ANOREXIA NERVOSA
Clinical features
This is a disorder characterized by deliberate weight loss, induced and/or sustained by the patient using a number of strategies, including avoiding ‘fattening’ foods, self-induced vomiting and/or purging, excessive exercise, and using diuretics and/or appetite suppressants. The ICD-10 criterion for body weight is that it is maintained at least 15% below that expected, or that Quetelet’s body-mass index (mass (kg)/[height (m)]2) is equal to or less than 17.5. The patient has body-image distortion and a dread of fatness.
Disorder of the hypothalamic–pituitary–gonadal axis leads, in women, to amenorrhoea (although if taking the oral contraceptive pill breakthrough vaginal bleeding continues to take place), and in men to low libido and erectile dysfunction. If the onset is prepubertal in girls, breast development does not take place and there is primary amenorrhoea; in boys the genitals do not develop.
Gastrointestinal complications include:
• Delayed gastric emptying
• Impairment of hunger and satiety sensations
• Delayed small bowel transit time
• Constipation
• Gastric dilatation.
Psychiatric symptomatology most commonly associated with anorexia nervosa includes:
• Anxiety, particularly related to food and eating
• Mood disorder, including depressive episodes (with suicidal thoughts, poor concentration and social withdrawal) and labile mood.
DSM-IV-TR criteria for anorexia nervosa
The four criteria are:
• Refusal to maintain body weight at or above a minimally normal weight for age and height (e.g. weight loss leading to maintenance of body weight < 85% of that expected; or failure to make expected weight gain during period of growth, leading to body weight < 85% of that expected
• Intense fear of gaining weight or becoming fat, even though underweight
• Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight
• In postmenarchal females amenorrhoea, i.e. the absence of at least three consecutive menstrual cycles. (A woman is considered to have amenorrhoea if her periods occur only following hormone, e.g. oestrogen, administration.)
Restricting type
During the current episode of anorexia nervosa the patient has not regularly engaged in binge-eating or purging behaviour (i.e. self-induced vomiting or the misuse of laxatives, diuretics or enemas).
Binge-eating/purging type
During the current episode of anorexia nervosa the patient has regularly engaged in binge-eating or purging behaviour (i.e. self-induced vomiting or the misuse of laxatives, diuretics or enemas).
Physical examination
Patients appear thin and emaciated. There may be evidence of dehydration, salivary gland swelling, dental caries and perimolysis. Lanugo hair is often present on the face, back, abdomen and forearms. Axillary and pubic hair are present (cf. hypopituitarism in which they are absent or scanty). There may be evidence of a poor peripheral circulation, including acrocyanosis (Fig. 8.1). The presence of purpura may be serious, potentially indicating a bleeding diathesis.
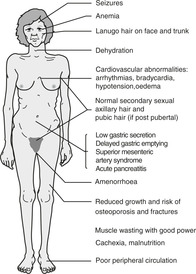 |
| Figure 8.1 (With permission from Puri BK, Laking PJ, Treasaden IH 2002 Textbook of psychiatry. Churchill Livingstone, Edinburgh.) |
Investigations
The differential diagnosis of anorexia nervosa (and bulimia nervosa) is summarized in Table 8.1. Organic causes of weight loss in young patients should be excluded, e.g. chronic debilitating diseases, brain tumours and intestinal disorders such as Crohn’s disease or malabsorption syndromes. The body weight and height should be carefully measured. The former acts as a baseline from which to monitor progress during treatment. Abnormal investigation results that may be found include the following.
| Psychiatric | Depression |
| Obsessive–compulsive disorder | |
| Personality disorder | |
| Physical | Chronic debilitating disorders |
| Neoplasia | |
| Thyroid disorder | |
| Intracranial space-occupying lesions | |
| Malabsorption syndromes | |
| Intestinal disorders, including Crohn’s disease |
Haematological
Leukopenia and mild anaemia are common; thrombocytopenia occurs rarely.
Metabolic
• Metabolic alkalosis (↑plasma bicarbonate), hypochloraemia and hypokalaemia secondary to induced vomiting
• ↑Blood urea nitrogen secondary to dehydration
• Hypercholesterolaemia is common in spite of emaciation – serum levels of cholesterol, cholesterol ester transfer protein (CETP) and apolipoproteins decrease after weight gain, suggesting increased cholesterol metabolism in patients who have normal serum levels of free fatty acids
• Raised liver function tests may occur
• Hypomagnesaemia, ↑plasma amylase, fasting hypoglycaemia, ↓plasma zinc and hypercarotenaemia are occasionally seen
• Plasma protein and albumin levels are commonly normal.








