Chapter 16 Transcutaneous electrical nerve stimulation (TENS)
INTRODUCTION
Transcutaneous electrical nerve stimulation (TENS) is a simple, non-invasive analgesic technique that is used for the symptomatic management of acute and non-malignant chronic pain (Box 16.1; Barlas & Lundeberg 2006, Walsh 1997a, Woolf & Thompson 1994). TENS is also used in palliative care to manage pain caused by metastatic bone disease and neoplasms (Berkovitch & Waller 2005, Stannard 2002, Thompson & Filshie 1993). It is claimed that TENS also has antiemetic and tissue-healing effects, and that it can improve some of the neurophysiological and behavioural effects of dementia (Cameron et al 2003, Walsh 1997b). It is used less often for these non-analgesic actions.
Box 16.1 Common medical conditions for which TENS has been used
Surveys show that TENS is one of the most frequently used electrotherapies for pain relief and that it is available throughout the world (Johnson 1997, Pope et al 1995, Reeve et al 1996, Robertson & Spurritt 1998). TENS is popular because it is cheap, non-invasive, easy to administer, has few side effects and has no drug interactions. There is no potential for toxicity or overdose. TENS is commonly prescribed by doctors, physiotherapists, nurses and midwives; patients in the UK can also buy a TENS device for their own use. It is preferable for patients to administer TENS for themselves, following appropriate instruction by a healthcare professional. TENS effects are rapid in onset for most patients, so benefit can be achieved almost immediately.
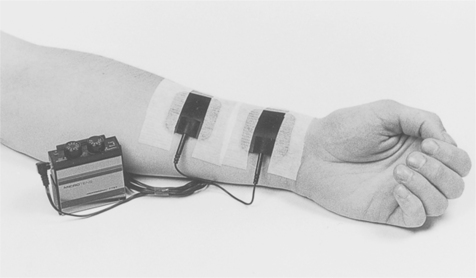
During TENS, pulsed electrical currents are generated by a portable pulse generator and delivered across the intact surface of the skin via conducting pads called electrodes (Fig. 16.1). The conventional way of administering TENS is to use electrical characteristics that selectively activate large-diameter non-noxious afferents (Aβ) without activating smaller-diameter nociceptive fibres (Aδ and C). Evidence suggests that this will produce pain relief in a similar way to ‘rubbing the pain better’. In practice, conventional TENS is delivered to generate a strong but comfortable paraesthesia within, or close to, the site of pain using frequencies anywhere between 1 and 200 pulses per second (pps) and pulse durations anywhere between 50 and 500μs.
HISTORY
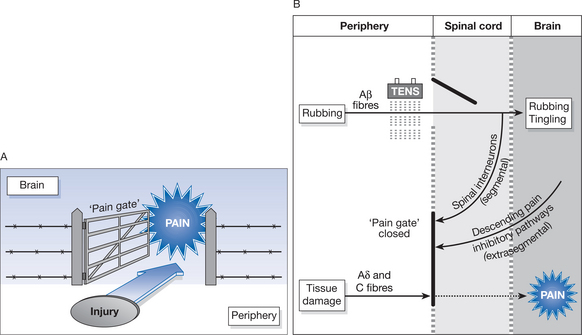
The use of electricity to relieve pain is an age-old technique. The ancient Egyptians used electrogenic fish to treat ailments in 2500 bc, although the Roman physician Scribonius Largus is credited with the first written report of the use of electrogenic fish in medicine in AD46 (Kane & Taub 1975). The development of electrostatic generators in the eighteenth century increased the use of medical electricity, although popularity declined in the nineteenth and early twentieth centuries owing to variable clinical results and the development of pharmacological treatments (Stillings 1975). Interest in the use of electricity to relieve pain was re-awakened in 1965 by Melzack and Wall, who provided a physiological rationale for electroanalgesic effects. They proposed that transmission of noxious information could be inhibited by activity in large-diameter peripheral afferents or by activity in pain inhibitory pathways descending from the brain (Fig. 16.2). Wall and Sweet (1967) used high-frequency percutaneous electrical stimulation to artificially activate large-diameter peripheral afferents and found that this relieved chronic pain in patients. Pain relief was also demonstrated when electrical currents were used to stimulate the periaqueductal grey (PAG) region of the midbrain (Reynolds 1969), which is part of the descending pain inhibitory pathway. Shealy et al (1967) found that electrical stimulation of the dorsal columns, which form the central transmission pathway of large-diameter peripheral afferents, also produced pain relief. TENS was used to predict the success of dorsal column stimulation implants until it was realised that TENS could be used as a successful modality on its own (Long 1973, 1974).
DEFINITION
By strict definition, TENS is anything that delivers electricity across the intact surface of the skin to activate underlying nerves. Healthcare professionals use the term ‘TENS’ to describe a ‘standard TENS device’ (see Fig. 16.1), although literature about TENS uses ambiguous and inconsistent nomenclature. This has resulted in inappropriate clinical practice.
THE STANDARD TENS DEVICE
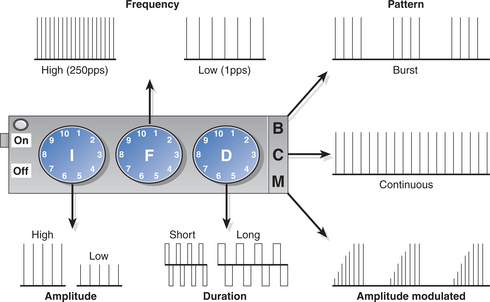
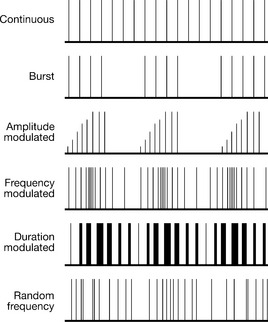
Standard TENS devices are characterized by their technical output characteristics, and in the UK they retail at between £30 and £150 (Table 16.1). Standard TENS devices vary between manufacturers but these variations are minor and have a limited impact on the physiological effects produced. Standard TENS devices usually deliver biphasic pulsed currents in a repetitive manner using pulse durations of between 50 and 500 μs and pulse frequencies of between 1 and 200 pulses per second (pps) [American Physical Therapy Association (APTA) 1990, Barlas & Lundeberg 2006, Mannheimer & Lampe 1987, Sjölund et al 1990, Walsh 1997a, Woolf & Thompson 1994]. Pulses are usually delivered in a continuous pattern, although most modern devices have other patterns available, such as burst, modulated amplitude, modulated frequency, and modulated pulse duration (Fig. 16.3).
Table 16.1 Typical features on TENS devices
| Feature | Examples |
|---|---|
| Weight | 50-250g |
| Dimensions | 6 × 5 × 2 em (small device) 12 × 9 × 4cm (large device) |
| Cost | £30-150 |
| Pulse waveform (fixed) | Monophasic Symmetrical biphasic Asymmetrical biphasic |
| Pulse amplitude (adjustable) | 1-50mAintoa 1 kO,load |
| Pulse duration (often fixed) | 50-500 μ5 |
| Pulse frequency (adjustable) | 1-200pps |
| Pulse pattern | Continuous, burst (random frequency, modulated amplitude, modulated frequency, modulated pulse duration) |
| Channels | 1 or 2 |
| Batteries | PP3 (9V), rechargeable |
| Additional features | Timer Most devices deliver constant current output |
TENS-LIKE DEVICES
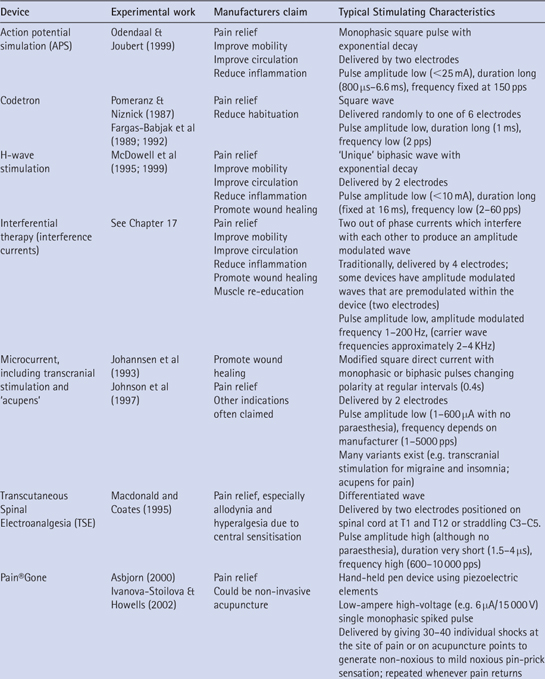
Developments in electronic technology have flooded the market with a variety of TENS-like devices (Table 16.2). TENS-like devices have been defined as any stimulating device that delivers electrical currents across the intact surface of the skin and whose technical output specifications and generic name differ from those of TENS (Johnson 2003). This includes interferential current therapy (IFT), microcurrent electrical therapy (MET), high-voltage pulsed (galvanic) current (HVPC), transcutaneous spinal electroanalgesia (TSE), action potential simulation (APS), H-wave therapy (HWT), Pain®Gone and transcranial electrical stimulation (TCES), to name but a few. TENS-like devices often have design features that are unique to a particular device and this makes categorization difficult. For example, some MET devices deliver currents at the site of pain using standard TENS electrodes; others deliver MET transcranially (e.g. as a type of TCES), and others deliver MET using a pen-like electrode. Claims about the relative effectiveness of TENS-like devices are overambitious and practitioners should use a standard TENS device in the first instance (Johnson 2003). The remainder of this chapter will focus on TENS administered using a standard TENS device.
PHYSICAL PRINCIPLES
The physiological intention of TENS when used for pain relief is to selectively activate different populations of nerve fibres to initiate antinociceptive mechanisms that produce clinically meaningful pain relief. The electrical characteristics of TENS determines which population of nerve fibres is activated, so it is important that the TENS user is familiar with the basic principles of nerve fibre activation and how this relates to TENS technique (this is described in Chapter 13).
PRINCIPLES OF NERVE FIBRE ACTIVATION
When the pulse amplitude (intensity) of TENS is increased, non-nociceptive nerve fibres are activated first and the user experiences a non-painful tingling under the electrodes. This is because large-diameter, non-nociceptive (touch) nerve fibres (Aα and Aβ fibres) have lower thresholds of activation to electrical stimuli than their small-diameter nociceptive counterparts (Aδ and C fibres; see Chapters 5 and 6). If the pulse amplitude (intensity) of TENS is increased further, nociceptive nerve fibres are activated and the user experiences a painful tingling under the electrodes.
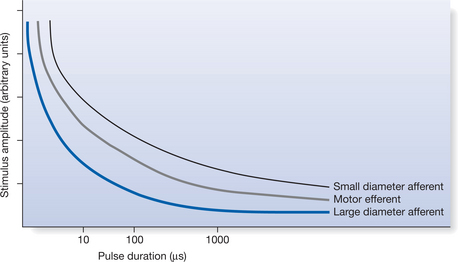
Pulse durations between 50 and 500 μs enable the user titrate pulse amplitude with greater precision (Howson 1978). Pulsed currents with small amplitudes (i.e. low intensity) and durations between 50 and 500 μs would be best to activate large-diameter fibres (Aβ) without activating small-diameter nociceptive fibres (Aδ and C) (Fig. 16.4). Increasing the pulse duration above 500 μs will lead to the activation of small-diameter fibres at lower pulse amplitudes. The number of nerve impulses generated by TENS will increase according to the frequency of the pulsed currents, although this is limited by the absolute and relative refractory periods for the axon. Theoretically, delivering TENS at high pulse frequencies (up to ∼200 pps) should be optimum (for a discussion, see Howson 1978, Walsh 1997e, Woolf & Thompson 1994).
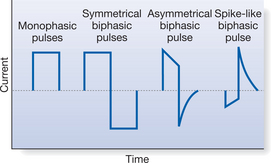
The type of pulsed current waveform used in TENS devices varies between manufacturers. Generally, these can be divided into monophasic or biphasic waveforms (Fig. 16.5). If the TENS device delivers a monophasic pulsed wave, the cathode should be placed proximal to the anode. This is because the cathode activates the axonal membrane, leading to an action potential, and placing the anode proximal could block nerve transmission due to hyperpolarization (Fig. 16.6, and see Chapter 13). The cathode is usually, but not always, the black lead. Many TENS devices use biphasic waveforms whereby the cathode and anode alternate between the two electrodes during stimulation. Biphasic waveforms, which result in zero net current flow, may prevent the build-up of ion concentrations beneath electrodes and reduce adverse skin reactions due to polar concentrations (Kantor et al 1994, Walsh 1997e). Electrode positioning with these biphasic waveforms is less critical given the zero net DC element and therefore orientation of positive/negative is not thought to make any significant clinical difference.
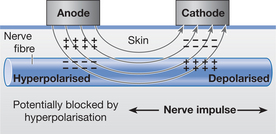
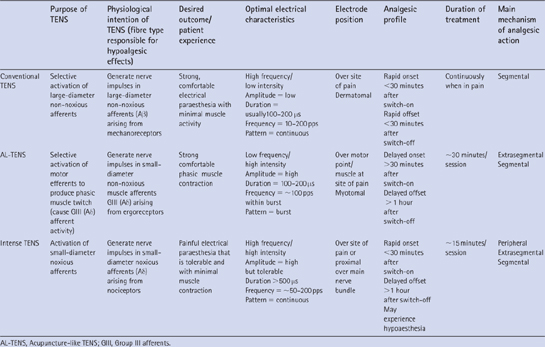
Figure 16.6 Fibre activation by TENS. When devices use waveforms that produce net DC outputs that are not zero, the cathode excites (depolarization) the axon and the nerve impulse will travel in both directions down the axon. The anode tends to inhibit the axon (hyperpolarization), which could extinguish the nerve impulse. Thus, during conventional TENS the cathode should be positioned proximal to the anode so that the nerve impulse is transmitted to the central nervous system unimpeded. However, during AL-TENS the cathode should be placed distally or over the motor point, as the purpose of AL-TENS currents is to activate a motor efferent. Table 16.3 The characteristics of different types of TENS
The theoretical relationship between output characteristics of electrical stimuli delivered and nerve fibre activation can break down in clinical practice. It has been shown that the exact nature and distribution of currents is difficult to predict when they are passed across the intact surface of the skin, due to the complex and non-homogeneous impedance of the tissue underlying electrodes (Demmink 1993). Furthermore, the skin offers high impedance at pulse frequencies used by TENS, so it is likely that currents will remain superficial, stimulating cutaneous nerve fibres rather than the more deep-seated visceral and muscle nerve fibres. Interestingly, however, recent evidence from animal studies suggests that activity in deeper afferents may be responsible for the antinociceptive effects of TENS (Radhakrishnan & Sluka 2005).
PRINCIPLES UNDERPINNING TYPES OF TENS TECHNIQUE
The most common types of TENS technique described in the literature are conventional TENS, acupuncture-like TENS (AL-TENS) and intense TENS (Table 16.3; Barlas & Lundeberg 2006, Mannheimer & Lampe 1987, Sjölund et al 1990, Walsh 1997a, Woolf & Thompson 1994). These TENS techniques suggest the electrical characteristics of the currents that are necessary to activate different types of nerve fibre, although the emphasis on electrical characteristics has resulted in the use of inflexible ‘prescriptive protocols’ in clinical practice and research. In addition, the emphasis on the electrical characteristics of TENS has driven the development of TENS devices with novel output characteristics (Fig. 16.7), which are based more on technological advances in electronics than on proven physiological effect. In clinical practice in the UK, conventional TENS is most commonly used by patients whereas AL-TENS and intense TENS tend to be used only in specific situations. It is important to establish the physiological intention of each TENS technique to appreciate their relative merits.
CONVENTIONAL TENS
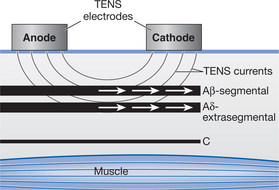
The physiological intention of conventional TENS is to selectively activate large-diameter Aβ fibres (touch related) without concurrently activating small-diameter Aδ and C fibres (pain-related) or muscle efferents (Fig. 16.8). Theoretically, high-frequency (∼10–200 pps), low-intensity (non-painful) currents with pulse duration between 50 and 500 μs would be most efficient in selectively activating Aβ fibres (see Table 16.3). As large-diameter fibres have short refractory periods, they can generate nerve impulses at high frequencies. This means that they are more able to generate high-frequency volleys of nerve impulses when high-frequency currents are delivered, resulting in a greater afferent barrage into the central nervous system.
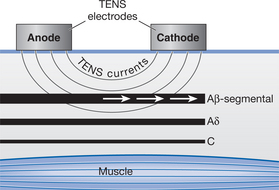
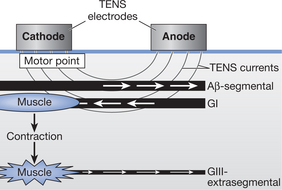
Figure 16.8 The aim of conventional TENS is to selectively activate Aβ afferents producing segmental analgesia.
Large-diameter afferent activity is occurring when the user reports ‘strong but comfortable’ non-painful electrical paraesthesia beneath the electrodes. Animal studies have demonstrated that TENS-induced large-diameter afferent activity inhibits ongoing transmission of nociceptive information in the spinal cord and reduces central sensitization (Garrison & Foreman 1994, 1996, Ma & Sluka 2001, Sandkühler 2000). This effect is often rapid in onset and offset. Studies on healthy human participants exposed to experimentally induced pain in laboratory settings demonstrate that TENS applied at a strong but comfortable level produces hypoalgesic effects over and above those seen with sham TENS (Johnson & Tabasam 1999, 2003, Walsh 1997d). Hence users should be trained to titrate pulse amplitude so that it is strong enough to generate a non-noxious paraesthesia (Aβ activity) without frank pain (Aδ or C fibre activity). It is claimed that the magnitude of analgesia achieved during conventional TENS depends in part on the pulse frequency. This is supported by studies in animals, which demonstrate that high- and low-frequency TENS may generate differential antihyperalgesic effects, which use different neurochemicals (Radhakrishnan & Sluka 2003, Radhakrishnan et al 2003, Sjölund 1985, Sluka et al 2000, 2005). However, the results of experimental studies in healthy human subjects and patients are inconsistent, with some demonstrating frequency-dependent effects (De Tommaso et al 2003, Johnson et al 1989, Walsh et al 1995) and others not (Barr et al 1986, Cramp et al 2000, Foster et al 1996, Walsh et al 2000).
ACUPUNCTURE-LIKE TENS (AL-TENS)
AL-TENS is often described – in vague terms – to be the delivery of low-frequency (e.g. <10 pps), high-intensity TENS. This has led to confusion about its physiological intention (Johnson 1998). Most, but not all, opinion leaders define AL-TENS as the induction of forceful but non-painful phasic muscle contractions at myotomes related to the origin of the pain (Eriksson & Sjölund 1976, Johnson 1998, Meyerson 1983, Sjölund et al 1990, Walsh 1997a). However, most research reports articulate AL-TENS as low-frequency, high-intensity TENS without any reference to the presence or absence of muscle contractions. Some commentators describe AL-TENS as the delivery of TENS over acupuncture points irrespective of muscle activity (Lewers et al 1989, Lewis et al 1990, Longobardi et al 1989, Rieb & Pomeranz 1992). It is possible that there are differences in physiological action when TENS is applied over acupuncture points in this way (see reviews by Johnson 1998, Walsh 1996).
The physiological intention of AL-TENS, as described by the opinion leaders who developed it, is to generate activity in small-diameter muscle afferents (Aδ or group III) that arise from ergoreceptors and respond to muscle contraction (Eriksson & Sjölund 1976, Sjölund et al 1990). This is achieved indirectly by activating Aα efferents to produce a forceful but non-painful phasic muscle twitch (Anderson et al 1973, Eriksson & Sjölund 1976, Eriksson et al 1979; Fig. 16.9). AL-TENS is administered over muscles or motor points at high but non-painful intensities using low-frequency pulses (∼1–10 pps) or low-frequency bursts of pulses (∼2–5 bursts per second of 100 pps). Burst patterns of pulse delivery were originally incorporated on TENS devices as they were found to be more comfortable than low-frequency single pulses in producing muscle twitches (Eriksson & Sjölund, 1976). The impulses generated in small-diameter muscle afferents initiate extrasegmental antinociceptive mechanisms and the release of endogenous opioid peptides in a manner similar to that suggested for acupuncture (Meyerson 1983, Sjölund et al 1977). It should be remembered that currents delivered during AL-TENS will also activate Aβ fibres during their passage through the skin leading to segmental analgesia (see Table 16.3).
INTENSE TENS
The physiological intention of intense TENS is to activate small-diameter Aδ afferents by delivering TENS over peripheral nerves arising form the site of pain at an intensity that is just tolerable to the patient (Jeans 1979, Melzack et al 1983; Fig. 16.10). Currents are administered at high frequencies (up to 200 pps) to prevent phasic muscle twitches that would be too forceful for the patient to tolerate (see Table 16.3). Cutaneous Aδ afferent activity has been shown to block transmission of nociceptive information in peripheral nerves and to activate extrasegmental antinociceptive mechanisms (Chung et al 1984a, 1984b, Ignelzi & Nyquist 1976, 1979, Woolf et al 1980). Intense TENS will also activate Aβ fibres, producing segmental antinociceptive effects. As intense TENS acts in part as a counterirritant, it can be delivered for only a short time; however, it may prove useful for minor surgical procedures such as wound dressing and suture removal (Mannheimer & Lampe 1987). Despite a large published literature on TENS there is a lack of good-quality and systematic experimental work that has directly compared the clinical effectiveness and analgesic profiles of these types of TENS.
PRINCIPLES UNDERLYING APPLICATION
The patient’s report of the sensation produced by TENS is the easiest means of assessing the type of fibre activity. A strong, non-painful electrical paraesthesia is mediated by large-diameter cutaneous afferents, as intended with conventional TENS; a painful electrical paraesthesia is mediated by small-diameter cutaneous afferents, as intended by intense TENS; a strong, non-painful phasic muscle contraction is likely to excite muscle ergoreceptors, as intended by AL-TENS. Patients should be trained to titrate the amplitude, frequency and duration of pulsed currents to produce the appropriate outcome. Before patients use TENS for the first time it is important to assess their pain and to instruct them on the safe use of TENS (Box 16.1).
CONTRAINDICATIONS AND PRECAUTIONS
Contraindications
In clinical practice, healthcare practitioners have to assess the risk of using TENS against the risk associated with using other available treatments, including drug medication. TENS usually evaluates favourably. Contraindications to TENS are few and mostly hypothetical (Table 16.4). TENS manufacturers list cardiac pacemakers, pregnancy and epilepsy as contraindications. From a legal perspective it may be difficult to exclude TENS as a potential cause of a problem in these patient groups. However, it is possible to use TENS in these patients providing TENS is not applied locally and the patient’s progress is carefully monitored throughout (Watson 2006). Most importantly, the situation must been discussed with the patients physician.
| Contraindication | Advice |
|---|---|
| ‘Undiagnosed pain’ | Ensure patient has undergone assessment by a healthcare professional |
| Cardiac pacemakers | Seek approval from patient’s cardiologist Apply over chest with extreme caution; cardiologist should monitor progress frequently |
| Pregnancy | Seek approval from patient’s cardiologist, obstetrician and midwife Do not apply over anywhere over abdomen/pelvic region |
| Epilepsy | Seek approval from patient’s neurologist Do not apply on neck or head |
| Non-adherent patients | Assess patient for competency If necessary, seek approval from patient’s psychiatrist |
| Malignancy | Seek approval from patient’s palliative care specialist In general, do not apply over active malignancy |
| Cardiovascular problems | Seek approval from patient’s cardiologist Apply over chest with extreme caution; cardiologist should monitor progress frequently |
| Dermatological conditions or frail skin | Apply electrodes to healthy skin at appropriate dermatomes |
| Inappropriate electrode sites | Do not apply on anterior neck, around the eyes, overtestes, through the chest (i.e. anterior and posterior electrode positions) or over damaged skin or open wounds |
| Precaution | Advice |
| Dysaesthesia/hypoaesthesia | Assess skin sensation using sharp/blunt test prior to first TENS treatment. Apply TENS on skin with normal sensation so that patient reports presence of TENS paraesthesia. Carefully monitor to ensure TENS does not aggravate dysaesthesia |
| Allodynia/hyperalgesia | Test skin sensation prior to first TENS treatment. Apply TENS on skin with normal sensation in first instance as TENS may, but not always, exacerbate the pain |
| Contact dermatitis | Change type of electrodes – use hypoallergenic electrodes |
| Autonomic reactions to TENS | Supervise first TENS treatment and assess severity of symptoms with a view to withdrawing TENS |
| Operating hazardous equipment | Advise patients never to use TENS when driving or when using hazardous equipment |
Cardiac pacemakers
Patients with cardiac pacemakers should not use TENS unless this has been discussed with their cardiologist. This is because the electrical field generated by TENS could interfere with implanted electrical devices. Rasmussen et al (1988) found that TENS did not interfere with pacemaker performance in 51 patients. However, Pyatt et al (2003) reported that TENS did interfere with pacemaker function in a patient who had received a biventricular ICD for malignant ventricular arrhythmias and medically refractory cardiac failure. The patient experienced bradycardia and dizziness. TENS has been reported to induce artefacts on monitoring equipment (Hauptman & Raza 1992, Sliwa & Marinko 1996). Chen et al (1990) reported two cases of a Holter monitor detecting interference with a cardiac pacemaker by TENS; in both instances the sensitivity of the pacemaker was reprogrammed to resolve the problem. Careful evaluation and extended cardiac monitoring should be performed when using TENS with pacemakers.
Pregnancy
There is much debate about whether TENS should be contraindicated in pregnancy and a recent review of the subject found no reports of deleterious effects of TENS on pregnancy (Crothers 2003). TENS should not be administered over the abdomen or pelvis during pregnancy because the effects of TENS on fetal development are still unknown. TENS should not be administered over a pregnant uterus because currents could inadvertently cause uterine contractions and induce premature labour. Potential hazards when using TENS away from these sites seem minimal, although it would be wise to regularly monitor progress. It is known that obstetric TENS interferes with fetal monitoring equipment (Bundsen & Ericson 1982).
Epilepsy
Practitioners should be cautious when giving TENS to patients with epilepsy as it may be difficult to exclude TENS as a potential cause of a seizure. Rosted (2001) reported a case of repetitive epileptic seizures in a post-stroke patient using TENS. Patients are more prone to epileptic seizures following a stroke, although in this case TENS seemed to trigger the repetitive seizures. TENS should be used with caution for post-stroke pain. Scherder et al (1999) reported increased frequency of seizures when TENS was used to improve memory and behaviour in a child with a severe psychomotor disorder and epilepsy. For these reasons, TENS should not be applied on the neck or head in patients with epilepsy.
Cardiovascular problems
Therapists wishing to administer TENS to a patient with a history of cardiac disturbances, such as dysrhythmias, should always discuss the situation with a cardiologist. It is likely that TENS can be used in most cases provided it is to be applied away from the chest area. TENS is often used over the chest for angina, with much success (see the section Known efficacy: the clinical effectiveness of TENS). However, Mann (1996) reported a case of a patient who had inappropriately applied TENS electrodes on the anterior and posterior areas of the chest for unstable angina and severely compromised pulmonary ventilation owing to excessive stimulation of the intercostal muscles. The situation was resolved as soon as TENS was switched off. TENS should not be delivered through the chest using anterior and posterior electrode positions. In addition, TENS should not be applied over areas where there has been recent haemorrhage because the currents may cause further bleeding. TENS should never be applied over areas where there is ischaemic tissue and/or thrombosis, as there may be a potential for an embolism.
Dermatological conditions or frail skin
TENS electrodes should not be applied on areas of broken or damaged skin, such as open wounds, although they can be placed over healthy skin surrounding a wound. Electrodes should not be applied on frail skin (e.g. some elderly patients) or on conditions such as eczema, because they may cause skin damage on removal. TENS can be placed over healthy skin around, or proximal to, an area of eczema. TENS has been used successfully for pruritus (Hettrick et al 2004, Tang et al 1999, Tinegate & McLelland 2002, Ward et al 1996).
Precautions
Contact dermatitis
Patients may experience minor skin irritation with TENS, such as reddening beneath or around the electrodes. This is often due to dermatitis at the site of contact with the electrodes resulting from the constituents of electrodes, electrode gel or adhesive tape (Corazza et al 1999, Meuleman et al 1996). The development of hypoallergenic electrodes has markedly reduced the incidence of contact dermatitis. Patients should be encouraged to wash the skin (and electrodes when indicated by the manufacturer) after TENS and to apply electrodes to fresh skin on a daily basis. Occasionally, patients may manifest severe contact dermatitis. There are anecdotal reports (not written up in the literature) of cases where TENS has caused an allergic response, with severe redness, blotching and irritation at local and distant sites to TENS. It is difficult to confirm the validity of such reports and whether symptoms are a direct result of TENS.
ELECTRODE POSITIONS
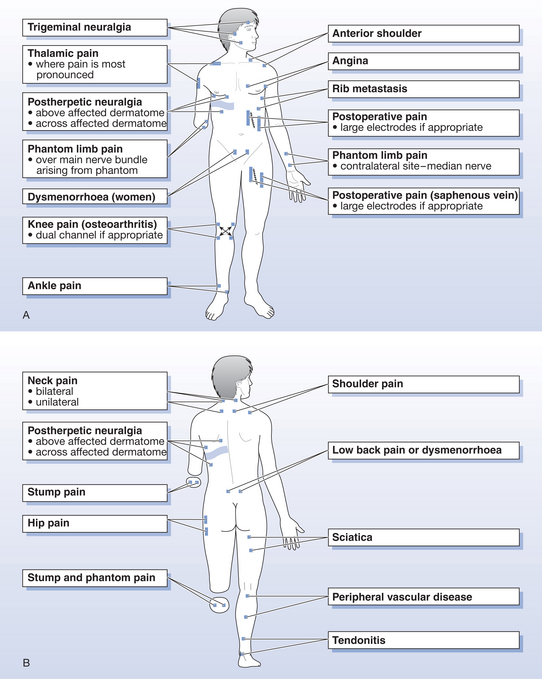
Normal skin sensation
TENS electrodes must be positioned on healthy innervated skin where sensation is intact, so it is important to check skin sensation prior to application. For most types of pain, TENS electrodes are placed around the site of pain so that paraesthesia can be directed into the painful area (Fig. 16.11). This is because conventional TENS is operating via a segmental mechanism so electrodes are placed to stimulate Aβ fibres, which enter the same spinal segment as the nociceptive fibres associated with the origin of the pain.
DUAL CHANNEL DEVICES
Dual channel devices using four electrodes or large electrodes should be used for pain covering large areas. However, if the pain is generalized and widespread over a number of body parts it may be more appropriate to use AL-TENS at the relevant myotome, as this may produce a more generalized analgesic effect (Johnson 1998). Dual channel stimulators are useful for patients with multiple pains such as low back pain and sciatica, or for pains which change in their location and quality over a short time period, e.g. during childbirth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree