Joseph F. Drazkowski
Electroencephalography (EEG) is a diagnostic procedure that measures temporal changes in summated postsynaptic potentials from the superficial layers of the cerebral cortex. Currently, EEG is used principally in two major areas of clinical practice: seizure disorders and alterations in mental status. Technologists connect electrodes to the patient and record and store the EEG data. After the study is completed, physicians with specialized training interpret the stored data. In emergency situations, such as status epilepticus, the EEG may be viewed while it is being recorded. The technologist places a series of electrodes in symmetric locations according to the International 10-20 System on the scalp. The EEG signals are amplified and stored on a specialized digital recording device. A routine EEG is recorded for about 30 minutes but may be recorded for periods of days as required by the clinical situation. While the EEG is being recorded, the technologist documents the patient’s behavioral state (i.e., awake, asleep) by asking the patient to perform certain tasks to judge the level of alertness. Hyperventilation and photic stimulation are performed by the patient during the recording if the patient is physically able to do so. These procedures, along with having the patient fall asleep during the EEG, are called “activation procedures” because they have the potential to provoke a seizure or abnormal EEG activity. The technologist observes and notes on the record any alteration in responsiveness, abnormal movements, seizure activity, or responses to noxious and auditory stimuli. If status epilepticus is found during the recording, a physician may administer antiepileptic drugs (AEDs) intravenously during the study to determine the effectiveness of therapy. An EEG may be recorded for a longer duration, either with concurrent video monitoring in the hospital in a specialized monitoring unit or in the ambulatory setting with a portable Holterlike recording device for up to several days. Video EEG recording is used to correlate electrographic activity with clinical behavioral features. Video EEG is especially useful in the classification of spells or in the surgical evaluation of a patient with medically refractory partial epilepsy. Ambulatory EEG is limited by the lack of video correlation with behaviors and is prone to technical artifacts.
NORMAL ELECTROENCEPHALOGRAM
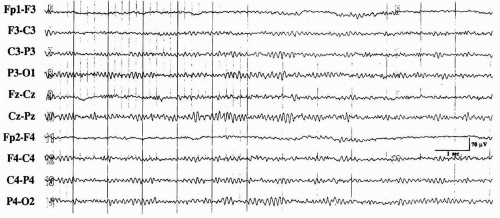
The normal EEG remains relatively unchanged from adolescence until at least 80 years of age. In interpreting EEG studies, the reader must be familiar with changes that may be explained by age and behavioral state. EEG rhythms are divided into four normalfrequency bands: delta (<4 Hz), theta (4 to 7 Hz), alpha (8 to 13 Hz), and beta (>13 Hz). The normal EEG signals are low voltage in comparison to EMG and ECG with the average background activity (“alpha rhythm” or posterior dominant rhythm) being about 50 mV during the waking state. A mixture of faster and slower frequencies predominates over the more anterior head regions during the waking state. In people over 60 years of age, the EEG is not distinguishable from other normal adults; in people over 80 years of age, some slowing of this dominant posterior rhythm is considered normal, along with some increase in brief intermittent focal slowing in other areas.
Hyperventilation may provoke physiologic slowing of the background rhythm and further intermittent slowing in many normal subjects, but this is commonly absent in the elderly. Photic stimulation can evoke a repetitive, time-locked occipital rhythm (so-called photic driving response) with the same photic stimulus in normal subjects. Hyperventilation and photic stimulation are known to provoke seizures and abnormal epileptiform activity in prone individuals. Characteristic EEG features in the EEG background determine the various stages of non-rapid eye movement (REM) and REM sleep. In many patients with epilepsy, the
sleep-deprived and sleep EEGs may activate abnormalities and improve the diagnostic yield of the test.
sleep-deprived and sleep EEGs may activate abnormalities and improve the diagnostic yield of the test.
NORMAL EEG CHANGES IN THE ELDERLY
Extensive literature describes normal EEG changes in the elderly. Some variation in what is considered normal exists, chiefly because of the care involved in case selection. Recent studies indicate that truly normal elderly people show remarkably well-formed EEG rhythms that cannot be distinguished from younger patients.
DOMINANT BACKGROUND FREQUENCY
Hubbard et al. (10) reported EEG findings in 10 centenarians. Seven of the 10 were living in the community and were considered generally healthy. Six of these seven had a background alpha frequency of 8 Hz or faster. In four separate studies of patients aged 60 to 80 years (3,7,11,21), the mean alpha frequency was approximately 9.5 Hz. Therefore, in healthy people 80 years old and older, an alpha frequency of 9 Hz should be expected (Fig. 3-15). After age 50, alpha frequency activity may appear in either temporal region, especially the left. It is often higher in voltage than occipital alpha and is considered to be normal. Fragments of this temporal alpha can appear as wicket spikes, which is an epileptiform variant seen in older adults and the elderly that will be discussed later.
