermis |
|
ii. and contains_____ _____ such as | skin appendages |
|
iii. hair follicles? | yes |
|
iv. sebaceous glands? | yes |
|
86. True or False. A dermal sinus tract is a potential pathway for intradural infection such as meningitis or abscess. | true | G7 p.251:155mm |
87. Radiologic evaluation of dermal sinus |
| G7 p.253:48mm |
a. If seen at births do_____ | ultrasound |
|
b. If first seen later do_____ | MRI |
|
88. Given the above, indicate whether the dermal sinus tract should be excised at the given locations. |
| G7 p.253:80mm |
a. lumbar | yes |
|
b. sacral | yes, though controversial |
|
c. coccygeal | no |
|
89. Complete the following concerning the cranial dermal sinus: |
| G7 p.253:140mm |
a. The track extends_____. | caudally |
|
b. If the dermal sinus tract enters the skull they do so_____ to the torcula. | caudal |
|
 Klippel-Feil Syndrome
Klippel-Feil Syndrome
90. True or False. Klippel-Feil syndrome results from failure of |
| G7 p.253:183mm |
a. primary neurulation | false |
|
b. secondary neurulation | false |
|
c. dysjunction | false |
|
d. segmentation | true (Klippel-Feil results from abnormal segmentation of the cervical somites between 3 and 8 weeks gestation.) |
|
91. Klippel-Feil syndrome |
| G7 p.253:183mm |
a. results from failure of_____ of _____ _____ at gestational age of _____. | segmentation of cervical somites; 3 to 8 weeks |
|
b. Clinical triad |
|
|
i. Hairline is_____. | low |
|
ii. Neck is_____. | short |
|
iii. Motion is_____. | limited | |
c. Limitation of range of motion of the neck occurs only if more than_____ segments are fused. | 3 |
|
d. True or False. Other congenital abnormalities may also be present. | true |
|
e. True or False. Klippel-Feil causes symptoms related to fused vertebrae. | false (No symptoms ever attributed to the fused vertebrae.) |
|
92. True or False. Anomalies seen in association with Klippel-Feil include |
| G7 p.254:45mm |
a. Sprengel deformity | true |
|
b. webbing of the neck | true |
|
c. basilar impression | true |
|
d. unilateral absence of the kidney | true |
|
93. Possible systemic congenital abnormalities include (be specific) |
| G7 p.254:63mm |
a. g_____ | enitourinary—absence of one kidney |
|
b. c_____ | cardiopulmonary |
|
 Tethered Cord Syndrome
Tethered Cord Syndrome
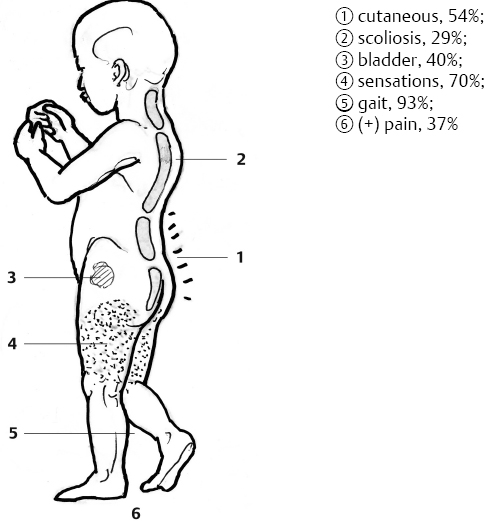
94. List six presenting signs and symptoms of tethered cord syndrome. |
| G7 p.254:130mm |
| ||
Fig. 8.2 | Illustration by Tony Pazos | |
95. True or False. In a patient with myelomeningocele with worsening scoliosis, spasticity, worsening gait, or deteriorating urodynamics, shunt evaluation is not part of the primary workup. | false (In a myelomeningocele patient with worsening clinical symptoms, shunt evaluation and confirmation of normal intracranial pressure should be one of the first modalities of intervention.) | G7 p.255:15mm |
96. True or False. |
| G7 p.255:33mm |
a. Progressive scoliosis is not seen in conjunction with tethered cord syndrome. | false (Progressive scoliosis may be seen in up to 29% of patients with tethered cord syndrome.) |
|
b. Early untethering may result in improvement in scoliosis | true |
|
97. True or False. The following is associated with adult tethered cord syndrome: |
| G7 p.255:78mm |
a. foot deformities | false (Foot deformities are associated with childhood tethered cord syndrome.) |
|
b. pain | true |
|
c. leg weakness | true |
|
d. urological symptoms | true |
|
98. True or False. Urological symptoms are not common in the adult tethered cord syndrome. | false (Urological symptoms are common in both pediatric and adult tethered cord syndrome.) | G7 p.255:95mm |
99. True or False. A tethered conus lies distal to L2 on radiographic evaluation. | true | G7 p.255:130mm |
100. Complete the following concerning tethered cord syndrome: |
| G7 p.255:132mm |
a. Name two criteria. |
|
|
i. conus below level_____ | L2 |
|
ii. thick filum greater than_____ | 2 mm diameter |
|
b. A preop test that is strongly recommended is a _____. | cystometrogram |
|
101. Indicate the characteristics used to identify the filum. |
| G7 p.255:180mm |
a. The vessel on the surface is _____. | squiggly |
|
b. The color of the filum is_____ _____ than nerve roots. | more white |
|
102. Complete the following outcome from tethered cord: |
| G7 p.256:30mm |
a. In meningomyelocele it is usually _____ to permanently untether. | impossible |
|
b. Repeated untethering is advised till patient stops_____. | growing | |
c. Symptoms of retethering are especially likely during the a_____ g_____ s_____. | adolescent growth spurt |
|
d. Surgical release in an adult is |
|
|
i. good for_____ and | pain |
|
ii. poor for_____ _____. | bladder function |
|
 Split Cord Malformation
Split Cord Malformation
103. True or False. Diastematomyelia is associated with a nonrigid bony septum that separates two durally ensheathed hemicords. | false (Diastematomyelia is associated with a rigid bony septum that separates two durally ensheathed hemicords.) | G7 p.256:84mm |
104. Complete the following concerning diastematomyelia: |
| G7 p.247:95mm |
a. cutaneous stigmata h_____ | tuft of hair hypertrichosis |
|
b. True or false. There are foot abnormalities | true |
|
c. specifically n_____ h_____- a_____ f_____. | neurogenic high-arched foot |
|
 Miscellaneous Developmental Anomalies
Miscellaneous Developmental Anomalies
105. True or False. In holoprosencephaly, there is absence of the septum pellucidum. | true | G7 p.247:33mm |
106. Characteristic features of septo-optic dysplasia include Hint: h3pvoplas3i2a |
| G7 p.247:55mm |
a. h_____ hypopituitarism |
| |
b. h_____ | hydrocephalus |
|
c. h_____ | hypersecretion of hormones |
|
d. p_____ | pituitary infundibulum absent |
|
e. v_____ | ventricles enlarged |
|
f. o_____ | optic nerves absent (blind) |
|
g. p_____ | panhypopituitarism |
|
h. l_____ | little-dwarfism-Tiny Tim |
|
i. a_____ | anterior midline structures fail |
|
j. s_____ | septum pellucidum absent |
|
k. s_____ | schizencephaly |
|
l. s_____ | sexual precocity |
|
m. i_____ | isolated growth hormone deficiency |
|
n. i_____ | intelligence normal |
|
o. a_____ | absence of midline morphogenesis | |
107. True or False. Septo-optic dysplasia frequently presents with symptoms of |
| G7 p.247:55mm |
a. panhypopituitarism | true |
|
b. sexual precocity | true |
|
c. dwarfism | true |
|
d. blindness | true |
|
e. impaired intelligence | false (Most patients are of normal intelligence.) |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree