Fig. 8.1
a Otoscopic exam: normal tympanic membrane b normal tympanic membrane with landmarks labeled. a. lateral process of malleus b. tympanic annulus c. chorda tympani d. incudostapedial joint e. handle of malleus f. shadow of Eustachian tube g. shadow of round window niche h. promontory (floor of middle ear) i. umbo j. bulge of anterior EAC wall k. hypotympanic air cells
Table 8.1
Findings on pneumatic otoscopy
Color | Position | Translucency | Mobility |
|---|---|---|---|
Gray | Normal | Translucent | Normal |
Yellow | Bulging | Semiopaque | Increased |
Amber | Retracted | Opaque (dull) | Decreased |
White | No movement | ||
Red | |||
Blue |
In contrast to a normal tympanic membrane, the exam findings in otitis media are quite different. OME (Fig. 8.2) will often present with complaints of fullness and possibly decreased hearing. It may also be asymptomatic. Exam findings in serous OME are usually a yellow or amber tympanic membrane with normal or retracted position. Mobility is usually impaired and air bubbles may be seen in the fluid in the middle ear space. Mucoid OME has a yellow to white or creamy color with a bulging, normal, or retracted position. Mobility is also usually decreased (Fig. 8.3). The findings in OME contrast with the findings in AOM. Here the patient may or may not complain or ear pain. The tympanic membrane will be red with prominent vessels. There will be effusion in the middle ear space, often purulent in appearance, and the tympanic membrane will appear in a normal or bulging position. Mobility will also likely be decreased (Fig. 8.4).
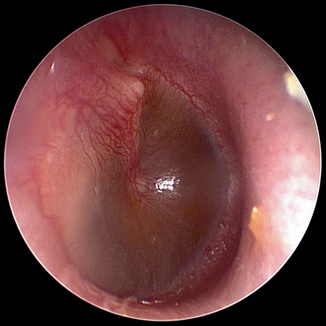

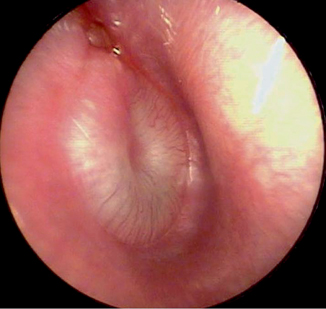
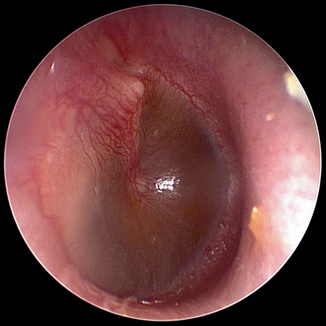
Fig. 8.2
Otoscopic exam: serous otitis media

Fig. 8.3
Otoscopic exam: mucoid effusion with bubbles
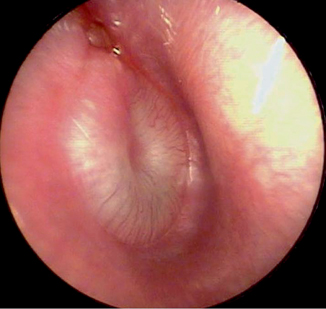
Fig. 8.4
Otoscopic exam: AOM
Of paramount importance is making the correct diagnosis for a patient with otitis media as the diagnosis will determine the treatment. The 2013 Clinical practice guideline: Diagnosis and Management of AOM from the American Academy of Pediatrics (AAP) [6] built upon and further clarified diagnostic criteria set forth in the 2004 AAP guidelines [7]. The 2004 guidelines used a three part definition of AOM with (1) acute onset of symptoms, (2) presence of MEE, and (3) signs of middle ear inflammation. Criticisms of these criteria were that they lacked precision to exclude OME and permitted the diagnosis of AOM in cases of acute onset of symptoms with otlagia and MEE but without other signs of inflammation on otoscopy. Additionally, the 2004 guidelines included a category for “uncertain diagnosis” which may have permitted diagnosis of AOM without clear visualization of the tympanic membrane. The 2013 guidelines qualify these criteria and states that the diagnosis of AOM:
1.
Should be made in children who present with moderate to severe bulging of the tympanic membrane (TM) or new onset otorrhea not due to acute otitis externa
2.
Should be made in children who present with mild bulging of the TM and recent onset (less than 48 h) of ear pain (holding, tugging, and rubbing of the ear in a nonverbal child) or intense erythema of the TM
3.
Should not be made in children who do not have MEE (based on pneumatic otoscopy and/or tympanometry)
Critically, the new guidelines place great importance on the otoscopic exam of the patient to make the correct diagnosis. A study by Karma et al. [8] looked at over 2900 children over the course of 2 years at two separate sites—totaling over 11,000 visits. Physical exam findings, the color, position, and the mobility of the TM were recorded. AOM was diagnosied if the child had MEE and fever, earache, irritability, ear rubbing or tugging simultaneous other upper respiratory symptoms, vomiting, or diarrhea. Tympanocentesis was performed but no culture was obtained. Of the acute visits in the study, MEE was found in 84.9 and 81.8 % at the two sites. Of the exam findings, a cloudy, bulging TM with impaired mobility was the best predictor of AOM. Impaired mobility had the highest sensitivity (95 %) and specificity (85 %). Individually, cloudiness was 74 % sensitive and 93 % specific. Bulging TM was only 51 % sensitive, but 97 % specific. Several other studies support the value of the bulging TM on physical exam [9, 10] moderate to severe bulging of the TM is the most important characteristic in the diagnosis of AOM [6].
In looking at the presenting symptoms of AOM, ear pain had the highest combined positive likelihood ratio (3.0–7.3) in a 2003 review by Rothman et al. [11]. In three studies cited, Niemela et al. reported 54 % sensitivity and 82 % specificity of ear pain [12]. Heikkinen reported 60 % sensitivity and 92 % specificity [13] and Ingvarrson reported 100 % sensitivity, though did not report specificity [14].
Despite its usefulness as a symptom to be used in the diagnosis of AOM, ear pain is only present in 50–60 % of children with AOM [11]. Other signs, restless, ear rubbing, fever, non-specific respiratory complaints, diarrhea do not appear to be helpful in the diagnosis of AOM.
Takata et al. reviewed the accuracy of eight methods of diagnosing OME [15]. Pneumatic otoscopy was found to have the best performance with a sensitivity of 94 % (95 % CI 92–96 %) and a specificity of 80 % (95 % CI 75–86 %). Pneumatic otoscopy was compared to acoustic reflectometer, portable tympanometry and several variations of professional tympanometry. All included studies used myringotomy as internal diagnostic comparison. Only one of the included studies on pneumatic otoscopy was performed by validated otoscopists [16]. Additionally, the author notes that audiometry, binocular microscopy and nonpneumatic otoscopy could not be included in the analysis because of inadequate evidence. In a small study, Rogers et al. looked at 201 ears in 102 patients and found that binocular by a staff pediatric otolaryngologist was the most sensitive in diagnosing OME with 88.0 % sensitivity (95 % CI 81.4–94.7) and 89 % specificity (95 % CI 83.1–94.9). Resident binocular microscopy was the next most sensitive, followed by staff pneumatic otoscopy and resident pneumatic otoscopy. Thus, as would be expected, there is improved performance garnered from additional years of training and experience. Interestingly, however, even the resident exam was more specific that the tympanometer 78.4 % (95 % CI 70.4–86.4) to 47.7 % (95 % CI 38.3–57.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




