Electrodiagnostic Approach to Patients with Suspected Radiculopathy
Timothy R. Dillingham
Introduction
Cervical and lumbosacral radiculopathies are conditions involving a pathologic process affecting the spinal nerve root. Commonly, this is a herniated nucleus pulposus that anatomically compresses a nerve root within the spinal canal. Another common etiology for radiculopathy is spinal stenosis resulting from a combination of degenerative spondylosis, ligament hypertrophy, and spondylolisthesis. Inflammatory radiculitis is another pathophysiologic process that can cause radiculopathy. It is important to remember, however, that other more ominous processes such as malignancy and infection can manifest the same symptoms and signs of radiculopathy as the more common causes.
This chapter deals with the clinical approach used in an electrodiagnostic laboratory to evaluate a person with neck pain, lumbar spine pain, or limb symptoms suggestive of radiculopathy. The indications for referring for testing as well as the limitations of testing are discussed to give a greater understanding of this important diagnostic procedure.
Given the large differential diagnosis for limb and spine symptoms, it is important for electrodiagnosticians to develop a conceptual framework for evaluating these referrals with a standard focused history and physical examination and a tailored electrodiagnostic approach. Accurately identifying radiculopathy by means of electrodiagnosis provides valuable information that informs planning of treatment and minimizes other invasive and expensive diagnostic and therapeutic procedures.
Spine and Nerve Root Anatomy: Deviations from the Expected
Spinal anatomy is discussed in Chapter 1 in greater detail. From an electrodiagnostic perspective, however, there are several specific anatomic issues that merit further discussion.
At all levels the dorsal root ganglion lies in the intervertebral foramen. This anatomic ar- rangement has implications for clinical electrodiagnosis of radiculopathy, namely that sensory nerve action potentials (SNAPs) are preserved in most radiculopathies as the nerve root is affected proximal to the DRG.
Regarding the cervical nerve roots and the brachial plexus, there are many anatomic variations. Perneczky (1) described an anatomic study of 40 cadavers. In all cases, there were deviations from accepted cervical root and brachial plexus anatomy. Levin et al (2) examined the pattern of abnormalities on electromyography (EMG) in 50 cases of surgically proven cervical root lesions. A range of needle EMG patterns was found, with EMG demonstrating less specificity for the C6 root level but more specificity and consistent patterns for C8, C7, and C5 radiculopathies. In
subjects with C6 radiculopathy, half of the patients showed findings similar to those with C5 radiculopathy and the other half demonstrated C7 patterns. This surgical group was more severely affected than patients who did not require surgical interventions, and this pattern may not hold for less symptomatic patients.
subjects with C6 radiculopathy, half of the patients showed findings similar to those with C5 radiculopathy and the other half demonstrated C7 patterns. This surgical group was more severely affected than patients who did not require surgical interventions, and this pattern may not hold for less symptomatic patients.
In the lumbar spine the dorsal and ventral lumbar roots exit the spinal cord at about the T11–L1 boney levels and travel in the lumbar canal as a group of nerve roots in the dural sac. This is termed the “horse’s tail” or cauda equina. This poses challenges and limitations to the EMG examination. A destructive intramedullary spinal cord lesion at the T11 vertebral level that damages the anterior horn cells can produce EMG findings in muscles innervated by any of the lumbosacral nerve roots and manifest precisely the same findings on needle EMG as those seen with a herniated nucleus pulposus at any of the lumbar disc levels. Likewise, an L2 skeletal level lesion can affect any of the cauda equina roots. For this reason, the electromyographer cannot determine for certain the anatomic location of the lumbar intraspinal lesion producing distal muscle EMG findings in the lower limbs. The needle EMG examination can identify the root or roots that are physiologically involved, but not the precise anatomic site of pathology in the lumbar spinal canal. This is an important limitation requiring correlation with imaging findings to determine which of the possible anatomic locations is most likely the offending site. This can be difficult in elderly persons with foraminal stenosis as well as moderate central spinal canal stenosis at a more proximal site.
In a prospective study of 100 patients with lumbosacral radiculopathy who underwent lumbar laminectomy, EMG precisely identified the involved root level 84% of the time (3). Needle EMG failed to accurately identify the compressed root in 16%. However, at least half of the failures were attributable to anomalies of innervation. Another component of this study involved intraoperative stimulation of the nerve roots with simultaneous recording of muscle activity in the lower limb using surface electrodes. These investigators demonstrated variations in root innervations, such as the L5 root innervating the soleus and medial gastrocnemius, in 16% of a sample of 50 patients. Most subjects demonstrated dual innervations for most muscles (3).
These findings underscore the limitations of precise localization for root lesions by EMG. The electrodiagnostician should maintain an appreciation of these anatomic variations to better convey the level of certainty with respect to diagnostic conclusions.
Physical Examination
The electrodiagnostic examination is an extension of the standard clinical examination. The history and physical examination are vital initial steps in determining what conditions may be causing the patient’s symptoms. Most radiculopathies present with symptoms in one limb. Multiple radiculopathies, such as are seen in cervical spinal stenosis or lumbar stenosis, may cause symptoms in more than one limb. A focused neuromuscular examination that assesses muscle strength, reflexes, and sensation in both the affected limb and the contralateral limb is important, providing a conceptual framework for electrodiagnostic assessment.
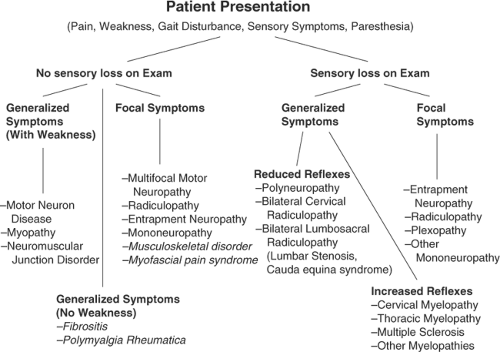
An algorithmic approach to using physical examination and symptom information to tailor the electrodiagnostic evaluation is shown in Figure 12-1. In this approach, the patient’s symptoms and physical examination signs of sensory loss and weakness create a conceptual framework for approaching these sometimes daunting problems. Admittedly, there are many exceptions to this approach, with considerable overlap in conditions that might fall within multiple categories. Radiculopathies and entrapment neuropathies are examples of such conditions with a variety of clinical presentations and physical examination findings, such that they are included in both focal symptom categories with and without sensory loss. In the case of a person with lumbosacral radiculopathy, a positive straight-leg raise test may be noted in the absence of motor, reflex, or sensory changes. Conditions such as myopathies and polyneuropathies better fit this algorithmic approach, given that symptoms and physical examination signs are more specific. Figure 12-1 also contains musculoskeletal disorders and denotes how they fall into this conceptual framework. The electrodiagnostician
must be able to modify the electrodiagnostic examination in response to nerve conduction and EMG findings and adjust the focus of the examination in light of new information.
must be able to modify the electrodiagnostic examination in response to nerve conduction and EMG findings and adjust the focus of the examination in light of new information.
The implications of symptoms and signs on electrodiagnostic findings were investigated by Lauder et al for both suspected cervical and lumbosacral radiculopathies (4,5). Even though physical examination findings were better at predicting who would have a radiculopathy, many patients (18% in the lower limb) with normal examinations had abnormal lower limb electrodiagnostic studies, indicating that clinicians should not curtail electrodiagnostic testing simply because the physical examination is normal. For lower limb symptoms, loss of a reflex or weakness dramatically increased the likelihood of having a radiculopathy by EMG. Losing the Achilles reflex, for instance, resulted in an odds ratio of 8.4 (P <0.01)—in other words, eight times the likelihood of having a radiculopathy by EMG with this physical examination finding (4). Similar findings were noted for upper limb symptoms. If a reflex was lost or weakness was noted, the likelihood of having a cervical radiculopathy confirmed by EMG was many times greater (5). Combinations of findings, particularly weakness plus sensory loss or weakness plus reflex changes, resulted in ninefold greater likelihood of cervical radiculopathy and two to three times greater likelihood of lumbosacral radiculopathy (4,5).
Electrodiagnostic Testing
Electrodiagnostic testing is expensive and uncomfortable for patients, and so it is important to understand why it is performed and the expected
outcomes. Electrodiagnostic testing serves several important purposes:
outcomes. Electrodiagnostic testing serves several important purposes:
It effectively excludes other conditions that mimic radiculopathy, such as polyneuropathy or entrapment neuropathy. Haig et al (6) demonstrated that the referring diagnostic impression is often altered with electrodiagnostic testing
Electrodiagnostic testing can to some extent suggest severity or extent of the disorder beyond the clinical symptoms. Involvement of other extremities can be delineated or the involvement of multiple roots may be demonstrated, such as in the case of lumbosacral spinal stenosis.
There is utility in solidifying a diagnosis. An unequivocal radiculopathy on EMG in an elderly patient with nonspecific or mild lumbar spondylosis or stenosis on MRI reduces diagnostic uncertainty and identifies avenues of management such as lumbar steroid injections or decompression surgery in certain situations.
Outcome prediction may be possible. If surgical intervention is planned for a lumbosacral radiculopathy, a positive preoperative EMG improves the likelihood of a successful outcome postoperatively (see “Implications of an EMG-Confirmed Radiculopathy”). This is an area that deserves more research attention.
Usefulness of Electrodiagnostic Testing
The value of any test depends upon the a priori certainty of the diagnosis in question, and this principle applies to electrodiagnostic testing. For a condition or diagnosis for which there is great certainty before additional testing, the results of the subsequent tests are of limited value. The concept of diminishing returns on the road to diagnostic certainty is an important one. For instance, an EMG test will be of limited value in confirming the diagnosis of radiculopathy in a patient with acute-onset sciatica while lifting, L5 muscle weakness, a positive straight-leg raise, and an MRI showing a large extruded L4-5 nucleus pulposus. This is because the a priori certainty of the diagnosis was very high. In contrast, an elderly diabetic patient with sciatica, limited physical examination findings, and equivocal or age-related MRI changes presents an unclear picture. In this latter case the electrodiagnostic testing is of high value, placing in perspective the imaging findings and also excluding diabetic polyneuropathy or plexopathy as confounding conditions.
Aanem Guidelines for Radiculopathy Evaluation
The American Association of Neuromuscular and Electrodiagnostic Medicine (AANEM, formerly AAEM) guidelines recommend that for an optimal evaluation of a patient with suspected radiculopathy, a needle EMG screen of a sufficient number of muscles and at least one motor and one sensory nerve conduction study should be performed in the involved limb (7). The nerve conduction studies are necessary to exclude polyneuropathy. The sufficiency of the EMG screen and a recommended number of muscles is discussed in detail below. An EMG study is considered diagnostic for a radiculopathy if EMG abnormalities are found in two or more muscles innervated by the same nerve root and different peripheral nerves, yet muscles innervated by adjacent nerve roots are normal (8). This assumes, of course, that other generalized conditions such as polyneuropathy are not present.
EMG study of bilateral limbs is often necessary, particularly if a single limb shows EMG findings suggestive of radiculopathy and the patient has symptoms in both the studied and the contralateral limb. If bilateral limbs are involved, then the electrodiagnostician should proceed by studying selected muscles in an upper limb (if the lower limbs are abnormal on EMG) or a lower limb (if both upper limbs are abnormal) to exclude a generalized process such as polyneuropathy or motor neuron disease. Likewise, additional nerve conduction studies are appropriate to exclude other suspected conditions, and the electrodiagnostician should have a low threshold for expanding the study.
H Reflex
H reflexes have commonly been used to determine whether a radiculopathy demonstrates S1 involvement (8). This is a monosynaptic reflex that is an S1 nerve root-mediated response and can
differentiate to some extent L5 from S1 radiculopathy. Many researchers have evaluated the sensitivity and specificity of the H reflex with respect to lumbosacral radiculopathies and generally found a range of sensitivities from 32% to 88% (8,9,10,11,12,13). However, many of these studies suffered from lack of a control group, imprecise inclusion criteria, or small sample sizes.
differentiate to some extent L5 from S1 radiculopathy. Many researchers have evaluated the sensitivity and specificity of the H reflex with respect to lumbosacral radiculopathies and generally found a range of sensitivities from 32% to 88% (8,9,10,11,12,13). However, many of these studies suffered from lack of a control group, imprecise inclusion criteria, or small sample sizes.
Marin et al (13) prospectively examined the H reflex and the extensor digitorum brevis muscle stretch reflex in 53 normal subjects, 17 patients with L5, and 18 patients with S1 radiculopathy. Patients in the study had all of the following: low back pain radiating to the leg; reduced sensation, weakness, or positive straight leg raise test; and either EMG evidence of radiculopathy or structural changes on MRI or CT. The H reflex maximal side-to-side latency difference was 1.8 ms, as derived from the normal group. They analyzed the sensitivity of the H reflex for side-to-side differences greater than 1.8 ms or a unilaterally absent H reflex on the affected side. The H reflex demonstrated only 50% sensitivity for S1 radiculopathy and 6% for L5 radiculopathy but had 91% specificity. H reflex amplitudes were not assessed in this study. These results suggest that the H reflex has a low sensitivity for S1 root level involvement but may help differentiate L5 from S1 root involvement.
H reflexes may be useful to identify subtle S1 radiculopathy, yet there are a number of shortcomings related to these responses. They can be normal with radiculopathy (13), and because they are mediated over such a long physiologic pathway, they can be abnormal due to polyneuropathy, sciatic neuropathy, or plexopathy (8). They are most useful in the assessment for polyneuropathy.
To interpret a latency or amplitude value, and to render a judgment as to the probability that it is abnormal, precise population-based normative values encompassing a large range of ages of normal subjects must be available to which to compare these nerve conduction findings. Falco et al (14) demonstrated in a group of healthy elderly subjects (60 to 88 years old) that the tibial H reflex was present and recorded bilaterally in 92%. Most elderly persons are expected to have normal H reflex studies, and when abnormalities are found in these persons, the electrodiagnostician should critically evaluate these findings and the clinical scenario before attributing H reflex abnormalities to the aging process.
In patients with upper limb symptoms suggestive of cervical radiculopathy, H reflexes and F waves are not useful in diagnosis but rather help exclude polyneuropathy as an underlying cause of symptoms. One study by Miller et al (15) examined the H reflexes in the upper limb in a set of patients defined by a combination of clinical criteria (no imaging or EMG studies, however) as having definite or probable cervical radiculopathy. They tested the H reflex for the flexor carpi radialis, extensor carpi radialis, and abductor pollicis brevis muscles and also evaluated the biceps brachii heteronymous reflex. The later reflex is derived by stimulating the median nerve in the cubital fossa and recording over the biceps brachii muscle, averaging 40 to 100 trials. These reflex studies had a 72% sensitivity overall for the group, with 100% for the subset of patients with definite cervical radiculopathy. In contrast, needle EMG demonstrated 90% sensitivity for the definite group. Although these findings suggest a possible role for these upper limb H reflexes, they are highly specialized, time consuming, and difficult to consistently elicit. They may have a role in sensory radiculopathies where needle EMG will not be positive and imaging findings are equivocal. Further studies are necessary to clarify whether these findings of Miller et al (15) can be duplicated in other centers.
F Wave
F waves are late responses involving the motor axons and axonal pool at the spinal cord level. They can be assessed and classified by using the minimal latency, mean latency, and chronodispersion or scatter (8). As in the case of H reflexes, F waves demonstrate low sensitivities and are not specific for radiculopathy; rather, they are a better test to screen for polyneuropathy. Published sensitivities in radiculopathies range from 13% to 69%, but these studies suffer from many of the shortcomings that are found in the H reflex studies (9,16,17).
London and England (18) reported two cases of persons with neurogenic claudication from lumbosacral spinal stenosis. They demonstrated that the F wave responses could be reversibly
changed after 15 minutes of ambulation that provoked symptoms. This suggested an ischemia-induced conduction block in proximal motor neurons. A larger-scale study of this type might find a use for F waves in the identification of lumbosacral spinal stenosis and assist with the delineation of neurogenic from vascular claudication.
changed after 15 minutes of ambulation that provoked symptoms. This suggested an ischemia-induced conduction block in proximal motor neurons. A larger-scale study of this type might find a use for F waves in the identification of lumbosacral spinal stenosis and assist with the delineation of neurogenic from vascular claudication.
Motor and Sensory Nerve Conduction Studies
Standard motor and sensory nerve conduction studies are not helpful in identifying a cervical or lumbosacral radiculopathy; however, they should be performed to screen for polyneuropathy and to exclude common entrapment neuropathies if the patient’s symptoms could be explained by a focal entrapment. It is important to remember that based upon the anatomy of the dorsal root ganglion, sensory responses should be normal in most radiculopathies. If they are found to be absent, this should increase suspicion for another diagnosis, such as polyneuropathy or plexopathy.
Plexopathies often pose a diagnostic challenge, as they are similar to radiculopathies in symptoms and signs. To distinguish plexopathy from radiculopathy, sensory nerve conduction test responses that are accessible in a limb should be tested. In plexopathy, they are likely to be reduced in amplitude, whereas in radiculopathy they are generally normal. If substantial axonal loss has occurred at the root level, the compound muscle action potential recorded in muscles innervated by that root may be reduced in both plexopathies and radiculopathies. This is usually when severe axonal loss has occurred, such as with cauda equina lesions or penetrating trauma that severely injures a nerve root. The distal motor latencies and conduction velocities are usually preserved as they reflect the fastest-conducting nerve fibers (8).
Somatosensory Evoked Potentials and Related Tests
The AANEM guidelines recently examined the literature and concluded that somatosensory evoked potentials (SEPs) may be useful for cervical spondylosis with cord compression. Likewise, in lumbosacral spinal stenosis, dermatomal SEPs (DSEPs) may be useful in defining levels of deficits (7). These tests are not necessary for electrodiagnostic testing for persons with suspected radiculopathies, and their usefulness is limited to special circumstances.
DSEPs can document physiologic evidence of multiple- or single-root involvement in lumbosacral spinal stenosis and may be useful in the case where spinal canal narrowing is minimal and the patient has symptoms. This testing also complements standard needle EMG. Snowden et al (19) found that for single-level and multilevel lumbosacral spinal stenosis, DSEPs revealed 78% sensitivity relative to spinal imaging. In this well-designed prospective study, DSEP criteria as well as inclusion criteria were precisely defined. The predictive value was 93%. Yiannikas (20) demonstrated that SEPs may be useful for cervical myelopathy. In a study of patients with clinical signs of myelopathy, all 10 had abnormal peroneal SEPs, and 7 had abnormal median SEPs.
Maertens de Noordhout et al (21) examined motor evoked potentials (MEPs) and SEPs in 55 persons with unequivocal signs and symptoms of cervical spinal cord myelopathy. In this group, 87% showed gait disturbances and 82% showed hyperreflexia. MRI was not the diagnostic standard, as these authors felt that MRI was prone to overdiagnosis; rather, metrizamide myelography showed unequivocal signs of cervical cord compression for all of these patients. Magnetic stimulation of the cortex was performed and the responses were measured with surface electrodes over limb muscles. In these subjects, 89% demonstrated abnormalities in MEP to the first dorsal interosseus muscle, and 93% had one MEP abnormality. At least one SEP abnormality was noted in 73%.
Tavy et al (22) examined whether MEPs or SEPs assisted in identifying persons with radiologic evidence of cervical cord compression but who were without clinical markers for myelopathy. All patients had clinical symptoms of cervical radiculopathy, but not myelopathy. In this group, MEPs were normal in 92% and SEPs were normal in 96%. These investigators concluded that MEPs and SEPs are normal in most cases of persons with asymptomatic cervical stenosis. This indicates that abnormal MEPs and SEPs are likely to be true-positive findings and not false-positives related to mild cord compression that does not cause symptoms. It is important to remember that cervical
spondylosis is a process that causes a continuum of problems, including both radiculopathy and myelopathy.
spondylosis is a process that causes a continuum of problems, including both radiculopathy and myelopathy.
The inherent variability in SEP recordings and difficulty in determinations as to what constitutes “normal” prompted investigation. Dumitru et al (23) examined the variations in latencies with SEPs. In 29 normal subjects, they examined the ipsilateral intertrial variations, arithmetic mean side-to-side differences, and maximum potential side-to-side differences with stimulation of the superficial peroneal sensory nerve, sural nerve, and the L5 and S1 dermatomes with respect to P1 and N1 latencies and peak-to-peak amplitudes. Considerable ipsilateral intertrial variation was observed, and side-to-side comparisons revealed a further increase in this inherent variation regarding the above-measured parameters. They suggested an additional parameter with which to evaluate SEPs: the maximum side-to-side latency difference.
Dumitru et al (24), in a later study involving persons with unilateral and unilevel L5 and S1 radiculopathies, evaluated dermatomal and segmental SEPs. History, physical examination, imaging studies, and electrodiagnostic medicine evaluations clearly defined patients with isolated L5 or S1 nerve root compromise. Regression equation analysis for cortical P1 latencies evaluating age and height based on comparable patient and control reference populations revealed segmental and dermatomal sensitivities for L5 radiculopathies to be 70% and 50%, respectively, at 90% confidence intervals. Similar sensitivities were obtained for cortical P1 latencies using the mean ± 2 standard deviations (SD) method. Side-to-side cortical P1 latency difference data revealed SEP and DSEP sensitivities for S1 radiculopathies to be 50% and 10%, respectively, also at 2 SD. These investigators questioned the clinical utility of both segmental and dermatomal SEPs in the evaluation of patients with suspected focal L5 or S1 nerve root compromise, finding little utility for these tests in persons with single-level lumbosacral radiculopathy.
In summary, SEPs, DSEPs, and MEPs are not necessary or recommended for the vast majority of patients referred for possible cervical or lumbosacral radiculopathy (7). They can be helpful if performed in special laboratories skilled in such testing, with adequate normal values, and in certain clinical situations that can be clarified by such results.
Needle Electromyography
The need for EMG, particularly in relationship to imaging of the spine, has been recently highlighted (25). Needle EMG is particularly helpful in view of the fact that the false-positive rates for MRI of the lumbar spine are high, with 27% of healthy subjects having a disc protrusion (26). For the cervical spine the false-positive rate for MRI is much lower, with 19% of subjects demonstrating an abnormality, but only 10% showing a herniated or bulging disc (27). Radiculopathies can occur without structural findings on MRI, and likewise without EMG findings. The EMG evaluates only motor axonal loss or motor axon conduction block, and for these reasons a radiculopathy affecting the sensory root will not yield abnormalities by EMG. If the rate of denervation is balanced by reinnervation in the muscle, then spontaneous activity is less likely to occur and be identified with needle EMG.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree