Disorders of Mental Development
Marcel Kinsbourne
Frank B. Wood
A host of neurologic disorders with onset early in life compromise mental development. The cognitive impairment may be one among many neurologic abnormalities, or it may be the dominant feature. Even in the latter case, less prominent neurologic signs and symptoms are usually also to be found, and no clear neurobiologic distinction can be made between syndromes of mental dysfunctions and other brain disorders. This chapter treats in detail those disorders in which the mental development component is key. Where disordered mental development is one of many abnormalities, the mental component is briefly summarized, and the reader is referred to other chapters for more comprehensive discussion of the entity in question.
A developmental disability is an impairment in behavioral development due to abnormality of the central nervous system. Developmental disabilities manifest during the developmental period and result in lifelong impairment in any combination of physical, cognitive, sensory, speech and language, and neuropsychologic functions. Beginning with the formation of the neuroectoderm, the developmental period is in principle not complete until the end of myelinization during the decade of the twenties. In practical terms, however, the general category of developmental disorders reflects alterations in neural maturation that manifest most often and most prominently in the preschool and early grade school years. This chapter considers the nature, diagnosis, and management of those developmental disorders and disabilities that implicate higher cortical function—that is, cognition and attention.
NATURE OF DEVELOPMENTAL DISORDERS
Postnatal neurologic maturation underwrites the gradual acquisition of an extensive repertoire of cognitive skills. The newborn is devoid of cerebrally controlled behavioral patterns, so that in the first 6 weeks of life it is hard to distinguish the normal newborn’s behavior from that of an anencephalic infant. Different brain regions progressively assume control over specific functions in predictable sequence and timing—brainstem before cerebrum, sensorimotor projections before integrative cortex. Late-developing skills, typically subserved by late-maturing prefrontal cortex (1), develop over many years, at least until late adolescence, before the skill in question asymptotes to its ultimate adult level (2).
A developmental disorder typically becomes apparent when a specific ability fails to present within the normatively expected time frame. It induces an unexpected low point in the child’s cognitive profile, a selective deficit. In the general childhood population, there is a high correlation between an individual’s performance on a wide range of mental tests, a phenomenon that has given rise to the construct of g, or general intelligence. Some two-thirds of the interindividual variance in the overall intelligence quotient (IQ) of the general population reflects genetic diversity (3,4). Variations in the prenatal and postnatal environment account for the remainder. Even in the general population, aspects of brain structure correlate with IQ: Intracranial, cerebral, temporal lobe, hippocampal and cerebellar volume as well as gray matter volume account for between 12% and 31% of the variance in IQ (5). However, many adverse biologic, genetic, environmental, and gene-environment interactions can reduce the rate of intellectual development, either globally, causing mental retardation, or selectively, compromising some components of intelligence only. IQ tends to be higher in those who were heavier at birth or who grew taller in childhood and adolescence. In a study of normal nine-year-old children, IQ at age 9 rose by about two points for every standard deviation increase of head circumference at 9 months and by nearly three points for every standard deviation increase at 9 years. It appears that postnatal head growth, at asymptote between age 14 and 16, is more important than prenatal head growth in determining cognitive function. Postnatal head growth correlates positively with mothers’ height and weight, socioeconomic status (SES), and educational level (6).
Selective cognitive deficit results in “intertest scatter,” such that the child scores within the normal range on some tests, but disproportionately poorly on those that tap
developmentally compromised cognitive processes. Such scatter between normally and slowly developing skills is typical of learning disabilities. Any cognitive skill may be selectively impaired, but it is the impairments that have social consequences that attract attention. Those selective cognitive deficits that result in delayed language development, abnormal play, and defective social skills commonly become apparent during the second and third years of life. Selective deficits in attention, concentration, and learning that leave a child lacking readiness for instruction in academic areas may not be recognized until the preschool or grade school period. Such disorders are usually diagnosed on functional and behavioral criteria, whether or not biologic validation of the diagnosis is feasible.
developmentally compromised cognitive processes. Such scatter between normally and slowly developing skills is typical of learning disabilities. Any cognitive skill may be selectively impaired, but it is the impairments that have social consequences that attract attention. Those selective cognitive deficits that result in delayed language development, abnormal play, and defective social skills commonly become apparent during the second and third years of life. Selective deficits in attention, concentration, and learning that leave a child lacking readiness for instruction in academic areas may not be recognized until the preschool or grade school period. Such disorders are usually diagnosed on functional and behavioral criteria, whether or not biologic validation of the diagnosis is feasible.
In some cognitive domains, normal development continues until late in adolescence. Examples of this include executive functions, such as the capacity of working memory and cognitive flexibility (7). A recent imaging finding that dorsolateral frontal activation continues to develop in adolescence (8) is provocative but may only show that adolescents tend to underutilize that cortex, rather than that they are as yet incapable of using it. Developmental delays usually reach an end-point of persisting cognitive deficits by late adolescence, within the same time frame as that in which normal development asymptotes. In general, gradual improvement is common, though some is due to statistical regression artifact. But some improvement reflects genuine progress as the child sorts out the most relevant and controlling stimuli of life, school, and work, thereby reserving the most effort at improvement for the areas that promise the most gain. A child’s brain may compensate, reorganize, and mature, and special education may offer systematic practice of impaired skills, combined with alternative training that circumvents the cognitive limitation (“bypass”). In other instances, cognitive abilities gradually deteriorate, as in increasingly intractable seizure disorder and secondary behavioral disorder. Or development may be predestined genetically to decelerate gradually, as in Down syndrome. However, usually the child makes gains over time but with a ranking relative to his typically functioning peers that does not appreciably change. Notwithstanding that, the gap in adolescence is usually rather more obvious than it is around school entry. Such a child’s level of functioning is quantitatively insufficient for his chronologic age and instead is as would have been expected in a younger child.
TABLE 18.1 Typical Cognitive and Language Developmental Milestones of Infancy and Childhood | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
NEURODEVELOPMENTAL LAG
Normative cognitive and language developmental milestones are presented in Table 18.1. In neurodevelopmental lag, the effects of an early brain lesion or maldevelopment become increasingly apparent many months or years later as cognitive milestones are slow to be reached and immature patterns of sensorimotor control persist. The newborn has a limited repertoire of innate movement patterns. These synergisms subserve activities such as rooting, sucking, startle, and lateral orienting, which occur spontaneously or as reflexive responses to stimulation. Synergisms gradually disappear according to a well-delineated schedule in the course of infancy or childhood. The overall trend of motor development is toward increasingly precise control over an ever widening repertoire of discrete movement combinations (9); sensory development tends toward a finer, more exact differentiation between various stimuli (10).
In neurodevelopmental lag, synergisms may persist, presenting as “soft signs” on the neurologic examination. Soft signs are signs that would have been normal had the child been younger. Motor soft signs are of two kinds: (a) unwanted movements (e.g., persistent asymmetrical tonic neck response, unwanted associated and mirror movements); and (b) imperfect execution, such as slowness in speeded sequential activities such as finger tapping or finger-thumb sequencing, or in alternating movements, such as pronation-supination of the forearm or flexion-extension at the ankle (dysdiadochokinesis). In the absence of long tract signs, dyspraxia, or clumsiness, is diagnostically nonspecific (see discussion of developmental coordination disorder below).
Delayed development proceeds through the same stages as normal development, although at a slower rate. Thus, with increasing age and neurologic maturation, scores on quantitative scales for soft signs decline, regardless of diagnosis (11). Considerable consistency in neuromotor developmental status has been demonstrated over periods as long as 10 years (12). Signs of sensorimotor immaturity are often lower-level analogues to later emerging cognitive immaturity, behavioral problems, and attention deficits. Early signs of developmental delay indicate a high risk of long-term functional developmental disabilities, depending on the distribution and severity of the underlying cause, but these associations do not provide an adequate basis for prognosis. For instance, an association exists between persisting mirror movements and aggressive psychopathology, perhaps because both are manifestations of disinhibition (13). Excessive, uncontrollable crying that persists beyond 3 months of age has been associated with a shortfall of some nine IQ points relative to controls with colic only in a prospective study (14).
Neurodevelopmental lags that involve both cognitive and sensorimotor control have been bracketed together as “minimal brain dysfunction” (MBD) (15). This construct was intended to indicate organicity, so as to counteract the now virtually extinct tendency to ascribe developmental delays to intrapsychic problems. A similar construct, intended to be descriptive rather than making hard-to-prove claims about the brain, has gained acceptance in Scandinavia. This is the collective labeling of children with childhood onset of deficits in attention, motor control, and perception with the acronym DAMP (16). These disparate neurocognitive immaturities may or may not affect specific academic skills. A clinical level of deficit is reached by 1.5% of the childhood population. The syndrome does not indicate any particular etiology (17), and its antecedents do not differ qualitatively from those of major brain dysfunctions such as cerebral palsy or mental retardation, which also are end results of a host of different neuropathologies. The extent to which development is impaired depends on the anatomical distribution and the severity of the insult, rather than its cause. Despite their substantial comorbidity (18), neuropsychologic testing does not reveal any functional overlap between the motor and the attentional components. The practical usefulness of the MBD/DAMP construct is limited by the fact that each component of the syndrome is managed in the same way when it coexists with the other ones, as when it is present in isolation.
CLASSIFICATION OF DEVELOPMENTAL DISORDERS AND DISABILITIES
Ideally, disorders of cognitive development are classified on both an etiologic and a descriptive and functional basis. However, many patients have developmental disorders “of uncertain etiology.” In the absence of a precise medical diagnosis, it is preferable to record the chief characteristics of the abnormal developmental process rather than to make inferences such as “cerebral dysfunction,” “organicity,” or “static encephalopathy.” The characteristics include qualitative and quantitative descriptions of the mental status, including use of language, play skills, visual and auditory recognition, reasoning, orientation to spatial relationships, impulse control, and the ability to sustain attention.
Most neurodevelopmental disorders that result in mild disability affect quality of life but do not curtail longevity. The children require no more than the customary standard of medical care throughout their lives. Any need for additional specific medical interventions for certain neurologic disorders (e.g., diets for metabolic disorders or epilepsy, pharmacologic treatment for severe behavioral problems), or for nonmedical therapy programs, should be re-evaluated periodically for evidence of cost-effectiveness on long-term outcome.
PRACTICAL APPROACHES TO NEURODEVELOPMENTAL DISORDERS
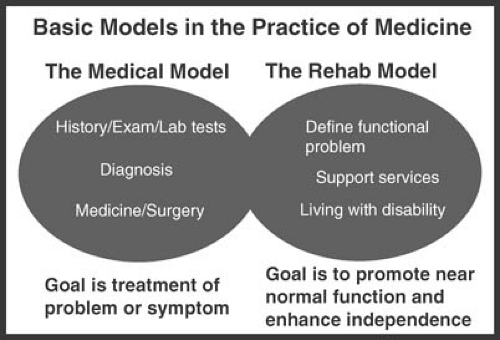
The medical model and the habilitation model (Fig. 18.1) are complementary, and both are fundamental to clinical practice. The habilitation model is particularly relevant when, as in disorders of mental development, there generally are few means of offering complete symptomatic relief and fewer still of outright cure. By federal law, the Individuals with Disabilities in Education Act (IDEA)—the habilitation/rehabilitation model for developmentally disabled children—is the programmatic and financial responsibility of local education authorities, assisted to a varying extent by federal funding.
Medical Diagnosis and Treatment
Developmental disorders have a wide variety of causes, and few have a specific, identifiable genetic or neurobiologic etiology. Different etiologies converge on identical
behavioral phenotypes. The diagnostic yield is much greater if there is associated microcephaly, antenatal toxin exposure, or focal findings (19). In their absence, a thorough search for diagnostic clues includes family history with a three-generation pedigree and information from the prenatal, perinatal, and early postnatal periods. The development of motor skills; comprehension of speech; emergence of words and formed, intelligible sentences; and quality of social play skills are often relevant. The physical examination includes measuring head circumference as well as body size and growth; assessment of vision, hearing, and ocular funduscopy; searching for facial, skeletal, somatic, and dermatoglyphic anomalies and asymmetries; visceromegaly; neurocutaneous lesions and depigmentations; and other signs of chronic illness. Hand preference and pencil grip are noted as well as any abnormal postures and involuntary movements. Clinical clues in the evaluation of developmental disorders are presented in Table 18.2.
behavioral phenotypes. The diagnostic yield is much greater if there is associated microcephaly, antenatal toxin exposure, or focal findings (19). In their absence, a thorough search for diagnostic clues includes family history with a three-generation pedigree and information from the prenatal, perinatal, and early postnatal periods. The development of motor skills; comprehension of speech; emergence of words and formed, intelligible sentences; and quality of social play skills are often relevant. The physical examination includes measuring head circumference as well as body size and growth; assessment of vision, hearing, and ocular funduscopy; searching for facial, skeletal, somatic, and dermatoglyphic anomalies and asymmetries; visceromegaly; neurocutaneous lesions and depigmentations; and other signs of chronic illness. Hand preference and pencil grip are noted as well as any abnormal postures and involuntary movements. Clinical clues in the evaluation of developmental disorders are presented in Table 18.2.
TABLE 18.2 Clinical Clues in the Determination of Developmental Disorders and their Etiology | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
The mental status examination assesses the child’s orientation, relatedness to, and interest in the examiner, caregiver, siblings, peers, and other people in the child’s environment; the quality of reciprocal social exchange in verbal and nonverbal communication (e.g., eye contact, gestures, facial expression), ability to engage in reciprocal imaginative play with representational toys; presence of perseverative, stereotypic, and ritualistic behavior; and presence of problematic behaviors such as attention difficulties, overactivity, aggression, and self-injury.
The laboratory evaluation of choice for developmental disorders continues to evolve as increasingly detailed understanding of the human genome leads to improved delineation of syndromes and advances in cytogenetic,
molecular, and neuroimaging techniques. Routine test batteries are not effective. The incidence of identifiable metabolic disorders in children with developmental delay is low, ranging from 0% to 5% (20,21). In addition, nonspecific, nondiagnostic, or false-positive “abnormalities” are common in routine nondirected laboratory testing. This can lead to further futile laboratory pursuits. Most infants and children with inborn errors of metabolism show signs or symptoms of their metabolic disorder such as hepatosplenomegaly, failure to thrive, intolerance of certain food groups, intermittent emesis, recurrent unexplained illnesses, seizures, intermittent somnolence, or fluctuating hypotonia. The relevant metabolic tests are reviewed in Chapter 1. In patients with developmental disorders who lack signs or symptoms of a metabolic disorder, metabolic screening should be deferred (22,23,24).
molecular, and neuroimaging techniques. Routine test batteries are not effective. The incidence of identifiable metabolic disorders in children with developmental delay is low, ranging from 0% to 5% (20,21). In addition, nonspecific, nondiagnostic, or false-positive “abnormalities” are common in routine nondirected laboratory testing. This can lead to further futile laboratory pursuits. Most infants and children with inborn errors of metabolism show signs or symptoms of their metabolic disorder such as hepatosplenomegaly, failure to thrive, intolerance of certain food groups, intermittent emesis, recurrent unexplained illnesses, seizures, intermittent somnolence, or fluctuating hypotonia. The relevant metabolic tests are reviewed in Chapter 1. In patients with developmental disorders who lack signs or symptoms of a metabolic disorder, metabolic screening should be deferred (22,23,24).
Many individuals with mental retardation have associated behavioral, emotional, and psychiatric disorders and nonneurologic congenital anomalies. A composite pattern recognition or cytogenetic testing may lead to a specific diagnosis (25). In these circumstances, the diagnostic label refers to the most salient aspect of the condition or is noted by an acronym, such as CHARGE association (of congenital anomalies) or eponym (e.g., Angelman syndrome), or by the underlying chromosomal abnormality, such as at chromosome 22q11.2. A specific molecular cytogenetic analysis, such as fluorescence in situ hybridization (FISH), may be indicated if the child has features of a known mental retardation syndrome (e.g., Williams or fragile X syndrome) or autism (e.g., chromosome 15q11 duplication) (see Chapter 4).
In most individuals with mild mental retardation, there are no specific neuropathologic correlates. Neuroimaging has a low diagnostic yield unless there are suspicious physical findings or localized neurologic deficits (26). Delayed myelination visualized on magnetic resonance imaging (MRI) is nonspecific in infants and children with neurodevelopmental delays (27). The diagnostic yield of neuroimaging increases considerably if the mental retardation is severe or complicated by microcephaly or macrocephaly, major motor abnormalities, features of a genetic syndrome, or seizures. MRI may reveal migrational disorders (e.g., lissencephaly), midline defects (e.g., holoprosencephaly or septo-optic dysplasia), or other brain malformations and disruptions (e.g., schizencephaly) (see Chapter 5). When the history suggests metabolic insult, vascular compromise, infection, or trauma, neuroimaging may reveal evidence of destructive central nervous system (CNS) changes.
There is no consensus on which children with developmental delay should be studied by imaging, and there are considerable variations in technique, methodology, demographics, and interpretation between the few available studies of computed tomography (CT) and MRI in children with mental retardation. Correspondingly, the reported frequency of abnormal neuroimaging findings in persons with mental retardation ranges from 9% to 80% (28,29,30,31). Positron emission tomography (PET), single photon emission CT (SPECT), functional MRI (fMRI) (32), and volumetric and morphometric MRI (33) provide insights into specific conditions but have limited overall application in the infant or child with a nonspecific developmental disorder. Formal audiologic testing is required to rule out hearing loss in all children who have language delay and may have isolated high-frequency hearing losses. Children with hearing impairment should be followed longitudinally for speech therapy and possible speech amplification.
Electroencephalography (EEG) is indicated if the history suggests seizures or regression or plateau in language acquisition (see Chapter 14). EEG can assist in the diagnosis of certain children with developmental disorders (34). Seizure disorders are often in their own right associated with diminishing IQ, as is their treatment with antiepileptic drugs (see Chapter 14). Memory may be deficient when the seizures are generalized. In complex partial seizure disorder, verbal and nonverbal memory may be impaired when there are left and right foci, respectively (35). Epileptic children as a group have inferior attention and general slowing of mental processes (36) as well as a varying degree of lag in language and reading ability (37). Children with frontal epileptic foci exhibited a relatively greater degree of impulsivity and disordered planning, verbal fluency, and motor coordination than generalized and temporal comparison groups (37). A comprehensive treatment of the neuropsychology of childhood epilepsy is available (38).
Habilitation and Rehabilitation
In habilitation, rehabilitation techniques are applied to individuals who, rather than having lost previously mastered skills, failed to master new skills at the expected age. This applies to children with developmental delay. For purposes of habilitation, the physician is less concerned about the level of function, and more with the implementation of evidence-based effective and enabling therapies, regardless of etiology. Schools are the primary venues of such therapies, and the consensus is swinging toward ever stricter demand for evidence-based justifications for such educational practices. For example, the Federal Department of Education maintains a “What Works Clearinghouse” that periodically reviews and reports educational efficacy evidence that meets high standards (39).
Children who are considered to have cognitive deficiency may come to attention because of poor academic achievement, abnormal behavior, or both. Is the lack of academic achievement due to limited cognitive ability, or does it represent underachievement relative to the child’s potential for other (e.g., psychosocial or emotional) reasons? If the child appears to be achieving at his or her
maximum level, consistent with that child’s specific profile of cognitive or attentional strengths or weaknessess, then special needs are identified, and an individualized educational plan (IEP) is implemented. If the child is underachieving, the causes are sometimes found in the child’s school and social setting or emotional well-being. In only a few developmental syndromes, notably attention-deficit hyperactivity disorder (ADHD), can cognitive potential be enhanced by medical means. In particular, there is as yet no evidence that learning disabilities, distinct from any comorbid attentional disorder, are pharmacologically treatable.
maximum level, consistent with that child’s specific profile of cognitive or attentional strengths or weaknessess, then special needs are identified, and an individualized educational plan (IEP) is implemented. If the child is underachieving, the causes are sometimes found in the child’s school and social setting or emotional well-being. In only a few developmental syndromes, notably attention-deficit hyperactivity disorder (ADHD), can cognitive potential be enhanced by medical means. In particular, there is as yet no evidence that learning disabilities, distinct from any comorbid attentional disorder, are pharmacologically treatable.
Most disorders of mental development are long lasting, if not permanent. Whether the child’s condition declares itself at or before birth or during early childhood, the parents have to adjust their previous expectations of a perfectly healthy child to the current reality. This adjustment is traumatic, and not all parents navigate its difficulties with success. The problem is amplified if, as is commonly the case, a specific diagnosis as well as a specific prognosis cannot be formulated. Such opinions as “developmental disability” convey confusion and are no substitute for the clarity and credibility of a specific diagnosis. When the disability is chronic and not fully explained—for instance, as in mental retardation and in autism—the quality of the parent–child relationship may suffer for lack of clarity about what to expect in the future. The clinician cannot always persuade the parents of what appears to be the reality of the situation, or even of the diagnosis, when that can be ascertained. Continued uncertainty is detrimental to parent–child attachment as well as to the functioning of the family unit. Under such circumstances, encouragement to seek a second opinion can with advantage be accompanied by referral for psychological counseling.
Inclusion in Public Education
The Education for All Handicapped Children Act (EHA) was renamed the Individuals with Disabilities Education Act (IDEA) in 1990. This legislation requires schools to provide an appropriate individualized educational plan to students with disabilities, to be implemented in the “least restrictive environment.” The IDEA mandates a nondiscriminatory assessment, active involvement of parents in the educational process with due-process rights and hearing, and access to indicated ancillary services such as physical therapy, counseling, and transportation. The reauthorization of IDEA requires that students with disabilities be educated with their nondisabled peers to the extent possible, and that schools actively plan for student transitions (and that traumatic brain injury and autism be considered separate categories). The word handicapped in the original version of the law was replaced with the word disabled. Inclusion refers to the effort to include students with disabilities in general classrooms while providing special services outside the general classroom as needed. Currently, approximately 70% of all students with disabilities attend mainstream classes during part of the school day.
Quantitative Measurement of Cognition (Standardized Scales)
In infancy and early childhood, receptive and expressive language and play skills are the best indices of cognitive level. The prognostic reliability of cognitive testing improves when children reach an age at which some language competence is expected and a wider range of testing modalities becomes available. Language development up to age 3 years can initially be documented in the clinical setting with the Early Language Milestone Scale (40). Early cognitive and language developmental milestones in infancy and childhood are summarized in Table 18.1.
The diagnosis of a cognitive deficiency requires that a clinical impression be validated by standard psychometric assessment or referral report. The assessment that is appropriate for infants and children with developmental delays or disabilities depends on the child’s age, level of impairment, and the presence of additional sensory deficits. For clinical screening up to age 6 years, the Denver-II, formerly the Denver Developmental Screening Test–Revised (41), has been commonly used. The Denver-II draws on parent history, testing, and observation and takes approximately one-half hour to administer. However, for predictive value, the Battelle Developmental Inventory Screening Test (BDIST), which screens children up to age 8 years, is preferred (42) though it is not designed to identify specific learning disabilities. A trained infant psychometrist is likely to adminster the Bayley Scales of Infant Development II, which estimate the level of cognitive and motor deficits in infants (43). However, because infant cognition is limited, only sensorimotor functions can be evaluated accurately for normative purposes. These functions are nonspecifically correlated to an infant’s later emerging cognitive skills, the lack of which may result in a developmental disability in later years. More specific information about selective deficits in cognitive operations can be gleaned from the results of neuropsychologic testing. A cognitive profile is established for diagnoses and functional evaluation, the monitoring of further development, and rehabilitation planning. Some commonly used measures of cognitive and adaptive behavioral development are summarized in Table 18.3.
Administered with proper reservation, an IQ test is by far the most valid means toward establishing a child’s level of functioning—knowledge that has wide clinical application. Regardless of disagreements as to whether IQ is a valid measure of intellectual or educational potential (58), the IQ test result is unequivocably the best guide in estimating overall current levels of functioning. IQ within the normal range by definition eliminates mental retardation
as the reason for preschool or school achievement below the expected level. It does not exclude the possibility that specific learning disabilities are compromising the acquisition of some academic skills. Therefore, IQ has been withdrawn from the necessary definition of learning disability in the 2004 IDEA. Furthermore, no single IQ test measures all cognitive operations, and various subtests involve multiple cognitive processes. Therefore, a low score on a subtest would be unlikely to isolate the basic cognitive deficit that prevents the child from learning to read, write, or calculate.
as the reason for preschool or school achievement below the expected level. It does not exclude the possibility that specific learning disabilities are compromising the acquisition of some academic skills. Therefore, IQ has been withdrawn from the necessary definition of learning disability in the 2004 IDEA. Furthermore, no single IQ test measures all cognitive operations, and various subtests involve multiple cognitive processes. Therefore, a low score on a subtest would be unlikely to isolate the basic cognitive deficit that prevents the child from learning to read, write, or calculate.
TABLE 18.3 Common Measures of Cognitive and Adaptive Behavioral Development in Infancy and Childhood | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Some “scatter” between the levels of subscale or subtest scores on an intelligence scale is normal. Only when it is statistically excessive might it reflect a disparity in the level of development of different intellectual skills. Verbal-performance discrepancy scores are often reported. Children with mild mental retardation tend to score somewhat lower on the Wechsler verbal subscale than on the performance subscale. A much lower verbal than performance IQ accompanies selective language delay; the converse discrepancy is often found in association with developmental difficulties in spatial orientation and visuomotor control, and to some extent in Asperger disorder.
The Stanford-Binet scale (46) and the Wechsler Preschool and Primary Scale of Intelligence (WPPSI) (44) are most commonly used for preschoolers. The Wechsler Intelligence Scale for Children (WISC-III) is available for school-aged children (45). These are well-standardized test batteries that call for the use of a range of different cognitive skills. For deaf children, the WISC-III performance scale and the Hiskey-Nebraska Test of Learning Aptitude have been specifically standardized (59). On such tests, deaf children without additional disabilities score close to the population average. The Perkins-Binet (60) and the Blind Learning Aptitude Test (61) are suitable for blind children. However, the most widely used psychometric instruments lack sensitivity in the mental retardation range. Even simple tests that use single words, such as the Peabody Picture Vocabulary Test (56), cannot be used if the patient is nonverbal. The Leiter International Performance Scale is useful for evaluating low functioning individuals (50). The interpretation of psychometric findings in mentally retarded subjects is complicated by uncertainties about the child’s test orientation and motivation. Because IQ levels in children younger than 3 years are unstable, the low-scoring child should receive a more definitive evaluation at a later date.
Considerations in the Assessment of Learning, Emotion, and Behavior
The developmental history and physical findings in early infancy are unreliable bases for prognosis as to developmental outcome. For example, Apgar scores of 0 to 3 at 15 and 20 minutes are predictive of high mortality and high probability of disability; however, many of these infants score normally in later developmental assessment (see Chapter 6). Intelligence tests in infancy yield a developmental quotient (DQ) that is necessarily heavily loaded with factors that relate to motor development. Within a normal population, the DQ is a poor predictor of individual differences in cognitive development. It has some success, however, in distinguishing a normally functioning from a mentally retarded population. Infant testing is highly specialized and also calls for the child’s cooperation. If this cannot be enlisted, the mother can be asked standard questions about her child’s social development (53).
Taken literally, the IQ scores can underestimate the child’s cognitive potential. Specific adaptive limitations often coexist with strengths in other adaptive skills or other personal capabilities. Limitations in adaptive skills may reflect the context of the child’s community. Motivation to perform during testing cannot be taken for granted, particularly when the child’s cultural or ethnic background has little understanding of and interest in cognitive testing and its uses. Anxiety can block the child’s reasoning processes, alienation and withdrawal can render the child unavailable for the task, thought disorders can intrude, and impulsive behavior can disrupt test performance. Lapses of attention owing to subclinical absence seizures can interrupt concentration, and psychotropic and antiepileptic medication may impair some cognitive processes. The limited attention span of patients with ADHD can degrade performance on tasks that demand sustained attention and cognitive effort. In young children, even gross impairment of vision, hearing, or touch can go unrecognized, and the child’s imperfect response to instruction or questions can be misattributed to defiance or cognitive deficiency. Other factors that complicate the interpretation of mental test performance are extremely low or high parental educational level, poor motivation with failure to expend mental effort on the test, depression, fatigue, and fear of failure with low self-esteem. Such potential sources of misinterpretation, which almost always lead to underestimation rather than overestimation, can never be fully ruled out, but conventional best practices expect the psychologist’s report, usually in writing, to provide an estimate of the reliability of the reported score, taking such factors into consideration.
MENTAL RETARDATION
Terminology and Definitions
The terminology that is used to characterize persons with cognitive and adaptive behavioral disabilities has evolved, in repeated efforts to minimize social stigma. Terms such
as cognitive deficiency, intellectual disability, and learning disability have been suggested to replace mental retardation, a term that misleadingly implies delay and therefore the possibility that the child will catch up. A similar term is developmental delay, which is nonspecific and is more of a chief complaint or a symptom complex than a diagnosis (62). Whereas children with mental retardation may learn new skills as they mature and are taught, most functional neurologic impairments are associated with intractable deficits of intellectual capacity. Mental retardation is a compendium term that does not refer to particular groups of diseases, syndromes, or medical disorders. It is not applied to cognitive deficiency that is a result of neurodegenerative and progressive neurometabolic diseases, or is secondary to psychiatric disorders.
as cognitive deficiency, intellectual disability, and learning disability have been suggested to replace mental retardation, a term that misleadingly implies delay and therefore the possibility that the child will catch up. A similar term is developmental delay, which is nonspecific and is more of a chief complaint or a symptom complex than a diagnosis (62). Whereas children with mental retardation may learn new skills as they mature and are taught, most functional neurologic impairments are associated with intractable deficits of intellectual capacity. Mental retardation is a compendium term that does not refer to particular groups of diseases, syndromes, or medical disorders. It is not applied to cognitive deficiency that is a result of neurodegenerative and progressive neurometabolic diseases, or is secondary to psychiatric disorders.
The World Health Organization (ICD-10) characterizes developmental disabilities as due to impairment of the central nervous system, causing a functional disability, which consequently handicaps the individual in activities of daily living (63). It characterizes mental retardation as “incomplete or insufficient general development of mental capacities.” Formal definitions of mental retardation that are currently recognized emphasize a descriptive diagnosis of persons with significant disability because of “subaverage intellectual functioning” and “concurrent deficits or impairments in present adaptive functioning [i.e., how effective persons are in meeting the standards expected for their age by their cultural group]” (64,65). In addition, the manifestation of brain dysfunction must originate during the developmental period of life. The three formal definitions differ slightly in their approach to the diagnosis because of differences in emphasis on adaptive skill symptom menus or underlying etiologic factors.
TABLE 18.4 Classification of Mental Retardation by Measure of IQ and Level of Adaptive Behavior | |||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||
Because mental abilities are on a continuum, the quantitative definitions of mental retardation and its subdivisions based on the IQ are necessarily arbitrary cut-off points. The mental age (the age equivalent at which the child functions on the test) divided by the chronologic age is the IQ. The mean I.Q. for the general population is set at 100. Higher IQ predicts more academic success in such terms as higher grades, more years completed, and higher standardized test scores. It also predicts positive life outcomes, such as better mental health, lower divorce rate, lower level of criminality, and greater occupational success (66,67).
The standard deviation (SD) of a test refers to the distribution of scores around the mean. Mild, moderate, severe, and profound mental retardation have been traditionally associated with cutoff points in standard deviations below the mean of –2, –3, –4, and –5, respectively (68) (roughly corresponding to IQs of 70, 55, 40, and 25). IQ scores between 70 and 85 are sometimes referred to as borderline. But measured intelligence does not offer specific information about the individual’s adaptive skills (Table 18.4). There is ongoing controversy on whether to emphasize IQ level or adaptive behavioral deficits as the central defining characteristic of mental retardation (69). The extent to which persons with mental retardation succeed in life is determined by their level of adaptive skills rather than by their IQ. However, there is no single measure of
adaptive behavior. Newer efforts to define mental retardation have emphasized the amount of support needed for an individual to succeed or maintain basic activities of daily living, instead of focusing on global degrees of impairment (70). Support intensities are subdivided into four levels: intermittent, limited, extensive, and pervasive. Support functions are classified into eight categories: teaching, befriending, financial planning, behavioral support, in-home living assistance, community and school access and use, and health assistance. This categorization acknowledges that the diagnosis of mental retardation is useful only as a pointer toward providing the individual with additional supports for activities of everyday living beyond those that are considered to be customary for the child’s age.
adaptive behavior. Newer efforts to define mental retardation have emphasized the amount of support needed for an individual to succeed or maintain basic activities of daily living, instead of focusing on global degrees of impairment (70). Support intensities are subdivided into four levels: intermittent, limited, extensive, and pervasive. Support functions are classified into eight categories: teaching, befriending, financial planning, behavioral support, in-home living assistance, community and school access and use, and health assistance. This categorization acknowledges that the diagnosis of mental retardation is useful only as a pointer toward providing the individual with additional supports for activities of everyday living beyond those that are considered to be customary for the child’s age.
Further insight into the child’ strengths and weaknesses is afforded by neuropsychological testing, which attempts to tease out of the cognitive spectrum different domains of functioning that can be differentially affected by brain damage, depending on which areas have borne the brunt of the insult. These techniques are most frequently used with normal functioning children who have school problems but also can be applied to mildly mentally retarded children. The resulting information may be helpful with respect to diagnosis, prognosis, and educational and vocational planning (e.g., 71). IQ labeling should not replace repeated educational and achievement assessments. Not only is the IQ score unreliable below age 3 years, but also deficits in visual, spatial, and motor function, as well as expressive language, may influence early testing. Underprivileged and understimulated children may perform poorly on language-based tests for reasons that are sociocultural rather than neurobiological. Such a child’s level of functioning is better reflected in the results of nonverbal testing, as on the Culture-Fair Intelligence Test, Scale 2 (72), Raven’s Progressive Matrices (73), and the Universal Nonverbal Intelligence Test (74). The interpretation of IQ test results should take into account cultural and linguistic diversity, differences in communication ability, and attentional and behavioral factors.
Behavioral Phenotypes of Mental Retardation Syndromes
A syndrome is a recognizable and consistent pattern of multiple manifestations that are known to have a specific etiology (75). More than 1,000 defined syndromes involve multiple congenital abnormalities (76). Most feature some pattern of impaired mental development. The degree of mental retardation is quite variable in most of these syndromes and is not indicated by the severity of neurobiologic concomitants, such as degree of abnormality of brain structure as visualized on MRI. Also, the deficit is often compounded by social factors. Dysmorphic facial features may give a misleading impression of low intelligence, and severe neurologic handicap may limit the children’s ability to express their intellect. Striking instances are athetosis and Lesch-Nyhan syndrome. Teachers may underestimate the child’s learning potential and offer a restricted number of learning opportunities. Nonetheless, some syndromes are characterized by specific behavioral phenotypes—of cognition, personality, and psychopathology—over and above the generally diminished level of functioning and any negative effects of the child’s environment.
Behavioral phenotypes have been characterized as follows, “a number of conditions, recognizable by a common physical phenotype, single gene defect or chromosomal abnormality, seem also to have a constellation of behaviors or cognitive anomalies which are characteristic” (77). Although mentally retarded children are by definition impaired in all or most cognitive domains, certain mental retardation syndromes present striking cognitive and behavioral dissociations. Selective neuropsychological deficits can occur against a background of generally deficient intellect as well as in otherwise normally functioning children. The adverse influence, whether genetic or due to intercurrent insults, is widespread, but lowering the level of intelligence below normative expectations, is not homogeneous, perhaps reflecting unequal impact on areas of the brain that differ in functional specialization. Examples of dissociations follow.
Mentally retarded children with autism are disproportionately handicapped in the language and social domains, domains that are relatively spared in children with Williams syndrome (78 and see Chapter 4). Children with Williams syndrome speak with appropriate phonology and syntax, although their comprehension and pragmatics are weak (see Chapter 4). However, they are especially deficient in visual-spatial construction and number sense. Conversely, visuospatial skills are a strong point for children with Prader-Willi syndrome, who display a specific flair for jigsaw puzzles (79). Down syndrome children are particularly impaired in receptive and still more in expressive language, long-term memory (80,81), and gross and especially fine motor skills (82). Particularly with respect to language, these impairments become more obvious after the initial relatively rapid development of the first three years has decelerated. Some Down children become autistic, especially if there is an autistic spectrum disorder family history (83). Girls with Down syndrome as a group consistently perform better than boys (84). Children with hydrocephalus tend to be disproportionately strong in speech production, producing rapid uninformative “cocktail chatter,” though not in speech comprehension and pragmatics. They are weak in face recognition and social cognition (85). Among X-linked chromosomal aberrations, fragile X syndrome (85a) is particularly handicapping in language development and social skills (86). Speech development is delayed, perseverative, and echolalic, and the children are
shy, anxious, and show many autistic features. There is fine and gross motor delay. The language and social domains also are problematic for children with XXX (87), whereas Turner syndrome (XO) is associated with visuospatial, arithmetic, and memory deficits (88) as well as deficient recognition of faces and facial expressions (89), while language is intact. XYY syndrome is characterized behaviorally by language disability, lack of sociability and aggressiveness, and Klinefelter syndrome (XXY) boys tend to exhibit low verbal abilities, clumsiness, and introversion (90). In Cornelia de Lange syndrome, nonverbal abilities may be selectively impaired (91). Untreated, phenylketonuria results in severe mental retardation. Even when effectively treated, children with phenylketonuria exhibit impaired performance on executive function tests (92), apparently implicating dopaminergic projections to dorsolateral prefrontal cortex (93). The characterization of the selective deficit as involving executive functions is disputed, however (94). Untreated children with congenital hypothyroidism are severely mentally retarded. After early treatment, deficits are confined to the domains of visuospatial skills, attention, and fine motor control (95). In galactosemia, language and executive impairments as well as fine motor deficits have been reported. Some of the children are mentally retarded (96).
shy, anxious, and show many autistic features. There is fine and gross motor delay. The language and social domains also are problematic for children with XXX (87), whereas Turner syndrome (XO) is associated with visuospatial, arithmetic, and memory deficits (88) as well as deficient recognition of faces and facial expressions (89), while language is intact. XYY syndrome is characterized behaviorally by language disability, lack of sociability and aggressiveness, and Klinefelter syndrome (XXY) boys tend to exhibit low verbal abilities, clumsiness, and introversion (90). In Cornelia de Lange syndrome, nonverbal abilities may be selectively impaired (91). Untreated, phenylketonuria results in severe mental retardation. Even when effectively treated, children with phenylketonuria exhibit impaired performance on executive function tests (92), apparently implicating dopaminergic projections to dorsolateral prefrontal cortex (93). The characterization of the selective deficit as involving executive functions is disputed, however (94). Untreated children with congenital hypothyroidism are severely mentally retarded. After early treatment, deficits are confined to the domains of visuospatial skills, attention, and fine motor control (95). In galactosemia, language and executive impairments as well as fine motor deficits have been reported. Some of the children are mentally retarded (96).
It is apparent from the highly diverse listing presented above that deficits in cases of atypical development are not interpretable in terms of selective loss with respect to a single behavioral module or a single functional domain. Rather, there is a suite of more impaired domains, and a suite of better functioning domains, in every type of affected child. The cognitive phenotypes associated with a specific genetic abnormality also can be quite diverse, as for instance in Williams syndrome (97). Therefore, the phenotypes even of genetically determined syndromes appear to be multiply determined, with some effect of environment, in the broad sense that encompasses both prenatal and postnatal factors, interacting with the genetically determined susceptibility. Notably, language ability does not fall out or remain intact in one piece (98). The classical dispute about whether language skill is modular and unique among cognitive skills (99) is not resolved by the study of atypical development.
TABLE 18.5 Examples of Genetic Syndromes with Characteristic Behavioral Phenotypes | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Comorbid Psychiatric Disorders in Persons with Mental Retardation (Dual Diagnosis)
Persons with mental retardation are at increased risk for psychiatric disorders. Whereas the incidence of psychiatric disorders in the general childhood population is 7% to 10% (100), approximately one-third of all children with developmental disorders also have psychiatric disorders (100,101,102,103). In the severely retarded subpopulation, the frequency of psychiatric disorders is much higher and approaches two-thirds by adolescence (104). The broad spectrum of psychopathology includes affective disorders (105), anxiety disorders, autisticlike behaviors (106), conduct disorders (107), maladaptive behaviors (repetitive self-stimulation, self-injurious behavior, pica) (108,109), and psychosis. These emotional and behavioral disturbances are caused by multiple factors, both primary psychopathologies and neuropsychologic disorders and the secondary effects of illness, dependency, environmental deprivation, frustration, and low self-esteem (110).
The behavioral phenotypes of certain genetic syndromes are associated with typical personality characteristics and reproducible behavioral mannerisms (Table 18.5). Though otherwise often of even temperament, Down syndrome children may be irritable and inattentive because they are prone to obstructive sleep apnea (120), which in turn is a separate risk factor for neurocognitive (especially right hemisphere) deficits (121) and for depression (122). Specific personality differences also may occur in mental retardation syndromes, such as unusual sociability and distractibility in Williams syndrome and compulsivity, excessive talkativeness, impulsivity, and low activity level as well as compulsive eating and foraging for food in Prader-Willi syndrome (79).
Children with velocardiofacial syndrome have on average a borderline IQ, concrete thinking, bland affect, and little social interaction. They are highly susceptible to
psychiatric disorders, particularly schizophrenia, with which they may have a frequently occurring deletion on chromosome 22 in common (123). Twenty-five percent of children with velocardiofacial syndrome present with schizophrenia by early adulthood. A higher proportion still presents with ADHD in childhood and responds favorably to stimulant therapy (124). Girls with Turner syndrome tend to be unassertive and compliant and maintain poor and sparse social relationships (125). Children with Lesch-Nyhan syndrome have a unique form of compulsive behavior, which is expressed by an apparently involuntary drive toward self-injury and aggression. The children apologize and ask to be restrained in the act of attacking others or themselves (126). Abnormal dopamine functioning during early development may be implicated (126).
psychiatric disorders, particularly schizophrenia, with which they may have a frequently occurring deletion on chromosome 22 in common (123). Twenty-five percent of children with velocardiofacial syndrome present with schizophrenia by early adulthood. A higher proportion still presents with ADHD in childhood and responds favorably to stimulant therapy (124). Girls with Turner syndrome tend to be unassertive and compliant and maintain poor and sparse social relationships (125). Children with Lesch-Nyhan syndrome have a unique form of compulsive behavior, which is expressed by an apparently involuntary drive toward self-injury and aggression. The children apologize and ask to be restrained in the act of attacking others or themselves (126). Abnormal dopamine functioning during early development may be implicated (126).
Epidemiology and Prevalence
Since the frequency with which a disorder arises in a population during a stated period of time is its incidence, and since its prevalence describes the amount within a population at a given time, the prevalence of the condition is the product of its incidence and its duration. The prevalence of a developmental disorder, therefore, may change over the years because of prenatal diagnosis and more frequent termination of pregnancy, changes in the maternal population, and changes in health care. For example, the prevalence of Down syndrome increased from the 1920s through the 1960s, as persons with this condition began to live much longer because of improvements in medical care. However, since 1980, further increases have been slight (127,128).
The prevalence of mental retardation is 6 to 20 per 1,000 (129,130,131,132). The published estimates vary on account of regional differences, ascertainment biases, and variations in diagnostic criteria and study methodology. Mild mental retardation is 10 to 12 times more common than severe retardation. Mental retardation is more common among males because of X-linked syndromes involving mental retardation, especially fragile X syndrome. The male to female ratio ranges from 1.3:1 to 1.9:1 (133). Morbidity and mortality are greater in persons with severe mental retardation, not due to the mental retardation itself, but because of the severe cerebral palsy that is often associated with it. Total immobility and feeding by nasogastric tube are the features that are most predictive of curtailed life span (134,135).
Causes of Mental Retardation
Timing
Mental retardation can be caused by genetic, environmental, and ecogenetic factors. A specific diagnosis can be determined in most children with global developmental delay [see (136) for recommendations as to which tests should routinely be used]. The diagnostic process is aided considerably if one can determine when the developmental insult occurred. Prenatal causes of mental retardation, with genetic etiologies as the major subset, account for approximately 60% to 80% of all developmental disorders. Perinatal causes include asphyxia and birth trauma. Mental retardation secondary to perinatal causes is almost invariably accompanied by cerebral palsy and/or epilepsy and probably accounts for at least 8% to 12% of all cases (137). Postnatal causes, including meningitis, encephalitis, trauma, and malnutrition, may account for up to 10% of cases. Some individuals may have more than one etiologic cause of their developmental disability, and the interacting causes may have occurred at different periods of development. For example, a fetus with hypotonia secondary to genetic causes is predisposed to perinatal injury (138,139,140). When individuals thought to have perinatal causes of their disabilities are later found to have a genetic etiology, the latter causation is likely to have been interactive with the perinatal stressors (141).
Severity
The more severe the mental retardation, the more likely it is that a specific etiologic diagnosis can be made [and the more likely the child is to be nonrighthanded (142)]. An identifiable cause is found in 70% to 80% of severe cases but in less than 50% of individuals with mild mental retardation. By neuroimaging or at autopsy, the brains of most severely mentally retarded individuals are found to be grossly abnormal. Mild mental retardation for which no specific cause can be uncovered is usually ascribed to polygenic inheritance. Subnormal head circumference may be the only abnormal physical sign in mentally retarded children. In a review of referrals to a child development center, some 15% of children were microcephalic. One-half of these children were mentally retarded. Prematurity, perinatal asphyxia, intrauterine growth retardation, respiratory distress syndrome, and intracerebral hemorrhage were associates of microcephaly (143) (see Chapter 5).
Diagnostic Categories
Chromosomal and Genetic
Chromosomal aberrations have been reported in 4% to 28% of persons with moderate to severe mental retardation, craniofacial differences, and other congenital anomalies (Table 18.6;143, 144, 145, 146, 147, 148). The percentage of clinically relevant chromosomal abnormalities varies between studies because of differences in definitions, methodology, ascertainment (population-based versus institutional), and type of cytogenetic study. Down syndrome is by far the most common chromosomal disorder and accounts
for 4% to 7% of all cases of mental retardation (148,149). The fragile X syndrome (FXS) is considered in Chapter 4. In FXS, developmental testing reveals delays by 9 to 12 months of age (150). Cognitive deficits are milder in females than in males and often implicate math learning disability and frontal lobe–related deficits. Chromosomal disorders, including the contiguous gene syndromes, are considered in Chapter 4.
for 4% to 7% of all cases of mental retardation (148,149). The fragile X syndrome (FXS) is considered in Chapter 4. In FXS, developmental testing reveals delays by 9 to 12 months of age (150). Cognitive deficits are milder in females than in males and often implicate math learning disability and frontal lobe–related deficits. Chromosomal disorders, including the contiguous gene syndromes, are considered in Chapter 4.
TABLE 18.6 Cause of Mental Retardation by Diagnostic Category | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||
Primary malformations of the CNS result from multiple genetic and ecogenetic causes (see Chapter 5). Numerous major and minor developmental malformations result from disturbances in neuronal proliferation, migration, differentiation, axonal outgrowth, synapse formation, dendritic arborization, and process elimination, depending on the genetic condition or severity and timing of an environmental insult. In the prenatal period, it is often impossible to distinguish the extent to which an environmental insult causes vascular or parenchymal injury or disrupts gene and signaling molecule expression.
Prematurity and Cerebral Palsy
Technologic advances in neonatology have transformed survival rates and morbidity patterns. Outcomes differ notably between very-low-birth-weight infants (less than 1,500 g) and extremely low-birth-weight infants (less than 1,000 g). Outcomes in premature infants range from normal functioning to severe disability (151), lasting at least into the teenage years in the form of academic deficits (152). Cognitive deficits occur even if the neonatal course was uncomplicated. Difficulties in spatial memory, sustained attention, and visuospatial function were documented at 4 years of age in otherwise normal preterm children (153). A wide range of cognitive deficits as well as elevated scores on an ADHD rating scale were found in children aged 7 years who were born before 32 weeks of gestation and were being educated in mainstream schools (154). Very-low-birth-weight children do even worse if they also had bronchopulmonary dysplasia (BPD). At age 8 years, the presence of BPD and/or relatively long duration on oxygen were found to have predicted lower performance IQ, impaired perceptual organization, and motor and attentional skills as well as lower educational achievement, with more frequent special education placement (155). Twenty percent of BPD children had IQs below 70, in the mental retardation range, as compared with 11% of very-low-birth-weight children without BPD and 3% of term controls. However, even mild indications of risk for birth anoxia had significantly adverse effects on cognitive outcome (156). This result supports the view that the deficits following asphyxia at birth are a matter of degree, in proportion to the severity of the injury—“there is a continuum of brain injury in asphyxia” (157)—rather than supporting an all-or-none “threshold” model (158). Correspondingly, selective neuronal necrosis in asphyxiated sheep brain was directly proportional in its severity and extent to the duration/ischemic of the inflicted insult (159). Another recent study also found a continuum, such that the neuropsychologic outcome was inversely related to the birth weight among children born weighing less than 1,500 g (160). Verbal functions were relatively spared, whereas spatial recognition, working memory and attention shifting were most affected.
Bradycardia and apnea are postnatal causes of hypoxia. In one study, 256 preterm and term infants were monitored at home and then tested on an index of mental development 96 weeks after conception. Infants who had five or more episodes of apnea and/or bradycardia performed significantly worse than infants who did not meet that criterion (161). Furthermore, 5-year-old children with sleep-disordered breathing scored less well than controls on tests of overall intellectual ability as well as on attention, memory, and planning (162).
Nearly one-half of a group of premature children had ocular pathology associated with impaired acuity, stereopsis, contrast sensitivity, and color vision (163). Cognitive deficits may be associated with regional brain volume reductions revealed by neuroimaging. Episodic memory deficits were associated with diminution in hippocampal volume in otherwise normal very-low-birth-weight children (164). MRI studies of adolescents who were born after a gestation of 33 weeks or less reveal decreased brain volume and enlarged lateral ventricles (165). In premature infants scanned near term, regional volume reductions were documented. White matter volumes in the sensorimotor and midtemporal regions correlated strongly with neurodevelopmental outcome (166). Neurological complications of prematurity are reviewed in Chapter 6.
Those premature and term children who sustain damage that results in cerebral palsy frequently bear the additional burden of associated deficits in vision, hearing and the ability to learn. Independent of the frequently present mental retardation, children with bilateral spastic
cerebral palsy were found to have selective difficulty on tasks that call for inhibitory control, and presumably rely on intact prefrontal function (167). More generally, cerebral palsied children have up to a 40% chance of learning disability or mental retardation. Most of this is accounted for by children with spastic quadriplegia. In hemiplegic cerebral palsy, early damage to either side has relatively more detrimental cognitive effects if it is complicated by seizure activity. The more severe deficits that accompany the seizure disorder group do not bear the usual qualitative relationship to the side of the lesion (168). Stroke before age 1 year has similar but greater effects on cognition than in adults (), calling into question the notion that children escape from the consequences of brain injury if it occurs very early (169). Both cerebral palsy (170) and childhood stroke (171) feature ADHD phenotypes among their sequelae. Methylphenidate is effective in treating the ADHD phenotype associated with cerebral palsy (172).
cerebral palsy were found to have selective difficulty on tasks that call for inhibitory control, and presumably rely on intact prefrontal function (167). More generally, cerebral palsied children have up to a 40% chance of learning disability or mental retardation. Most of this is accounted for by children with spastic quadriplegia. In hemiplegic cerebral palsy, early damage to either side has relatively more detrimental cognitive effects if it is complicated by seizure activity. The more severe deficits that accompany the seizure disorder group do not bear the usual qualitative relationship to the side of the lesion (168). Stroke before age 1 year has similar but greater effects on cognition than in adults (), calling into question the notion that children escape from the consequences of brain injury if it occurs very early (169). Both cerebral palsy (170) and childhood stroke (171) feature ADHD phenotypes among their sequelae. Methylphenidate is effective in treating the ADHD phenotype associated with cerebral palsy (172).
Toxins and Radiation
The long-term effects of exposure to alcohol, marijuana, cigarettes, cocaine, and other street drugs on cognition and behavior are difficult to determine separately because polydrug use is the rule. Also, the frequency, quantity, type of substance, and timing of exposure during pregnancy vary greatly. Moreover, drug habits are frequently associated with poor nutrition and lack of prenatal care. However, there are clear associations between maternal alcohol abuse and adverse effects on early brain development. Fetal alcohol syndrome (FAS) may be the most common among the identified causes of mental retardation in North America and Europe. Children with facial features of FAS and a history of maternal alcoholism during pregnancy have been described as inattentive and hyperactive, with disordered conduct and defective memory (173). Whether prenatal cocaine exposure has any adverse effect on long-term cognitive outcome is questionable (174). Any low functioning is more likely to be due to adverse conditions in the postnatal caretaking environment (175). Some children with fetal valproic acid syndrome have been reported to be autistic (176). Fetal alcohol syndrome and the effects of cocaine and opiates are discussed in Chapter 10.
Acute severe lead poisoning may cause mental retardation as a sequelae of an acute encephalopathy. Chronic subclinical lead poisoning is associated with an increased risk of antisocial and delinquent behavior as well as disorders of cognition and learning (177), but these outcomes are confounded by the effects of low socioeconomic status and stimulation level in the home environment (178) (see Chapter 10). The HOME questionnaire measures the stimulation a child receives at home. This type of variable is a crucial covariate in any population study on cognitive effects of potential toxins. When relevant covariates were held constant in a meta-analysis, the apparent detrimental effects of subclinical lead dwindled into insignificance (179). Maximum controversy centers on the clinical significance of the 10 to 19 ug/dL blood lead dose level, the Centers for Disease Control’s (CDC) lowest “level of concern” (180,181). An attempt to show that lead levels below 10 ug/dL cause deficits in cognitive and academic skills (182,183) is controversial (184) and suffers from methodological shortcomings (185). The neurobiology of lead poisoning is discussed in Chapter 10.
Mercury nitrate is the toxin that caused “Mad Hatter’s” disease (186). Children who were given a “teething” powder that contained mercury fell victim to acrodynia (pink disease), which in addition to physical signs caused severe irritability, anorexia, photophobia, and sleeplessness (187). A comprehensive resource for information about the toxic effects of methylmercury is available (188). Widely differing sensitivities to comparable levels of exposure draw attention to host factors in clinical susceptibility to mercury poisoning. Mercury is found in dangerous amounts in fish in certain geographic locations. When consumed in large amounts by pregnant women, it has led to cerebral palsy and mental retardation in their children (189). Symptoms of less severe exposure included muscle stiffness, dysesthesia, hand tremor, dizziness, loss of pain sensation, muscle cramps, arthralgia, chest pain, palpitations, fatigue, visual dimness, and staggering (190). Muscular atrophy was observed. Methylmercury is taken up by multiple organs. In the brain, it is gradually broken down to metallic mercury, which cannot be cleared. Over time, cerebral atrophy results. Other sources of intense mercury poisoning include skin whiteners and processing of mined gold. The recently withdrawn ethylmercury-containing vaccine preservative thimerosal was administered by routine vaccination (DPT, Hepatitis B, HiB) to infants in cumulative amounts well above the Environmental Protection Agency’s (EPA) maximum sanctioned (benchmark) dose. Low-level prenatal exposure to methylmercury from maternal consumption of seafood poses a less severe but still increased neurodevelopmental risk (191,192,193). Neuropsychologic testing has implicated language, reading, attention, memory, and visuomotor function (194). The younger the child, the greater the risk. Susceptibility to low-grade poisoning also varies tremendously between individuals due to as yet unidentified host factors. Signs of mercury poisoning may present, weeks, months, or even years after exposure (195).
Prenatal polychlorinated biphenyls (PCB) and dioxin exposure have an apparent detrimental effect on children’s mental development, which for reasons that are not clear spared children who were raised in optimal environments or breast-fed (196,197). Organophosphate pesticides also are under suspicion (198).
Pelvic nuclear (199) and x-irradiation (200) can lead to mental retardation of offspring, especially if applied between the seventh and fifteenth weeks of gestation. The
degree of mental retardation is proportional to the amount of irradiation. The incidence of Down syndrome and other chromosomal abnormalities is greater among offspring of those women in their late reproductive years who were irradiated during pregnancy (201).
degree of mental retardation is proportional to the amount of irradiation. The incidence of Down syndrome and other chromosomal abnormalities is greater among offspring of those women in their late reproductive years who were irradiated during pregnancy (201).
Poverty and Other Familial Factors
There is a complex relationship between genetics, nutrition, social environment, and learning (202). The adverse effects of psychosocial deprivation on socialization and motivation may impair performance even if the child has normal cognitive abilities. One American child in five lives in a family with income below the poverty threshold (203). The risk of mental retardation and inferior academic performance increases with decreasing socioeconomic status (204,205,206). However, on a population basis, the factors that mediate the effects of poverty on child health and development are uncertain (207). Parental nurturing, sociocultural influences, and educational environments are determinants of developmental outcome and ultimate adaptation to society (208). Less positive parenting contributes to adverse outcomes (208a). Some children are resilient and function better than one would expect based on their socioeconomic status. Resilience is partly heritable and partly mediated by maternal warmth and stimulating activities (209). In contrast, infants and children who are deprived of maternal attention and are institutionalized in a hospital or an orphanage often become depressed, and their cognitive skills decline or fail to advance (210,211,212). Children adopted from Romanian orphanages exhibited anomalies of attachment and personality (213). A positron emission tomography study of such adoptees revealed reduced brain activation in orbitofrontal, inferolimbic, and medial temporal cortex, including amygdala, structures involved both in cognition and emotion regulation (214). EEGs of Romanian adoptees showed diminished power in high frequency bands at frontal and temporal electrode sites and increased power in low-frequency bands posteriorly (215). These EEG abnormalities indicate cortical hypoarousal and/or delayed cerebral maturation. Adverse cognitive and academic consequences are to be expected in such children, but the outcome is never certain, let alone irremediable, in the individual case.
Hormones and Infections
Maternal hypothyroidism results in lowered IQ of the offspring (216). Congenital hypothyroidism causes mental retardation only in children who are left untreated after birth. Insulin-dependent diabetes mellitus is associated with declining verbal test scores (217). The neurologic complications of thyroid deficiency and diabetes are presented in Chapter 17. Nutritional disorders are discussed in Chapter 10.
CNS infection early in life is a major cause of mental retardation, especially in developing countries. Prenatal infections such as toxoplasmosis, syphilis, rubella, cytomegalovirus, herpes, and varicella are associated with microcephaly, intracranial calcifications, cataracts, growth retardation, sensorineural hearing loss, and seizures. Such infections may cause mild, moderate, or severe mental retardation. Bacterial, viral, and fungal meningitis and encephalitis—in particular, neonatal and childhood herpes simplex encephalitis—are perinatal and postnatal causes of mental retardation (see Chapter 7). Hookworm infection can contribute to iron deficiency, which is associated with decreased cognitive abilities (218) whether anemia is present or not (219).
Management
Medical
Stimulant medications, such as methylphenidate, may be beneficial for some mildly mentally retarded children who are hyperactive (220). Numerous other older and newer medications have been used with variable success to ameliorate adverse behaviors such as aggression, self-injury, and severe hyperactivity in persons with mental retardation. Neuroleptics, such as thioridazine in low doses, may have a calming effect in some children and when given at bedtime may assist sleep. Carbamazepine and propranolol can be beneficial for rage and episodic loss of control. Antidepressants, such as clomipramine and fluvoxamine, are often helpful in decreasing compulsive behaviors and stereotypies. Opioid antagonists, such as naltrexone, are occasionally successful in decreasing self-injurious behaviors (221,222). On withdrawal, some medications can give rise to tardive dyskinesias because of dopamine hypersensitivity (223). This tendency can be counteracted by GABAergic antiepileptic agents (224). Pharmacologic treatment of behavioral disorders in children with mental retardation should be coordinated with behavioral modification programs.
Nonmedical
Management includes family support and education, and the provision of early intervention and special education programs. There are no specific methods for improving the overall intelligence of most mentally retarded people, although improvement in some skill deficiencies is a feasible educational goal. There is disagreement about how the largest group, the mildly mentally retarded, should be taught, and even about whether that should be any different from how learning disabled children are taught. The efficacy of early intervention programs in enhancing mental development has not been validated (225). The primary goals are to provide a “least restricted environment,” a placement that safeguards the child and at the
same time permits the child to function at maximum potential. The child’s temperament and level of socialization are important modifying factors that can differ widely among individuals at a given IQ level. A regular preschool with language therapy may be appropriate for mildly disabled preschool children with adequate comprehension and without behavioral problems. For children whose attention and concentration are limited, special education teachers use attention-focusing techniques to optimize learning. Best results are obtained in structured rather than flexible settings because individuals with mental retardation are usually deficient in judgment and problem-solving strategies. A child with mild mental retardation who is taught at an appropriate rate in suitably structured settings can become self-reliant in a considerable variety of work competencies, not strictly limited to manual and domestic occupations or routine industrial tasks such as assembly and production-line operations.
same time permits the child to function at maximum potential. The child’s temperament and level of socialization are important modifying factors that can differ widely among individuals at a given IQ level. A regular preschool with language therapy may be appropriate for mildly disabled preschool children with adequate comprehension and without behavioral problems. For children whose attention and concentration are limited, special education teachers use attention-focusing techniques to optimize learning. Best results are obtained in structured rather than flexible settings because individuals with mental retardation are usually deficient in judgment and problem-solving strategies. A child with mild mental retardation who is taught at an appropriate rate in suitably structured settings can become self-reliant in a considerable variety of work competencies, not strictly limited to manual and domestic occupations or routine industrial tasks such as assembly and production-line operations.
Children with mental retardation who in addition have significant language and social dysfunction often do not succeed in the typical classroom settings that are appropriate for students with specific learning disabilities. Self-contained classrooms usually provide a better environment for children with severe mental retardation and severe communication disorders or autistic behaviors. These classrooms ideally have a low teacher to student ratio with special education teachers who are familiar with interventions for students with nonverbal learning disabilities and social communication deficits. Some children with severe mental retardation require placements that offer behavioral modification programs and school time geared toward life skills such as basic hygiene and self-care. Public laws mandate that individual educational programs (IEP) be regularly reassessed.
Management involves many nonmedical disciplines. Caregivers may need to be trained in how to handle, feed, and toilet their child. Effective case management comprises health care planning that includes comprehensive diagnostic evaluation, an assessment of disabilities, and individualized treatment plans for educational, behavioral, pharmacologic, and medical interventions.
Declining Intellectual Function in Adolescence or Preadolescence
Infrequently, children are referred by psychologists, social workers, educators, or rarely, parents, based on the impression—with or without psychometric documentation—of declining intellect or IQ. Test-retest reliabilities on IQ tests are well established, and the findings must be taken seriously, especially when the psychologist’s report rules out the usual motivational or sociocultural reasons for an occasional aberrantly low score. A progressive neurological disorder also must be ruled out. More commonly, drug abuse is responsible and should be investigated by serum drug screening, cocaine being the substance of greatest interest. Alternatively, prodromal changes heralding schizophrenia should be considered. By standard definition, schizophrenia involves declining function over a 6-month period, and declining IQ may be a warning sign. Particularly for a child with a history of schizophrenia spectrum disorder in the extended family, the appropriate syndromally based diagnostic interview is called for (over and beyond any global impression or score on a single scale). An outcome that falls short of being diagnostic of schizophrenia may still offer warning signs of an impending diagnosis if the decline persists. Prompt treatment may then forestall the more serious outcome.
Epilepsy
The mental functioning of children with epilepsy is at risk of impairment by the underlying brain malfunctions, the seizures themselves and the side effects of antiepileptic agents. Most children with epilepsy score within normal limits on IQ tests such as the WISC-R, but the distribution of IQs is skewed toward the lower end of the range. Lower IQ scores reflect the detrimental effects of the total number of seizures, which is compounded of age of onset and frequency of the seizures (226). Among seizure subtypes, minor motor and atypical seizure states are associated with lower mean IQs than other seizure types. Even in children with an IQ in the normal range, neuropsychological testing can pinpoint cognitive domains that present individual difficulty. Examples are the verbal learning and memory difficulty associated with complex partial seizures that arise from left-sided foci and the visuospatial learning and memory deficits that accompany right focal discharges. Left focal temporal discharges also may underlie dysnomia and circumlocution in speaking (227). A study of children with complex partial seizures found cognitive and linguistic deficits that were predicted by the duration and frequency of seizures and by the number of antiepileptic drugs that were used (228). Petit mal implicates sustained attention only. The more severe manifestations of epilepsy are often also associated with dysarthria, general inattentiveness, and slowing of responding. Seizures and antiepileptic drug treatments are discussed in Chapter 14.
AUTISTIC SPECTRUM DISORDERS
Autistic spectrum disorders (ASD) are a behaviorally defined set of developmental disorders that result from diverse biologic, genetic, and ecogenetic factors (229). Although the broad spectrum of cognitive and behavioral impairments defies a concise definition, clinicians tend to agree on its predominant features (230,231). Research into the neurobiology of ASDs is complicated by their broad heterogeneity in clinical and biological characteristics (see examples in Table 18.7; 232, 233, 234, 235, 236, 237, 238, 239, 240, 241, 242, 243, 244, 245, 246, 247, 248, 249, 250, 251, 252, 253, 254, 255, 256, 257, 258, 259, 260, 261, 262, 263, 264, 265, 266, 267, 268, 269, 270, 271, 272, 273, 274, 275, 276, 277, 278, 279, 280, 281, 282, 283, 284, 285, 286, 287, 288, 289, 290, 291, 292, 293, 294, 295, 296, 297, 298, 299, 300, 301, 302, 303, 304).
TABLE 18.7 Some Neurobiologic Clues to the Etiology of Idiopathic Autism | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
When Kanner described and named autism in 1943 (305), he noted the following five characteristics in the 11 children he described: inability to relate to people, absent or abnormal and noncommunicative speech, obsessive desire to maintain sameness, but good cognitive potential and normal physical status. Autism was initially ascribed to dynamic causes, in line with the theoretical orientation of the times (cf. DSM I, DSM II). Reflecting the rise of biologic psychiatry, in 1980, the Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III), abandoned the psychodynamic approach for the medical model and adopted an atheoretical nomenclature. The current criteria for autistic disorder in the DSM-IV include qualitative impairment in social interaction; qualitative impairment in communication; and restricted, repetitive, and stereotyped patterns of behavior, interest, and activities (48). By definition, onset is before 3 years of age. The World Health Organization’s International Classification Diseases (ICD-10) invokes similar criteria (63). Rett syndrome, discussed in Chapter 3, and childhood disintegrative disorder (CDD) are separately classified. Autistic disorder, Asperger syndrome, Rett syndrome, and childhood disintegrative disorder are subsumed under the category of pervasive developmental disorders (PDD) in the DSM-IV (65).
The distinctions between the diagnostic categories are arbitrary and probably reflect differences in degree rather than kind (306). In family studies, different PDD subtypes cluster within the same pedigree, indicating that they share common causes. In the family of a proband with PDD, there is a 3% chance that another offspring has autistic disorder and a further 3% chance of an offspring with PDD or Asperger’s disorder (307). Concordance between monozygotic twins is about 70% as opposed to 5% for dizygotic twins (308).
Approximately one-third of children appear to develop normally until the second year of life, at which time they gradually regress into autism (309,310), often in the context of seizures (312). Subtly abnormal signs may precede the overt regression (313). Some of these children may have become autistic after sustaining brain damage postnatally (314).
Clinical Characteristics
As a psychopathology, autism is profoundly internalizing. The children are deeply preoccupied with their internal states of mind and feeling and only minimally engage the outside world for purposes of activities of daily living. The majority of children with autism are to a varying degree atypical even at an early age, moving and crying little, averse to being held, and content to be alone. Scales that assist earlier diagnosis are available, and home videos reviewed retrospectively can reveal a previously unsuspected onset during infancy (315,316). The children may reject solid foods, and toys elicit little interest or are held onto with unusual obstinacy. Their motor development is usually normal, but minor physical anomalies are more frequently found in autistic children than in controls (317). During the second year of life, children with autism are typically unusually sensitive to auditory, visual, tactile, and movement stimulation, and repetitive mannerisms or gestures begin to appear. The older child with autism has restricted and stereotyped behaviors and activities and markedly impaired creativity, social relations, language, and perception. Disturbances in social relations are manifested by poor or absent eye contact and a lack of interest in people, whom the child uses instrumentally rather than interactively. Toys are handled bizarrely or are dropped when handed to the child. Mannerisms include repetitive, stereotyped movements, such as hand flapping, ear flicking, or head banging (318). Toe walking, whirling, and rocking also are common. These movements, often complex, increase when the child is anxious or is confronted with a novel situation (319).
Language disturbances can consist of complete lack of speech, failure to communicate by pointing, failure to imitate (320), perseveration, echolalia (repeating words or phrases out of communicative context), and lack of reciprocity in dialogue (321). If speech does develop, its prosody is often monotonal, pronouns are used poorly, and humor is not understood. Speech in children with autism differs qualitatively from the speech of children with mild mental retardation. Within the limits of a restricted vocabulary, children with mild mental retardation typically speak normally, whereas children with autism use abnormal prosody, syntax, semantics, and pragmatics (322). In some children, termed hyperlexic, mechanical reading skills develop out of proportion to spontaneous verbal expression or reading comprehension (323,324).
Children with autism may be oversensitive to stimuli, notably self-created sounds or spinning objects (325). This oversensitivity can alternate with periods of nonresponsiveness to speech, objects, or pain. Affected children frequently ignore sounds and are “aloof,” provoking testing for possible hearing loss. Some have prolonged attention spans during self-initiated activity (326). Observational studies demonstrate hyperselectivity of attention in children with autism (319). They focus exclusively on a single distinctive aspect of a display, while ignoring its other features. They are impaired in broadening the spatial spread of visual attention (326a). Conversely, the excel as compaud to their typical peers on tests that calls for local perceptual processing, in which context has got to be discounted. An example is the Embedded Figures Task (326b). The propensity of some people with autism to achieve savant status on very narrowly defined skells (326c) also reflects their narrow focus. Children with autism also have been shown to be impaired in perceiving faces, but not objects (327). People’s clothing was more salient to autistic children then their emotional expressions (328). They fail as compaud to age-matched peers in infering other
people’s perspectives and mental states, focusing narrowly on their own (326d).
people’s perspectives and mental states, focusing narrowly on their own (326d).
Some children exhibit transitional or milder degrees of autistic behavior, within the PDD spectrum. After age 5 to 6 years, such behaviors may merge with those observed in mental retardation. Others deviate into childhood disintegrative disorder (329) or Asperger disorder (330). The natural history and outcome of autism is variable. Some 80% manifest a pronounced impairment in intelligence. Approximately one-third of children with autism do not develop communicative speech. Others develop rudimentary language, although their communication remains literal and concrete and their affect flat. In yet other affected children, characteristics of organic brain disease become apparent over subsequent years, including auditory or visuoperceptual impairment. A small subset of children with autism develops bizarre thoughts and even delusions. About 75% of children who fail to show language skills by age 5 years fail to adjust personally or socially. Other children with autism make a fairly adequate social adjustment but retain certain peculiarities of personality, lack of humor, and unawareness of social nuances (331). Neuropsychologic testing reveals deficits on problem-solving tasks (332). Standard diagnostic instruments include the ADI (332a) and the ADOS (332b). Early diagnosis is facilitated by the use of standard instruments such as the Checklist for Autism in Toddlers (CHAT) (333). It consists of nine questions asked of the parents, and five items that call for observation by the clinician. The latter include pointing and looking to where a parent is pointing and pretend play, activities that are available to a normal 18 month old. Approximately one-half of the population with autism have an IQ above 50, and one-fourth to one-third have an IQ above 70. Children who regressed into autism after initially developing normally generally are ultimately more impaired cognitively (312,334). Even when they are enrolled in treatment programs, only some children with ASD improve significantly. If children improve, they usually do so during the second half of their first decade.
Prevalence
Based on twin studies, autism is thought to have the heaviest genetic loading of the chief developmental disorders, with more than 50% hereditability for the narrowly defined autistic disorder (335), and as much as 90% for the wider range of ASD (336). Moreover, autistic individuals rarely reproduce (337). Autism would therefore be expected to have a stable incidence. On the contrary, its prevalence across the ASD spectrum has risen from 2 to 4 in 10,000 children in the 1970s to 60 in 10,000 children in recent years, that is, 0.6% of the population (338,339,340,341,342,343,344,345). The rate of increase in autism is highest in developed countries, in the United States among children of American rather than immigrant mothers, and for autistic children who are high-functioning (346). It has been argued that the rise in prevalence is due to relaxation in diagnostic criteria, diagnostic substitution [e.g., ASD diagnosis substituted for Developmental Language Disorder (DLD) diagnosis—(346)], changes in and increasing availability of special education services, mandatory notification of ASD diagnoses, and increasing awareness and earlier recognition of ASD. However, the rise in incidence is so worldwide that it cannot be attributed to regulatory changes in just one country. Potential alternative causes and a true rise in incidence are not mutually exclusive, and the explanatory power of the alternative factors is open to challenge (347,348). No published research has managed to determine how much of the variance in the spectacular increase in ASD diagnoses is attributable to each of the various factors that have been suggested. Pending such information, it is unwarranted to assume that the true incidence of ASD is not increasing.
Causes of Autism and Its Neurobiologic Basis
Pathogenesis
Autism clearly has genetic factors in its origins. Previous theories that certain family dynamics promote autism (349) have been refuted (238). However, autistic offspring are more frequent among mothers of relatively high intelligence (346) and perhaps social class (350). The importance of genetics in autism is illustrated by the four to one higher incidence of autism in males (336), a recurrence risk of up to 9% in families with one affected child (351), a high concordance of autism among monozygotic twins (336,352), an increased incidence of developmental and affective disorder in first-degree relatives (350), and the association of some disorders of known genetic etiology with autism. Susceptibility loci have been identified on distal 7q and 15q11–13 (353).
Increased head and brain size in autism contrasts with the frequent microcephaly of mentally retarded children (354). However, there is also an excess of microcephaly among autistic children who are mentally retarded and have diagnosable medical diseases. Autistic macrocephaly indicates an enlarged brain, according to measures of brain volume by MRI. The bulk of the increase is in cerebral and cerebellar white matter. It is not evident at birth, but develops throughout the first year of life (354a), and mostly consists of increased volume of the peripheral (radiate) cerebral white matter (355). It is perhaps the most consistently replicated neurobiologic feature of ASD (356). There is no consensus on the neural pathophysiology of autism (357). Structural abnormalities in various brain regions of autistic children may reflect etiologic heterogeneity. They include widespread abnormalities in the frontal and temporal cortices, cerebellar hemispheres, and vermis (358,358,359,360,361,362). An overview of neuropathologic findings (363) highlights the limbic system (increased cell packing density and smaller neurons in 9 of 14 cases), the
cerebellum (21 of 29 had a decreased number of Purkinje cells), and cerebral cortex (more than half had dysgenesis). Purkinje cell loss in the cerebellum is the most consistent microscopic neurological abnormality found in autism. The high energy demands of these large neurons makes them vulnerable to damage following a variety of insults (364), and the associated presence of gliosis (362) opens up the possibility of damage rather than dysgenesis. The neural substrate of autistic disorders has typically been thought to be the medial temporal lobe and limbic structures (365,366). Bilateral excisions of amygdala and hippocampus of monkeys resulted in impairment of social interaction (367). The hypothesis that autistic behaviors are attempts to compensate for frequent phasic overarousal (368) has found support in recent neuroanatomic (369) and physiologic (370) findings that suggest that the cortical network is underconnected and therefore insufficiently inhibited (371).
cerebellum (21 of 29 had a decreased number of Purkinje cells), and cerebral cortex (more than half had dysgenesis). Purkinje cell loss in the cerebellum is the most consistent microscopic neurological abnormality found in autism. The high energy demands of these large neurons makes them vulnerable to damage following a variety of insults (364), and the associated presence of gliosis (362) opens up the possibility of damage rather than dysgenesis. The neural substrate of autistic disorders has typically been thought to be the medial temporal lobe and limbic structures (365,366). Bilateral excisions of amygdala and hippocampus of monkeys resulted in impairment of social interaction (367). The hypothesis that autistic behaviors are attempts to compensate for frequent phasic overarousal (368) has found support in recent neuroanatomic (369) and physiologic (370) findings that suggest that the cortical network is underconnected and therefore insufficiently inhibited (371).
Etiology
Many genetic syndromes feature autistic behavior, notably Rett syndrome (372), fragile X syndrome (373), and occasionally Down syndrome (see Chapters 3 and 4). An intriguing instance is Timothy syndrome, a rare multisystem disorder that features cardiac arrhythmias and both cognitive and physical deficits. It is caused by a mutation in the CaV1.2 calcium channel (374) that incurs the risk of excessive entry of calcium into the cell. That some children become autistic, and that others with the same mutation do not, suggests that the autistic phenotype requires some additional epigenetic or environmental factor. The raised incidence of autism in thalidomide (375) and valproic acid (176,398) embryopathies indicates that an abnormal event such as a poisoning can trigger autism as early as 20 to 24 days after conception (376). Children with autism often have recurrent seizures (377) and EEG abnormalities usually with onset in the first year of life (378). The neurological symptoms of tuberous sclerosis become apparent only after the onset of seizures. Seizures that interact with pre-existing temporal lobe abnormalities may result in manifestations of autism. Tuberous sclerosis is discussed in Chapter 12. Perinatal injuries (232,233,234,235,236,379) and prematurity (380) are associated with autism with greater than chance frequency. However, the evidence more usually indicates prenatal maldevelopment even early in the first trimester (376). Rarely, an autistic syndrome arises during encephalitis (381), even at as late an age as 31 years (382). Therefore, autism is not always a developmental disorder.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree