Diagnosis and classification of schizophrenia
Symptoms
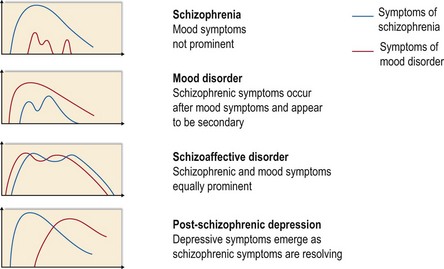
Symptoms required to make the diagnosis of schizophrenia are shown in Figure 1. It will be seen from this that some symptoms are virtually pathognomonic of schizophrenia. Most of these were described by Schneider and are known as Schneider’s first rank symptoms. If any of these symptoms are clearly present for at least one month and there is no organic cause, then the likely diagnosis is schizophrenia, although 15% will turn out to have an illness other than schizophrenia, most commonly a mood disorder. Two symptoms also considered to be diagnostic of schizophrenia were not described by Schneider: hallucinatory voices which appear to emanate from a body part and bizarre delusions.
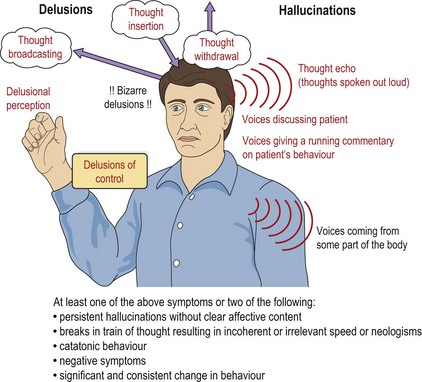
Fig. 1 Symptoms of schizophrenia. Schneider’s first rank symptoms are in red; other symptoms are in black.
Schizophrenia can also be diagnosed if at least two of the other symptoms shown in Figure 1 are present. There are also symptoms which are very common in schizophrenia but are not diagnostic because they occur relatively often in other conditions. The most common of these are persecutory delusions and delusions of reference, and examples of these are given in Table 1, along with examples of some of the symptoms described above.
Table 1 Examples of some common symptoms of schizophrenia
| Symptom | Example |
|---|---|
| Third person auditory hallucination | ‘I hear a voice saying “He’s an idiot, I hate him” and another saying “I don’t, he’s not that bad” ’ |
| Running commentary | ‘I hear a voice talking about what I’m doing, saying things like “Look at him, walking across the room. Now he’s making a cup of tea”.’ |
| Thought echo | ‘I hear my thoughts spoken out loud; it’s like a tape recorder playing them back to me out loud.’ |
| Thought insertion/withdrawal | ‘They put thoughts into my head and take them out.’ |
| Thought broadcasting | ‘The thoughts go out of my head. Other people can pick them up and tell what I’m thinking.’ |
| Delusions of control (passivity) | ‘They control my thoughts and make me feel sad. They must have some sort of machine to do it.’ ‘They create a force field that pushes me against the wall.’ |
| Delusional perception (delusional interpretation of a true perception) | ‘I knew the police were after me when I saw that the lamp-post outside wasn’t working.’ ‘When the postman opened the gate with his right hand, I knew the world would end tomorrow.’ |
| Bizarre delusions (delusions that could not possibly be true) | ‘I’m observed from an alien space-ship, they use a scanner in my radio and beam the signal up using microwaves.’ ‘My neighbour sends poisonous gas through the walls and down the telephone line.’ |
| Persecutory delusions | ‘My neighbour is spying on me for the government’ (also an example of a non-bizarre delusion, i.e. a false belief that could conceivably happen). |
| Delusions of reference (false belief that things refer to the patient) | ‘There are messages for me hidden in what they say on TV and the radio’ ‘When I see people talking, I know they are talking about me.’ |
| Thought disorder and neologisms | Patient says: ‘I walk down through back to square one something like the mooncar judging up to the nimjet”.’ |
Mood changes in schizophrenia
Changes in mood are a common feature of schizophrenia, and symptoms of schizophrenia can occur during episodes of mania or severe depression. As a result, there is often a difficult differential diagnosis between schizophrenia and mood disorders. Knowing when symptoms occurred and their relative severity is essential in making the correct diagnosis, as shown in Figure 2. Schizoaffective disorder, which is discussed in more detail on page 47, is diagnosed when first rank or other pathognomonic symptoms of schizophrenia occur at the same time as severe mood disturbance. Post-schizophrenic depression occurs as the acute psychotic phase is beginning to resolve. The depressive symptoms may seem to be an integral part of the illness or they may appear to be an understandable psychological reaction to having developed schizophrenia, but the diagnosis is the same in either case. It is an important condition to recognise, as it is associated with an increased risk of suicide.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree