23 EC-IC Bypass for Giant ICA Aneurysms
Introduction
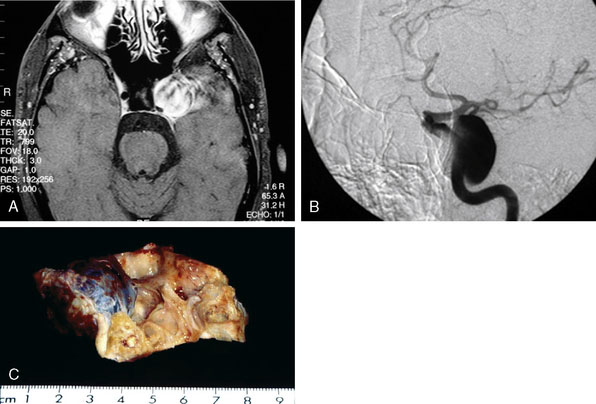
Pure cavernous ICA aneurysms are a separate category of aneurysms, which do not extend beyond the dural ring of the ICA. In general, in the neurosurgical literature these aneurysms are considered benign, even in larger sizes.1 However, in our experience it is possible that when these aneurysms get significantly large in size, they can cause rupture through the middle fossa dura, causing hemorrhage and potential mortality (Figure 23–1).
Natural history of transitional segment of ICA aneurysms
Unruptured intracranial aneurysms are being diagnosed more often than in the past and these lesions pose management problems. The first series of giant aneurysms was presented in 1969 by Morley and Barr, who described giant aneurysms as >2.5 cm.2 Giant aneurysms are relatively rare, comprising between 5% and 7% of aneurysms3 in most series. Giant aneurysms have a female predominance with ratios as high as 3:1 in some series4 and most commonly present in the middle decades. Giant aneurysms are most frequently located on the ICA, specifically, involving the paraclinoid segment 21% of the time.5
The natural history of giant aneurysms is one of a poor prognosis. Some have compared the fate of unruptured giant aneurysms to that of subarachnoid hemorrhage (SAH).6 Patients often present with symptoms consistent with SAH or mass effect. The Italian cooperative study has shown a 28% mortality rate for untreated giant aneurysms compared to a 14% mortality rate for patients who received treatment.7 In the same series, morbidity was seen in 48% of cases due to expansion. Giant aneurysms, not unlike other aneurysms, continue to enlarge over time. Expansion is thought to be from growth of the lumen or thrombus formation within the sac. This progressive enlargement often causes symptoms of mass effect.8
Historically, it was thought that giant aneurysms were less prone to rupture; however, contemporary evidence suggests that this is inaccurate. Drake found that 62 of 174 cases did rupture.9 Aneurysms sized ≥25 mm had a relative risk of rupture of 59% compared to aneurysms <10 mm.10 Giant aneurysms had a 6% rupture rate in the first year compared to <1% for aneurysms <10 mm.10 Patients with a giant aneurysm, but without previous SAH, were at a significantly increased risk for rupture based on size. The rupture rate was not dependent on the location of the aneurysm; all anterior circulation giant aneurysms were at increased risk of rupture.3 Risk factors for aneurysm rupture include hypertension, current or former tobacco use, alcohol use greater than five drinks per day, and use of oral contraceptives.10 It was thought that partially or completely thrombosed aneurysms would be less likely to rupture, thus not requiring treatment; however, in Drake’s large series, this was not the case.9
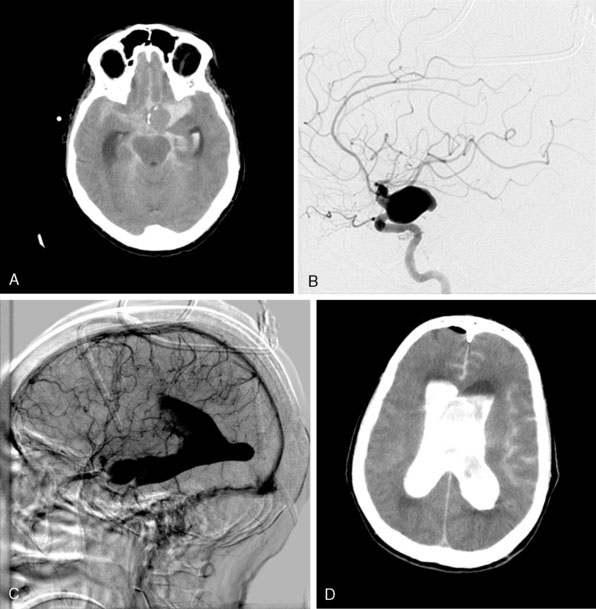
The ISUIA (International Study of Unruptured Intracranial Aneurysms Investigators) trial has shown that un-ruptured aneurysms overall do not pose the risk they once were thought to; and that treating aneurysms, specifically small ones, puts the patient at more risk than surveillance. However, this advice should not be applied to the special case of giant aneurysms, where “the natural history is ominous.”6 Morley and Barr’s original series demonstrated similar findings, with an 80% mortality rate for untreated aneurysms. Other studies have shown high 1-year mortality rates.11 Peerless et al. found that 85% of patients with giant intracranial aneurysms were dead at 5 years.12 Additionally, the ISUIA II found that the cumulative rupture rates for anterior circulation giant aneurysms with no previous history of SAH were 40%. Patients who present with SAH are at increased risk of mortality compared to patients without SAH.13 We present a case of a ruptured giant aneurysm without previous history of SAH 6 months after initial diagnosis (Figure 23–2).
The Dilemma of Deliberate ICA Occlusion
Traditional neurosurgical literature and practice have held a liberal view of ICA occlusion for the treatment of giant ICA aneurysms. Historically, this has been accompanied by a relatively high risk of stroke following the ICA occlusion (Table 23–1). With recent improvements in the balloon test occlusion (BTO) paradigms, the risk is smaller but clearly not absent.
| Source | Surgery | Outcomes |
|---|---|---|
| Sahs and Locksley, 196914 | ICA ligation | Stroke 30% Mortality 20.7% |
| Roski et al., 198115 | ICA ligation | TIA 16.6% Stroke 16.6% SAH 5.5% Mortality 5.5% |
| Linskey et al., 199416 | Intravascular ICA occlusion | Stroke 12.9% Mortality 3.2% |
| Larson et al., 199517 | Intravascular ICA occlusion | TIA 10.9% Stroke 3.6% SAH 3.6% Mortality 5.4% |
ICA, internal carotid artery; SAH, subarachnoid hemorrhage; TIA, transient ischemic attack.
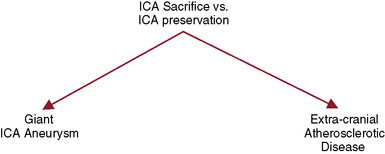
For the treatment of carotid occlusive disease, traditional neurosurgical literature and practice have strongly recommended preservation of the ICA. High-grade stenosis (i.e., 99% stenosis) is considered a relative neurosurgical emergency, requiring an endarterectomy or stenting. It is interesting that most patients who present with cervical carotid occlusive disease are usually older and generally have multiple medical comorbidities; yet performing a procedure to open the carotid artery has remained standard practice. Most cervical carotid occlusive disease symptomatology is due to embolic disease rather than hemodynamic compromise. Therefore, in the majority of cervical carotid occlusive disease, a deliberate occlusion of the ICA, in the opinion of the senior author, could be performed with a relatively low risk of morbidity, and most likely less risk of morbidity and mortality, when compared to carotid endarterectomy or stenting. However, this would be considered a complete departure from our current standards of care (Figure 23–3).
Experience at St. Louis University Hospital in Treatment of Giant ICA Aneurysms
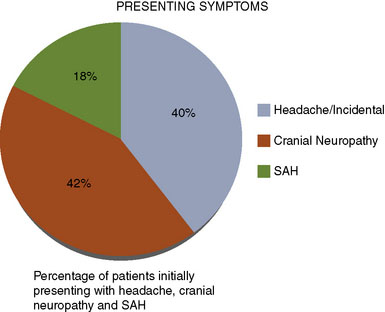
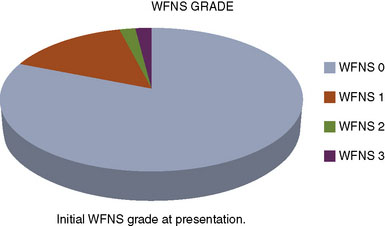
We performed a retrospective review of 55 consecutive patients treated at St. Louis University Hospital from June 1999 to June 2007. All 55 patients had transitional ICA aneurysms. The mean aneurysm size was 34.7 mm (range 25 to 70 mm). The mean age was 46 years (range 30 to 64 years). The mean follow-up period was 34.7 months (range 1 to 76 months). The objectives of this study were to assess the use of high-flow EC-IC bypass for the treatment of giant transitional ICA aneurysms, delineate surgical mortality and morbidity, and determine the long-term efficacy of the treatment and functional outcomes of these patients. The presenting symptoms were cranial neuropathy (42%), headache or incidental finding (40%), and SAH (18%) (Figure 23–4). The World Federation of Neurological Surgeons (WFNS) grade was 0 in 81%, 1 in 15%, 2 in 2%, and 3 in 2% (Figure 23–5). All 55 patients underwent a high-flow EC-IC bypass procedure.
Surgical technique
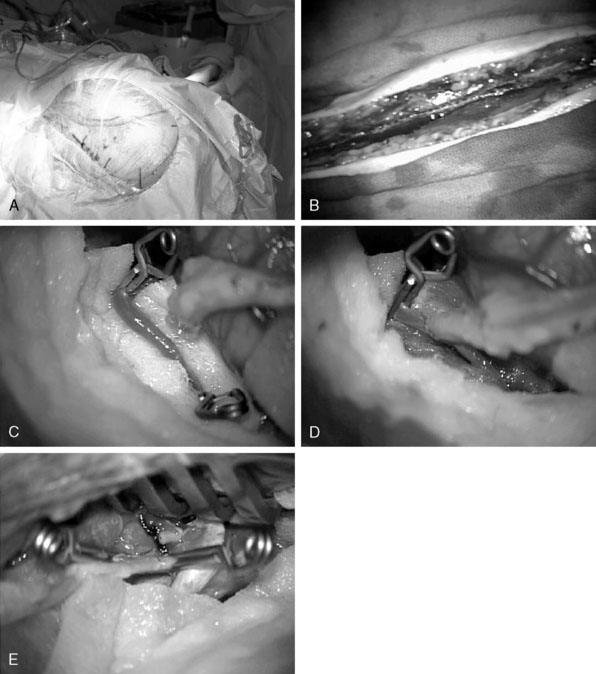
Craniotomy: A skull base approach, usually a cranio-orbital or a cranio-orbital-zygomatic access, is usually needed. We prefer a single-piece craniotomy, which entails an osteotomy of the orbital roof and lateral margins. A high-speed drill is used to thin the zygomatic arch posteriorly, which allows the radial artery to lie without kinking at the zygomatic area (Figure 23–6A).
Radial artery harvest: The critical aspect of radial artery harvest is the length of the graft, which can be limiting. Obtaining maximal length is critical during this harvest. The senior author prefers to personally mark the superficial wall of the radial artery with a marking pen prior to removal of the graft. This step is crucial to avoid rotation during the tunneling (Figure 23–6B). Once the graft is harvested, it is placed in a heparinized saline solution.
Intracranial anastomosis: We also start the patient on aspirin (81 mg) daily for 3 days prior to surgery. Intraoperative continuous electroencephalography (EEG), somatosensory-evoked potential (SSEP), and motor-evoked potentials are monitored. The site of the anastomosis is determined based on several factors: intended revascularization territory, size of donor and recipient vessels, length of the graft, and location of the aneurysm. Mild hypothermia is used. EEG burst suppression using pentobarbital is maintained during the temporary clipping period. A color background is placed behind the recipient vessel. Temporary clips are applied (Figure 23–6C). An arteriotomy is made using an arachnoid knife. The arteriotomy is extended using a microscissors to the width of the donor vessel lumen. The lumen of the donor vessel is expanded by “fish-mouthing” the opening. We used 9-0 nylon for M2 and M3 vessels and 8-0 nylon for the supraclinoidal ICA. We prefer a running suture technique and performing the “back” wall (i.e., the more difficult anastomosis) first, followed by the front wall (Figure 23–6D). When the anastomosis is completed, retrograde flow is confirmed in the graft followed by positioning of a temporary clip on the graft just distal to the anastomosis.
Cervical carotid anastomosis: The graft length is cut to expose an area of the ECA where the proximal anastomosis is planned. Yasargil long temporary clips can be used for the ECA anastomosis. Similar technique of “back” wall and “front” wall can be utilized as described previously for the intracranial anastomosis. For this part, 7-0 prolene can be used (Figure 23–6E).
Parent vessel occlusion: Once the preceding steps, including intraoperative angiography, have documented flow in the graft, we then advocate parent vessel occlusion during the same surgical procedure, rather than delayed (staged) occlusion. In our opinion, the risk of graft occlusion would be high if competitive flow in the parent vessel were allowed to continue. We occlude the ICA at the level of the bifurcation in the cervical area and just distal to the giant aneurysm in the supra-clinoidal portion of the ICA. The distal occlusion must be performed proximal to the anterior choroidal and dominant posterior communicating arteries.18
Results of Giant Aneurysm Series
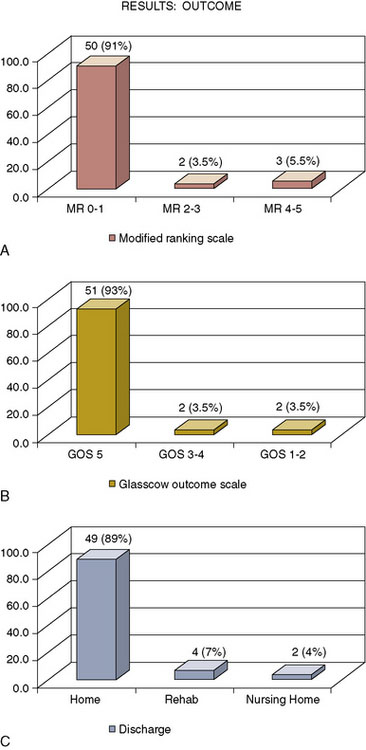
The outcome of this series shows that 50 patients (91%) had a Modified Rankin Scale (mRS) of 0 to 1, two patients (3.5%) had a mRS of 2 to 3, and three patients (5.5%) had a mRS of 4 to 5. Fifty-one patients (93%) had a Glasgow Outcome Scale (GOS) of 5, two patients (3.5%) had a GOS of 3 to 4, and two (3.5%), a GOS of 1 to 2. At discharge from the hospital, 49 (89%) of the patients went home, four (7%) went to rehabilitation facilities, and two patients (4%) went to nursing homes (Figure 23–7).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree