
Endovascular Treatment of Dural Arteriovenous Fistulas
Objectives: Upon completion of this chapter, the reader should be able to identify the transarterial and transvenous embolization techniques that can be used to treat dural arteriovenous fistulas at various intracranial and spinal locations.
Accreditation: The AANS* is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to sponsor continuing medical education for physicians.
Credit: The AANS designates this educational activity for a maximum of 15 credits in Category 1 credit toward the AMA Physician’s Recognition Award. Each physician should claim only those hours of credit that he/she spent in the educational activity.
The Home Study Examination is online on the AANS Web site at: http://www.aans.org/education/books/controversy.asp
* The acronym AANS refers to both the American Association of Neurological Surgeons and the American Association of Neurosurgeons.
 General Considerations
General Considerations
Dural arteriovenous fistulas (DAVFs) are arteriovenous shunts supplied by dural feeding arteries and usually occur within or near the dural sinuses in various locations. They can secondarily recruit pial or transosseous cutaneous feeders. Most adult lesions are considered as acquired, and the most well-accepted triggering factor for development is sinus thrombosis, which can be idiopathic or due to trauma, tumor,1 surgery, infection, or hypercoagulability secondary to hormonal influence.2–5 Angiography for these lesions frequently shows evidence of partial or complete sinus thrombosis with various degrees of outflow restriction of the venous drainage of the normal brain or the fistulas themselves. However, the inciting factor leading to the development of DAVFs is frequently undetected, suggesting that other unidentified factors must be present.
Dural arteriovenous fistulas can present with a variety of symptoms, which are mostly related to the direction of the abnormal venous drainage and disturbance of normal venous drainage of the brain, spinal cord, or orbit.6 Cognard et al and Borden et al proposed classifications of DAVFs based on venous drainage. Borden et al classified DAVFs into three types. Type I DAVFs drain into the dural sinus in an antegrade fashion. Type II DAVFs drain into the venous sinus with retrograde drainage into subarachnoid veins. Type III DAVFs drain into the subarachnoid veins.7 Cognard et al proposed a similar but more detailed classification. They classified DAVFs into five types: type I, located in the main sinus with antegrade flow; type II, in the main sinus with reflux into the sinus (IIa), cortical vein (IIb), or both (IIa+b); type III, with direct cortical venous drainage without venous ectasia; type IV, with direct cortical venous drainage with venous ectasia; and type V, with spinal venous drainage.8 These classifications correlate well with clinical symptomatology and prognosis.9
Venous hypertension is the most important etiologic factor and can be focal or global. Focal venous hypertension can develop due to primary pial (cortical or perimedullary) venous drainage of the fistula10 or secondary reflux to pial veins from the sinus due to sinus outflow restriction. Venous hypertension can cause venous rupture at any point of the cortical venous drainage resulting in intracerebral or subarachnoid hemorrhage, seizures, venous infarcts, or focal neurological deficits due to venous ischemia. Focal ectasia and stenosis of draining veins are the frequent findings in those cases presenting with hemorrhage and commonly seen in the tentorial-incisural, or anterior cranial fossa DAVFs. Spinal cord venous hypertension due to perimedullary venous drainage in posterior fossa DAVFs or spinal DAVFs can cause progressive myelopathy. Orbital signs and congestion associated with cavernous sinus DAVFs are attributed to focal venous hypertension of the ophthalmic venous system. Global venous hypertension can also occur due to functional outflow restriction of the venous drainage of the entire brain secondary to the arteriovenous (AV) shunting and dural sinus thrombosis or maldevelopment of the normal venous system. It can cause dementia or decreased mental activities and papilledema due to increased intracranial pressure. 6,9,11,12–14 This type of global cerebral dysfunction and papilledema can be reversible by closing the fistulas with preservation of the patency of the deep venous system.3
Other mechanisms of a functional disturbance in the venous system include venous mass effect, which can cause cranial neuropathy or optic neuropathy, and thrombosis such as of the ophthalmic vein, which causes retinal and choroidal hemorrhage and dysfunction, and sudden proptosis in cases with cavernous sinus DAVFs.15 Pulsatile tinnitus is another symptom due to high-flow venous drainage conducting to the auditory apparatus. A disturbance in the arterial circulation can rarely cause symptoms; Lasjaunias described cranial nerve palsy that developed from a possible arterial steal phenomenon.6
The prognosis of untreated DAVFs is poor if there is primary or secondary pial venous drainage but is usually benign if there is only drainage into the dural sinus without pial venous reflux16–18 The spinal DAVFs usually have a poor prognosis due to progressive myelopathy if they are not treated.19 It is important to recognize that DAVFs are a dynamic disease and the direction of evolution is unpredictable. They can increase or decrease in flow or even disappear depending on the location; or they may reroute their venous drainage due to progression of venous or sinus thrombosis. Although the disappearance of cranial bruit or symptoms may indicate favorable spontaneous thrombosis of the AV shunting, it can also reflect further thrombosis of the sinus with development of pial venous drainage, which places the patient at risk for hemorrhage, cerebral infarcts, and seizures.18,20 Changes in the symptoms, therefore, should be carefully evaluated with contrast magnetic resonance imaging (MRI) and, if necessary, with angiography for development of pial venous drainage.19
Although the classification of DAVFs based on venous drainage correlates well with the symptomatology, for consideration of treatment strategies, a classification based on the location of the lesion is preferred and facilitates comparison between surgical and endovascular approaches. We discuss angiographic features, symptomatology, indications, and techniques for endovascular treatment of DAVFs. Pediatric and spinal DAVFs are discussed separately, because they have distinct angiographic features, natural history, and treatment methods from adult intracranial DAVFs.
Pretherapeutic angiographic evaluation should address the location of the AV shunts, arterial supply, flow characteristics through the fistula, venous drainage, and existence and extent of thrombosis of cortical veins or dural sinuses, as well as the drainage of the normal brain. Evaluation of the venous phase of the cerebral circulation before and after endovascular treatment is especially important to assess the etiology of the symptoms and clinical findings and to predict their improvement after treatment.
Endovascular treatment for DAVFs can be performed by transarterial, transvenous, or a combined approach. For transarterial embolization, liquid embolic agents such as n-butyl cyanoacrylate (NBCA) are the most effective in penetrating to the fistula site and permanently occluding the shunt. For optimal transarterial embolization using a liquid agent, the tip of the microcatheter has to be wedged into the feeder beyond the supply to the normal tissue to obtain flow control and penetration of the agent into the venous side.21 Particulate agents such as polyvinyl alcohol (PVA) tend to result in proximal occlusion and recanalization of the fistulas either by collateral vessels to the fistula sites or recanalization of the embolized vessel itself.22 In general, particulate agents are a less-definite material but can be used for palliative embolization or if distal catheterization adequate for liquid agents is not possible. A cautionary comment for arterial embolization concerns the use of coils. It is important not to place coils in the proximal portion of the arterial feeders because it is rarely curative; it excludes the future transarterial access and facilitates development of inaccessible collateral supply to the fistulas. Coils in the arterial route are only used to protect normal vessels prior to liquid embolization.22 For transvenous embolization, coils are generally used to occlude the venous side of the fistulas. If the internal jugular vein is not available for the transvenous embolization of a sinus, transcranial approach to the sinus may be possible.23 It is important to evaluate the feasibility of the occlusion of the affected portion of the sinus on the pretherapeutic angiogram. If there is venous drainage of the normal brain to the sinus, that segment of the sinus should not be occluded. Transvenous coil embolization is occasionally possible without occlusion of the sinus if the DAVF drains into a venous lake that is separated from the sinus.24
Conventional radiotherapy for DAVFs was reported with some success before the development of endovascular embolization and refined surgical techniques. Radiosurgery for selected DAVFs has been recently reported with or without combination with transarterial embolization25–28; however, we have no experience with radiosurgery and thus are not discussing it in this review.
 Transverse-Sigmoid Dural Arteriovenous Fistulas
Transverse-Sigmoid Dural Arteriovenous Fistulas
Transverse-sigmoid sinus region DAVFs are the most common type of DAVFs found in Western countries. They are supplied by multiple dural branches to the transverse and sigmoid sinuses from the external carotid, internal carotid, and vertebral arteries. Venous outflow restriction due to thrombosis of the sigmoid or transverse sinus is common and results in cortical venous drainage that can cause hemorrhage,29 seizure, or venous infarction.30 If there is no cortical venous drainage, patients usually present with only bruit, which is the most common symptom. Spontaneous thrombosis of the fistulas in this location has not been documented.
The existence of cortical venous drainage is an absolute indication for treatment even for asymptomatic patients, because the natural history is poor if untreated. If bruit is the only symptom for those who do not have cortical venous drainage, the indication for treatment is relative. In this situation, the treatment plan can be chosen from conservative observation, partial treatment with preservation of the sinus patency, or complete obliteration with occlusion of the draining sinus. This decision should be made depending on the patient’s age, tolerability for bruit, and reliability of the patient for follow-up visits. For those patients who tolerate the noise and have no cortical venous drainage, we favor conservative observation. If treatment is demanded by the patient because of intolerance of bruit, the patient should be treated without sinus occlusion even if the treatment results in only partial obliteration of the fistulas. Once conservative observation is chosen, the patient should be closely monitored with periodic clinical examination and contrast-enhanced MRI. If there is MRI evidence of initiation or progression of sinus thrombosis and development of cortical venous drainage, the patient should undergo cerebral angiography. If cortical venous drainage is confirmed by angiography, the patient should be treated prior to the development of hemorrhage or neurological symptoms.
Embolization is the premier mode of treatment and can be performed by transarterial, transvenous, or a combined approach with a high rate of total obliteration of the DAVFs. Transarterial embolization is favored for small lesions because patency of the sinus can be preserved. This approach is also the first choice and is frequently curative for those lesions draining to the isolated sinus with cortical venous drainage due to sinus thrombosis proximal and distal to the fistula site (Fig. 16-1). For extensive lesions with multiple feeders and multiple fistula sites, a transvenous or a combined approach is favored because complete cure is difficult by transarterial embolization alone.31,32 If transvenous embolization is considered for complete obliteration of the fistulas, it is essential to identify and avoid occlusion of the junction between the vein of Labbé and the transverse sinus. It is also important to preserve the venous drainage of the cerebellum to the sinus (Fig. 16-2), which is especially relevant when occlusion of a long segment of the sinus or medial transverse sinus is planned. Once feasibility of sinus occlusion is confirmed, the technique for sinus obliteration is relatively simple. Even if the distal sinus is not opacified on the angiographic study, it is usually possible to reach the fistula site either through the contralateral sinus or through the nonopacified or thrombosed segment of the sinus with gentle guidewire and catheter manipulation.33 If sinus occlusion is not feasible, a combined approach with transvenous occlusion of the feasible part of the sinus and transarterial embolization for the remaining fistulas is considered. Recanalization of the occluded sinus with stenting to redirect the venous drainage from cortical veins to the sinus combined with additional transarterial embolization to decrease the shunt is theoretically a reasonable option.34 However, long-term patency of the recanalized sinus is currently not known.
Good results can be usually obtained by endovascular treatment for DAVFs in this location; therefore, the indications for surgery have become limited to only exceptional cases in which both transarterial and transvenous approaches are not feasible or failed.
 Cavernous Dural Arteriovenous Fistulas
Cavernous Dural Arteriovenous Fistulas
Dural arteriovenous fistulas involving the cavernous sinus are characterized by wide variation in their angioarchitecture, which is reflected in the variety of clinical symptoms and findings and also influences treatment strategies. Fistula sites can be at the dural membrane of one (Fig. 16-3) or both cavernous sinuses (Fig. 16-4). Unilateral fistulas can receive unilateral or bilateral supply from dural branches of the ICA or ECA and can drain either unilaterally or bilaterally.35 The pattern of venous drainage can be anterior to the ophthalmic venous system, posterior to the superior or inferior petrosal sinus, lateral and superior to the sylvian vein, inferior through the foramen ovale to the pterygoid plexus, medial through the coronary sinuses to the opposite cavernous sinus, or in more than one direction and pattern. Bilateral fistulas have a higher incidence of cortical venous drainage as compared with unilateral shunts. Thrombosis of some draining veins is a frequent observation, and the symptoms and clinical findings are closely related to the pattern of venous drainage. The anterior venous drainage to the ophthalmic vein causes exophthalmos, chemosis, conjunctival injection, restricted extraocular muscular movements, increased intraocular pressure, and visual loss from optic nerve or retinal/ choroidal dysfunction, or even hemorrhages.18,29,36 An acute exacerbation of eye and orbital problems can occur spontaneously or after treatment. This is usually due to progressive thrombosis of the ophthalmic venous system or anterior cavernous sinus that causes increased orbital congestion and intraocular pressure.37,38 This condition is usually self-limited if the DAVF is closed, but supportive measures may be necessary to preserve vision. In the case of spontaneous exacerbation, emergent angiography should be performed with intent to embolize if there are any remaining fistulas, to decrease the venous hypertension. The postero-inferior drainage causes cranial nerve paralysis39,40 and pulsatile tinnitus. Although the cortical venous drainage can potentially cause intracranial hemorrhage, seizure, or neurological deficits due to focal venous hypertension of the brain, they are unusual for cavernous DAVFs, probably because of multiple drainage pathways of the cavernous sinus.
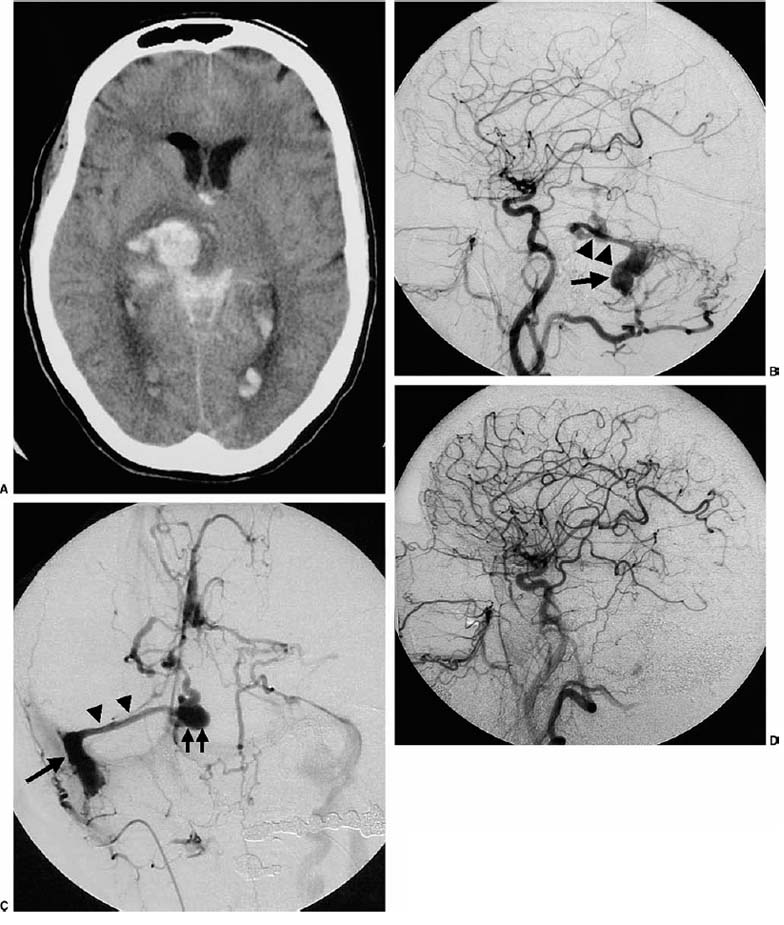
FIGURE 16-1 A 59-year-old woman presented with right cerebellar hematoma and subarachnoid hemorrhage. On the next day, the patient experienced another intracerebral hematoma in the right thalamus. (A) A noncontrast computerized tomography (CT) image after the second hemorrhage shows a right thalamic hematoma. (B) A lateral view of the right common carotid angiogram demonstrates dural arteriovenous fistulas (DAVFs) to the isolated right sigmoid sinus (arrow) draining predominantly to the superior petrosal sinus (arrowheads) with reflux to the cortical veins. (C) An anteroposterior view of the late-arterial phase of the right occipital angiogram demonstrates DAVFs to the isolated sigmoid sinus (arrow) refluxing to the superior petrosal sinus (arrowheads), then to the multiple cortical veins. There is a venous ectasia (two arrows) at the junction between the superior petrosal sinus and the perimesencephalic vein, indicating venous outflow restriction. (D) A lateral view of the right common carotid angiogram after two transarterial embolizations demonstrates complete occlusion of the DAVFs. The patient had no further hemorrhage.
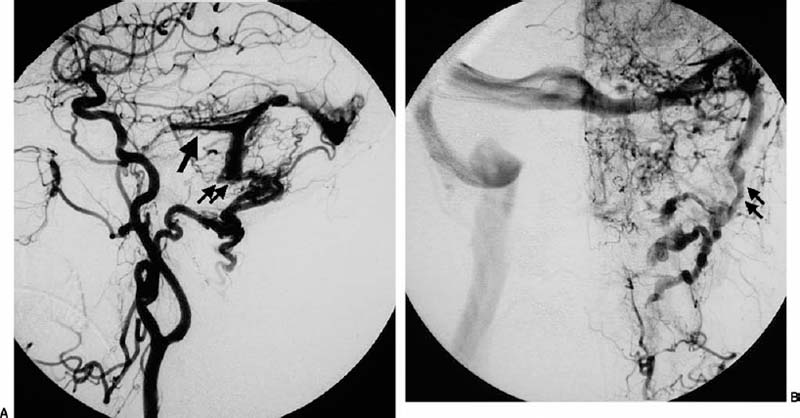
FIGURE 16-2 A 67-year-old woman presented with a 1-year history of headaches and pulsatile bruit. (A) A lateral view of the left common carotid angiogram shows the left sigmoid sinus dural arteriovenous fistulas supplied by transmastoid branches of the occipital artery, middle meningeal artery, posterior auricular artery, and the basal tentorial artery from the internal carotid artery. The venous drainage is through the opposite transverse and sigmoid sinuses as well as reflux to the left superior petrosal sinus (arrow) and cortical veins on the surface of the temporal lobe and cerebellar hemisphere. The left sigmoid sinus is occluded (two arrows). (B) An anteroposterior view of the left common carotid angiogram shows evidence of venous hypertension of the left cerebellar hemisphere and the occipitotemporal lobe. The left sigmoid sinus is occluded (two arrows) with collateral venous drainage to the paravertebral veins.
The first choice of treatment is embolization by a transarterial, a transvenous, or a combined approach. Those with minor symptoms without cortical venous drainage can be treated with manual carotid compression, 41 medical therapy, or conservative observation without intervention, which sometimes leads to thrombosis of the shunts.36 It is important to verify that there is no carotid artery stenosis before initiating manual carotid compression. Surgical interventions are rarely necessary, due to the high success rate of endovascular treatment. However, surgical ligation of the origin of the cortical venous drainage can be simply performed and effective when endovascular treatment fails.
During transarterial embolization, special attention should be paid not to compromise the cranial nerve vascular supply and to prevent the migration of embolic agents into the cerebral circulation through anastomosis between the external carotid artery (ECA) and the internal carotid artery (ICA).42 Partial treatment may be warranted to eliminate cortical venous drainage, decrease noise, or improve cranial nerve dysfunction in some situations, such as in elderly patients with significant risk factors for extensive embolization and anesthesia.
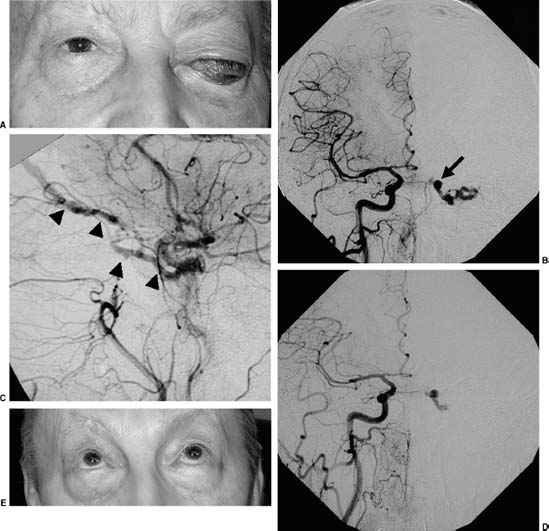
FIGURE 16-3 A 67-year-old right-handed man presented with progressive visual loss, exophthalmos, and chemosis of the left eye over the last 3 weeks. The patient had subjective bruit for the last few months. Despite maintaining normal intraocular pressure by medication, progressive visual loss and retinal hemorrhage were detected. (A) A clinical photograph before treatment shows significant proptosis and chemosis of the left eye. (B) An anteroposterior view of the right common carotid angiogram demonstrates the left cavernous dural arteriovenous fistulas (DAVFs) supplied by C5 branches of the right internal carotid artery and ascending pharyngeal artery branches crossing the midline. The venous drainage is predominantly to the dilated left superior ophthalmic vein (arrow). (C) The midarterial phase of the left common carotid angiogram in the lateral view demonstrates the left cavernous DAVFs supplied by small C5 branches of the internal carotid artery and the accessory meningeal artery and ascending pharyngeal artery branches, draining to the left superior ophthalmic vein (arrowheads). (D) An anteroposterior view of the right common carotid angiogram after the embolization shows residual shunts to the left cavernous sinus from the right C5 branches with partial opacification of the left superior ophthalmic vein with increased stagnation of contrast material. (E) The patient was further treated with manual compression of the left carotid artery with complete resolution of the symptoms. In this clinical photograph taken 4 months after the embolization, complete resolution of the exophthalmos and chemosis can be seen.



