Enhancing Cranial Nerve(s)
Anne G. Osborn, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Metastases
Neurofibromatosis Type 2
Neurofibromatosis Type 1
Plexiform Neurofibroma
Optic Nerve Glioma
Multiple Sclerosis
Optic Neuritis
Less Common
Viral, Post-Viral Neuritis
Bell Palsy
Herpes Zoster
ADEM
Lyme Disease
Lymphoma
Neurosarcoid
Opportunistic Infection, AIDS
Leukemia
Rare but Important
Ischemia
Diabetes
Arteriolosclerosis (Microvascular Disease)
Langerhans Cell Histiocytosis
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Enhancement of cisternal, cavernous sinus CN segments always abnormal
Which cranial nerve(s) affected?
Optic nerve: MS, NF1 (optic glioma), viral/post-viral
CN3, 6: Often ischemia (diabetes, arteriolosclerosis)
CN7: Bell palsy, Herpes zoster (Ramsay Hunt)
CN8: Schwannoma (sporadic or NF2 associated), metastasis
If multiple nerves involved, consider
Metastases, lymphoma, leukemia
NF2
Lyme disease
CIDP (especially if nerves massively enlarged)
History important
Optic neuritis (majority have or develop MS)
Known neoplasm
Flu-like illness (ADEM, viral neuritis)
Helpful Clues for Common Diagnoses
Metastases
Most common: CSF spread
Involves pia, CNs, may extend along perivascular spaces
Multiple thickened nerves > solitary involvement
Fundus of CPA/IAC most common site
Less common: Perineural tumor extension from extracranial primary
Extension into cisternal CN uncommon
Squamous cell, adenoid cystic carcinoma (CN5, 7 involvement most common)
Neurofibromatosis Type 2
Multiple schwannomas
Bilateral acoustic schwannomas diagnostic
Acoustic schwannoma plus schwannoma of one other CN highly suggestive
Schwannoma of “small” CN (e.g., CN3, 4) should raise consideration of NF2
Neurofibromatosis Type 1
Plexiform Neurofibroma
Intracranial involvement less common than scalp, orbit, face (e.g., parotid gland)
Plexiform neurofibromas of CN3 or CN5 may extend intracranially, involve cavernous sinus
Optic Nerve Glioma
Most are typical pilocytic astrocytomas (PAs)
15-20% of NF1 patients develop PA (most commonly in optic pathway)
Up to 1/3 of patients with optic pathway PA have NF1
Enhancement varies from none to striking
May be uni- or bilateral, extend to/from orbit, involve nerves/chiasm/hypothalamus
Multiple Sclerosis
Optic nerve (ON) most commonly affected
50-60% of patients with optic neuritis ultimately develop MS
Imaging
Mildly enlarged, enhancing ON
40% extend to intracanalicular, prechiasmatic/chiasmatic segments
Other CNs (e.g., trigeminal nerve) less commonly affected
Non-MS associated optic neuropathy
Infectious (viral)
Anterior ischemic optic neuropathy (AION)
Helpful Clues for Less Common Diagnoses
Viral, Post-Viral Neuritis
Bell Palsy
Enhancement of intratemporal facial nerve
“Tuft” of enhancement in IAC less common
Herpes Zoster
Ramsay Hunt syndrome (Herpes zoster oticus) = vesicular rash of pinna, involvement of CN7, 8 in IAC, cochlea
Other CNs (e.g., 5) less common
ADEM
Rare manifestation of post-viral demyelination
Affected nerve minimally enlarged, enhances transiently
Lyme Disease
Most common = MS-like lesions in patient with skin rash, flu-like illness following deer tick bite
Can involve multiple CNs (CN7 most common)
Lymphoma, Leukemia
Diffuse pial tumor spread → multiple CNs
Neurosarcoid
Most common intracranial involvement = optic nerve/chiasm/hypothalamus
Other CNs rare
Opportunistic Infection, AIDS
Tuberculous meningitis, CMV neuritis (retina, optic nerve)
Helpful Clues for Rare Diagnoses
Ischemia
Diabetes, microvascular disease
CN3, 6 most commonly affected
Optic nerve (anterior ischemic optic neuropathy) less common
Transient enhancement, then atrophy
Langerhans Cell Histiocytosis
Usually children
Optic nerve/chiasm/hypothalamus/infundibular stalk most common
Infiltrated, thickened structures enhance strongly, uniformly
Disseminated intracranial LCH rare
Sulcal/cisternal enhancement
Multiple enhancing CNs
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
Typical setting = chronic MS
Serial demyelination, remyelination → “onion bulb” thickening of affected nerves
Massive enlargement, enhancement of spinal, cranial nerves (spinal > > CNs)
Image Gallery
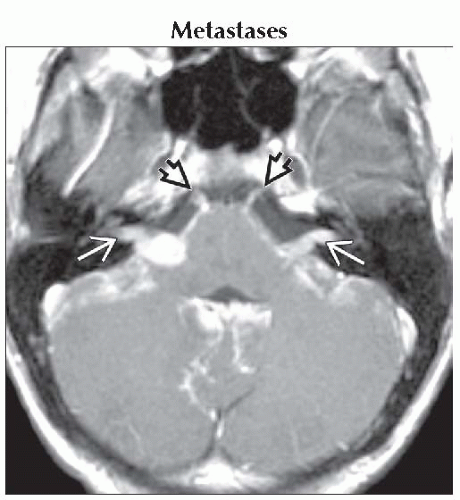 Axial T1 C+ MR in a patient with disseminated malignant glial neoplasm shows diffuse enhancing metastases covering brain, CPA/IACs
 , both abducens nerves , both abducens nerves  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|