INTERMITTENT FOCAL SLOWING
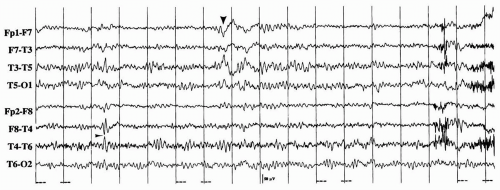
Intermittent focal slowing, especially in the left temporal region (Fig. 3-16), was considered a normal finding after mid-life (19). However, recent studies in which patients have been rigorously screened suggest that this finding, when present, should be infrequent. Katz and Horowitz (11) found intermittent focal slowing in 17% of 52 normal septuagenarians, but in
no patient did it occupy more than 1% of the total record. Arenas et al. (3) found slowing in 18 (36%) of 50 subjects. Theta activity was present in all 18 subjects, but delta activity was present in only six (12%). The combined theta and delta activity occupied less than 1.8% of the total recording in all but one subject. Maximal temporal slowing was left-sided in 72% of these patients. Intermittent slowing was best displayed on the transverse bipolar montage.
no patient did it occupy more than 1% of the total record. Arenas et al. (3) found slowing in 18 (36%) of 50 subjects. Theta activity was present in all 18 subjects, but delta activity was present in only six (12%). The combined theta and delta activity occupied less than 1.8% of the total recording in all but one subject. Maximal temporal slowing was left-sided in 72% of these patients. Intermittent slowing was best displayed on the transverse bipolar montage.
Visser et al. (22) correlated EEG, neuroimaging, and neuropsychological data in 27 “normal” subjects aged 65 to 83 years (mean age, 78 years). Patients were divided into those with left frontotemporal slowing and those with normal EEGs. Patients with focal delta slowing demonstrated significantly decreased performance on verbal fluency tests and ventricular dilatation on head computed tomography. How frequent the intermittent focal slowing (delta waves) and the amount of focal delta slowing on the record determines whether the record is normal or abnormal.
Substantial variation exists among electroencephalographers interpreting focal slowing. Figure 3-16 is an example of a routine EEG in a 73-year-old patient with new-onset complex partial seizures. The normal phenomenon of sharply contoured alpha transient is seen in the third second in the right temporal region (arrowhead). The abnormal feature of this patient’s EEG was the high-amplitude, sharply contoured slowing seen over the left temporal region, which is highlighted with the large arrowhead. No interictal epileptiform activity was seen on the record.
CHANGES IN SLEEP OR DROWSINESS
Katz and Horowitz (12) reported the abrupt onset of drowsiness or sleep in healthy normal septuagenarians with frontally dominant rhythmic delta activity of 1 to 4 Hz and 40 to 150 µV for at least 3 seconds at a time. This activity is indistinguishable from the pathologic frontal intermittent rhythmic delta activity (FIRDA). Changes also occur in non-REM sleep and sleep cycles. In Stage II sleep, K-complexes and spindles of Stage II sleep are noted to be decreased in amplitude, number, and duration compared with younger adults (8). The delta activity of Stages III and IV is lower in voltage compared to younger people. Septuagenarians also spend less time in slow-wave sleep (13).
BENIGN EPILEPTIFORM VARIANTS
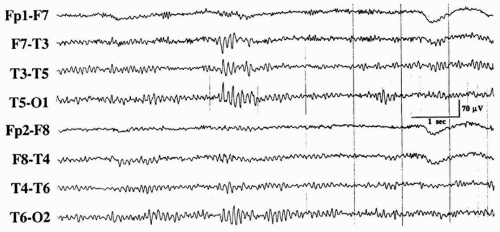
Two benign variants occur frequently in middle-aged and older people. Wicket spikes consist of monophasic, arciform, 6- to 8-Hz waves seen maximally in the temporal regions with a tendency to occur in brief trains of about 1 second (Fig. 3-17) (17). Although these wicket spikes occur in wakefulness, they are often masked by normal background activity. Occasionally, they appear singly when they retain the morphology of the individual waves in a train. Wicket spikes occur in a bitemporal, independent fashion, with approximately equal frequency over each hemisphere. Wicket spikes must be distinguished from anterior or middle temporal focal spikes. Wicket spikes have no correlation with epilepsy or any particular symptom complex, as opposed to anterior temporal spikes, which are correlated with seizures.
Subclinical rhythmic EEG discharge of adults (SREDA) (23) consists of repetitive, bilateral, temporoparietal theta discharges with abrupt onset and termination without any clinical accompaniment. SREDA is usually seen during waking in older adults and is a gradual change of frequency reaching 4 to 7 Hz and lasting 40 to 80 seconds before stopping. SREDA occurs in patients with diverse clinical complaints and is not associated with a clinical history of seizures. In some patients, it can be triggered by hyperventilation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree