Fig. 3.1
Age-related disk modifications, d isk bulging and disk herniation shown on sagittal FSE T2 images. Patient 1 (a) Minimal disk dehydration at C3-4 level (arrow), as demonstrated by low intensity signal on T2 images. Patient 2 (b) With progression of degenerative changes, disk height is reduced and associated with mild spondylotic alteration at C4-5 level (arrow). Patient 3 (c) Posterior disk bulging at C6-7 level (arrow). Patient 4 (d) Disk herniation at C6-7 level (arrow)
1.
Loss of signal intensity of disk (MR imaging)
2.
Loss of height (all imaging modalities)
3.
Bulging (CT or MR imaging)
4.
Herniation (CT or MR imaging)
The radial tear of the annulus that is often strictly associated with the other features, is to be considered the primary failure of the annulus itself [14]. The radial tear involves all layers on the annulus fibrosus and it is well described in MR imaging as high signal intensity tissue in the region of the disk normally characterized by low signal intensity [15].
The disk degeneration processes evolve in a progressively loss of water, with a compromised integrity of the annulus fibrosus.
On MR imaging these signs are well evident on T2-w fast spin echo (FSE) or gradient echo (GRE) images with a loss of normal hyperintensity of signal and an associated loss of height (often a vacuum phenomenon is demonstrated in CT or radiography). Frequently the disk degeneration is associated with an alteration of adjacent intervertebral body endplates (intervertebral osteochondrosis).
Modic [16] distinguishes three progressive grades of alteration adjacent to the endplates on MR imaging (Fig. 3.2), partially corresponding to the sclerosis described in radiographic or CT examination:
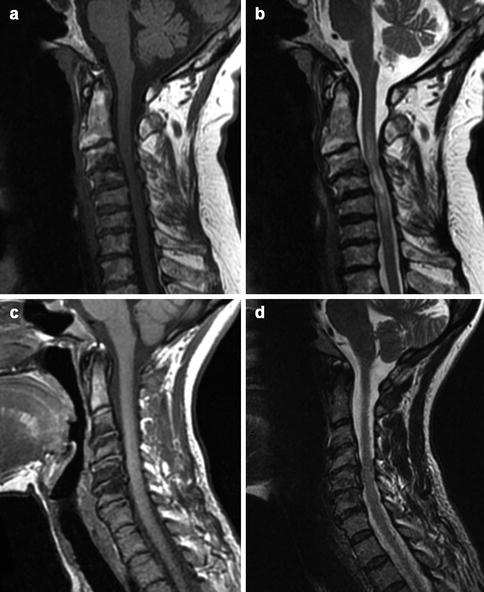
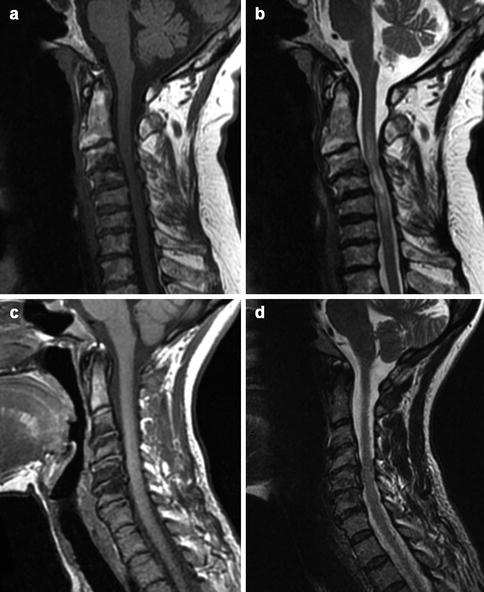
Fig. 3.2
Modic 2–3 alterations on sagittal FSE T1/T2 images. Patient 1: FSE sagittal T1 (a), FSE sagittal T2 (b). The vertebral endplates at C2-3 level show hyperintensity on both imaging sequences, due to the conversion of normal into yellow fatty marrow (Modic 2). Spondylosis results in spondylotic myelopathy as demonstrated by intrinsic high signal of the compressed spinal cord. Patient 2: FSE sagittal T2 (c), FSE sagittal T2 (d). The vertebral endplates at C5-6 show hypointensity on both sequences, representing subchondral bony sclerosis (Modic 3)
Type I: hypointense on T1-w and hyperintense on T2-w bands which represent the replacement with hematopoietic marrow
Type II: hyperintense T1-w and iso/hyperintense T2-w bands which represent the replacement by fatty marrow
Type III: hypointense T1-w and T2-w bands which are characteristic of bone sclerosis.
The endplates bony marrow changes associated with degeneration disks may be however distinguished from the other diseases such as infection and metastases.
Spondilosys
Dehydration and fibrosis of the disk mean that static and dynamic mechanical stress can no longer spread through the horizontal plane of the disk, without altering it structurally. The disk becomes the seat of fissures, protrudes out and becomes thinner. Because of the displacement of disk material beyond the margins of the intervertebral disk space, a productive reaction is established, producing fibroblasts, in the adjacent vertebral margins: these phenomena determine spondylosis pathogenesis.
Osteophytes are the most characteristic sign of spondylosis and are more commonly found at levels C5-7; at the beginning they are thin and have a horizontal course to become gradually larger until they weld in the more advanced stages. Uncovertebral joints osteophytes characterize the framework of mono- or bilateral uncoarthrosis: they push into the vertebral foramina and can compress the spinal root and into the intertransverse space, where they take relationship with the vertebral artery [17].
Interapophyseal joints osteophytes that protrude into the foramina will generally occupy the upper part and rarely are able to cause a radiculopathy by themselves. Instead they contribute to cause it in the presence of lateral herniated disk or severe uncoarthrosis. The development of anterior osteophytes in cervical spondylosis is usually modest and asymptomatic. Both radiography and CT can well demonstrate osteophytes. Even in the MR imaging, osteophytes can be well studied with T2*-w sequences that well demonstrate bone structures, distinguishing from the adjacent degenerated disk.
Cervical Facet Arthropathy
The degenerative facet disease or arthropaty is to be considered an osteoarthritis of sinovially lined apophyseal joints. Each apposing facet is composed of a thin uniform layer of dense cortical bone, and an overlying layer of cartilage. The facet joint is lined by synovium.
The degenerative process is not different from other synovial joints. It starts with hypertrophic degenerative inflammatory changes, following by subluxation that may produce gas (vacuum phenomenon). Lately there is a cartilage erosion with narrowed joint space. It is most common in mid lower cervical spine.
Radiologically the early degenerative signs maybe be difficult to demonstrate, while the later changes are well evident in radiography (facet arthrosis, vacuum phenomenon, mushroom caps facet appearance, sclerosis). CT with soft tissue window level well demonstrates the thickening and inflammatory changes of soft tissue better visualized with the injection of contrast media. MR imaging shows a better visualization of the inflammatory changes and the facet effusion (linear T2-w images hyperintensity), but overestimated with the T2*-w images the degree of foraminal and central canal narrowing.
Ligament Degeneration
Cervical ligaments also undergo degenerative changes, represented by the precipitation of calcium salts and the appearance of new bone formation, which compromise their firmness and elasticity. It should also be remembered that it is sufficient the involvement of disks and/or synovial joints to induce ligamentous laxity, consequently alteration that entails the functional spinal unit (FSU). A FSU consists of two adjacent vertebrae, the intervertebral disk and all adjacent ligaments between them.
The calcified depositions and ossification are most frequently found in the flaval ligaments and especially in the anterior and posterior longitudinal ligaments.
Degenerative Cervical Spine Instability
Stability can be defined as the ability of the vertebrae to maintain normal relations between them and to contain their mutual displacements, under the action of postures and physiological loads. In normal conditions, the geometric characteristics of the vertebrae, a normal intradiscal pressure, the configuration of the facet joints and, above all, a correct ligament tension are able to maintain stable motion segments. When the above conditions are not preserved, the spine becomes unstable.
Despite the efforts of numerous authors to define the spinal instability, there is not a definition shared by all; one of the biggest problems is that the concept has different meanings in various areas of clinical radiology and bioengineering. However, a reasonable definition has been proposed by White and Panjabi [18] that by supporting a biomechanical approach , define instability as a loss of “stiffness” of the motion segment in correspondence of which, under the action of a load, the motion determined abnormal displacement. In biomechanical sense, the “stiffness” is defined as the ratio between the loads applied to the structure and the resulting movement. The instability of the spine may be the consequence of a trauma, of a degenerative disease and various other causes.
This premise is fundamental to allow an interpretation of cervical degenerative instability not as a mere list of topographical radiological signs but as an alteration of the spinal disk-ligamentous complex as a whole. The various degenerative changes must be inserted in well-defined pathological successive phases according to Kirkaldy-Willis [19], which are:
Phase of functional derangement
Phase of instability
Phase of fixity
Phase of Functional Derangement
Degenerative changes in the initial (disk fissures and apophysis’ synovitis) determine an interapophyseal joints stress that leads to a modest hypermobility of the vertebrae. Consequently, the hypermobility causes a repeated stress of nerve fibers with the onset of cervical acute pain. Facet joints subluxation can be associated with a disk herniation or a symptomatic synovitis. At this phase the radiography is negative, so in the suspicion of a herniated disk is necessary to perform CT or MR imaging.
Phase of Instability
Going on the functional derangement, degenerative phenomena worsen both on disco-somatic complex (i.e. reduction of disk space, vacuum phenomenon, intervertebral osteochondrosis) and on zygapophyseal joints (sclerosis, “mushroom” deformation of articular pillars, articular effusion). Consequently radiculopathy or myelo-radiculopathy may spread out at this phase as a result of disk herniations and also a spondylolisthesis of the vertebra affected (degenerative spondylolisthesis) may result in dynamic narrowing of central canal and/or foraminal stenosis. The radiography, when performed in LL projection in flexion and extension (dynamic study) is able to detect not only the degree of listhesis but also to determine if it is reducible or fixed (Fig. 3.3).


Fig. 3.3
Degenerative instability on flexion/extension radiography. Flexion (a) and extension (b). Minimal degenerative spondylolisthesis C3-4 evident on the flexion radiogram (arrows, “phase of instability” according to Kirkaldy-Willis) with complete reduction on extension radiogram
Phase of Fixity
The findings are those of advanced osteoarthritis, with loss of motion, joint deformation and above all an increase in osteoproliferative phenomena (osteophytes and hypertrophy of the articular pillars); these alterations may lead to central canal stenosis. Conventional radiology is able to highlight osteoproliferative changes but not to assess their effects on neurovascular structures, and therefore they should be investigated with CT and MR imaging.
Cranio-Cervical Junction Degenerative Disease
The joint most frequently subject to degenerative changes in the craniocervical junction is the atlanto-odontoid. Atlantoaxial advanced degenerative changes are the main cause of the onset of symptoms (headache), with concomitant reduction in mobility.
Also, it has been suggested that the onset of vertigo can be referred to a strict relation between upper cervical spine afferent fibers and vestibular and oculomotor nuclei [20].
Sometimes degenerative changes can lead to the formation of abundant inflammatory reactive tissue, mainly posteriorly to the odontoid process that could determine an encroach on the ventral surface of the spinal cord (inflammatory pseudotumor).
Imaging
CT and MR axial images, as in the subaxial cervical spine, provide a good evaluation of the spinal canal stenosis which is often associated with the degenerative changes in the cranio-cervical junction; MR imaging is also capable to evaluate the medulla oblongata compression and its lately onset of myelomalacia (characterized by hyperintensity on T2-w images). Moreover, the MR imaging can differentiate hypertrophic pseudotumoral changes of the CCJ (Fig. 3.4). Post-contrast images a re useful to exclude/identify inflammatory changes (pannus).
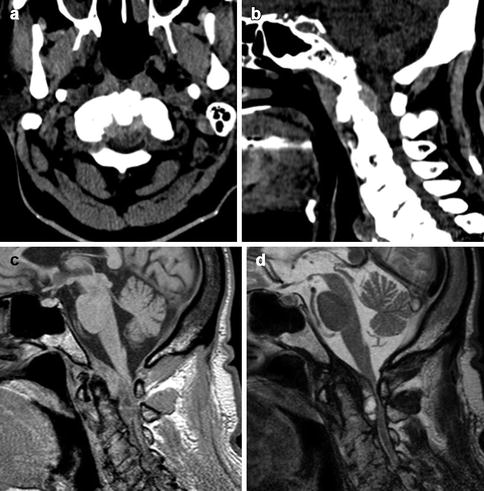
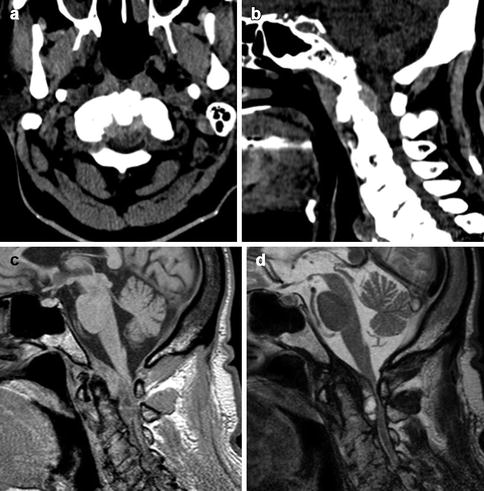
Fig. 3.4
Pseudotumor of the CCJ; CT and MR imaging. CT axial (a) and sagittal (b) images, sagittal GRE T1 (c) and FSE T2 (d) images. Abundant retro-odontoid inflammatory tissue at C0-C1 level, resulting in severe spinal cord compression
Subaxial Cervical Spine Degenerative Disease
Cervical Disk Herniation
Terminology
The general term of herniated disk means the displacement of disk material beyond the margins of the intervertebral disk space and represents one of the major causes of neck pain. There are not universally accepted terminology and classification to define various pattern of disk herniation; different words are often used to describe the same type of hernia. A purely pathological classification of disk herniations is not suitable in daily radiological practice; i.e., the terms disk prolapse or disk herniation, respectively indicating that a portion of the nucleus pulposus has made its way through a fissure that involves only the innermost fibers of the annulus (prolapse), and the disk material that has gone through the whole annulus fibrosus, but not the posterior longitudinal ligament (disk herniation). However, since these two conditions pathological are not differentiable from each other even with MRI (both can manifest as focal contour deformities of disk), it is better not to make such a distinction. Morphologically we can distinguish protruded from extruded hernias: a disk protrusion is a herniated disk in which the distance between the edges of the disk herniation is less than the distance between the edges of the base; conversely, a disk extrusion is a herniated disk in which the distance between the edges of the disk material is greater than the distance at the base [21, 22].
Even if a universally accepted classification is not forthcoming yet, differentiation between the “bulging disk” by “hernia” is necessary.
Bulging Disk (Fig. 3.5)
Fig. 3.5
Bulging disk. Sagittal FSE T2 (a) and axial FSE T1 (b) images. The C4-5 disk presents minimal diffuse bulging of its margins, with minimal effect on the ventral surface of the thecal sac
The “bulging disk ” is characterized by wide/diffuse displacement of disk material beyond the normal limits of the intervertebral space, while the herniated disk is instead a focal dislocation. For wide/diffuse dislocation is meant a dislocation that affects more than 50 % (180°) of the circumference of disk, while a dislocation is defined focal when interesting not more than 25 % of the circumference of the disk. It is important to emphasize that the “bulging disk”, very common over forty, may be associated with reduction in disk height and does not necessarily represent a pathological condition.
In the presence of a bulging disk, the posterior dislocation of the disk tissue is typically symmetrical and maximum on the median line, but occasionally it is possible to observe also a focal disk displacement on one side. In a relatively narrow spinal canal, the bulging disk can flatten the dural sac surface, but only rarely and in the presence of a marked stenosis, results in a true compression of the spinal cord or nerve roots.
Types of Hernia
A herniated disk can occur in any direction, although those that have clinical relevance occupy the spinal canal or radicular canal and encroach the dural sac and/or nerve roots.
According to the location they are divided as follows (moving from central to lateral):
“Central” hernia extends into the spinal canal along the midline, compresses and deforms the epidural surface of the dural sac and sometimes, according to its size, is so voluminous as to determine a bilateral radiculopathy and/or myelopathy (Fig. 3.6);
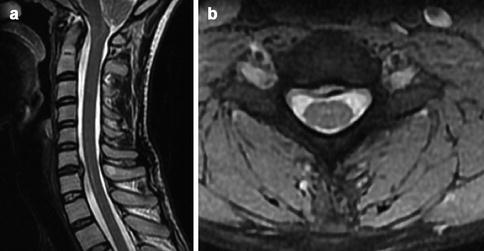
Fig. 3.6
Central disk herniation. Sagittal FSE T2 (a) and axial GRE T2 with fat suppression (b) images. There is focal C6-7 protrusion/herniation of disk material deforming the ventral surface of the thecal sac on the midline
“Lateral/Paramedian” (Right/Left) hernia: not on the median line, but does not extend into the lateral recess. The herniated material displaces the epidural fat and may occupy the lateral recess, at the origin of the nerve root. It is responsible for a unilateral radiculopathy (Fig. 3.7);