Epilepsy, General
Bronwyn E. Hamilton, MD
DIFFERENTIAL DIAGNOSIS
Common
Acquired Causes
Trauma
Remote Stroke
Remote Infection
Neoplasms
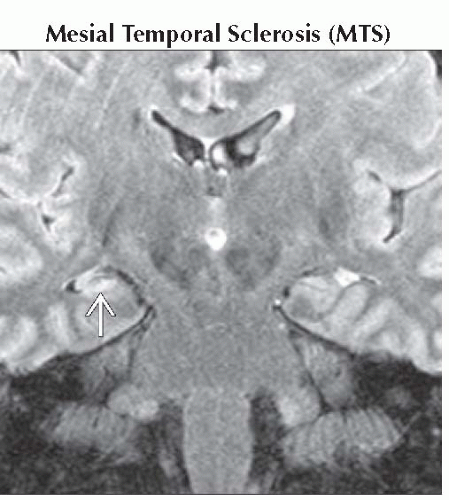
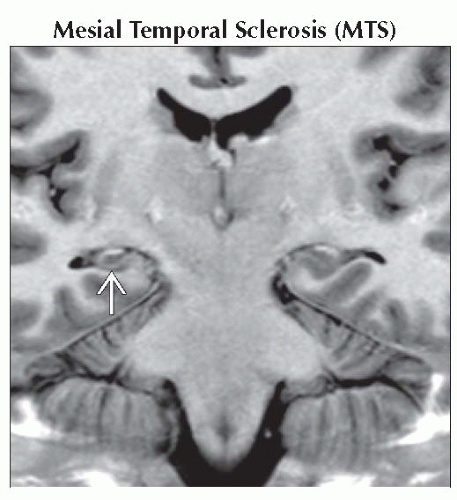
Mesial Temporal Sclerosis (MTS)
Vascular Malformations
Toxic/Metabolic Insult, NOS
Drug Abuse
Heterotopic Gray Matter
Perisylvian Dysplasia
Schizencephaly
Septo-Optic Dysplasia
Tuberous Sclerosis Complex (TSC)
Focal Cortical Dysplasia, Taylor Type (Balloon Cell Dysplasia)
Focal Cortical Dysplasia
Pachygyria-Polymicrogyria
Lissencephaly Type 1
Band Heterotopia
Hemimegalencephaly
Less Common
Neuronal & Mixed Neuronal-Glial Tumors
DNET
Ganglioglioma
Pleomorphic Xanthoastrocytoma
Rare but Important
Sturge-Weber Syndrome
Status Epilepticus
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Generalized seizure disorders usually nonlocalizing
Partial complex (focal) epilepsy usually due to focal structural abnormality (i.e., MTS)
High-resolution MR necessary to fully evaluate epilepsy
Helpful Clues for Common Diagnoses
Acquired Causes
Trauma is most common cause in adults
Trauma, remote stroke, or infection results in encephalomalacia &/or gliosis, which may cause epilepsy
Benign, malignant tumors
MTS: Small, hyperintense hippocampus associated with temporal lobe epilepsy
Causative vascular malformations include AVM & cavernous malformations
Toxic-metabolic & drug abuse patients may present with seizures
Heterotopic Gray Matter
Gray matter (GM) nodules, follow GM signal on all MR sequences
Subependymal most common location
Can be found incidentally in patients without seizures
Perisylvian Dysplasia
Common site for cortical dysplasia
Typically bilateral
± Septo-optic dysplasia, schizencephaly
Schizencephaly
CSF cleft extending to ventricular ependyma, GM-lined
Outpouching or “dimpling” of lateral ventricular contour “points” to cleft
Two morphologic varieties
Closed lip: GM ependymal seams touch
Open lip: GM seams separated by cleft
May be unilateral or bilateral
Absent septum pellucidum common
Associated with septo-optic dysplasia
Septo-Optic Dysplasia
Some consider mildest form of holoprosencephaly
Septum pellucidum absence + optic nerve hypoplasia, ± pituitary dysfunction
Common associated malformations: Schizencephaly, perisylvian dysplasia
Tuberous Sclerosis Complex (TSC)
T2 hyperintense cortical/subcortical tubers
Subependymal nodules follow white matter (WM) signal until calcified
10-15% develop giant cell astrocytoma
Focal Cortical Dysplasia, Taylor Type (Balloon Cell Dysplasia)
Imaging & histology = tubers in TSC
Histology shows “balloon cell” dysplasia
Solitary dysplasia; lack other TSC features
T2 hyperintense “comet tail” from cortex to ventricle; best seen on FLAIR > T2 > T1
Focal Cortical Dysplasia
Thickening &/or nodular cortex
Blurred gray-white junction
Pachygyria-Polymicrogyria
Pachygyria: Thick, smooth cortex
Polymicrogyria: Small, “pebbly”, cobblestone or micronodular appearing gyri (cortical dysplasia)
Lissencephaly Type 1
“Smooth” brain lacking normal gyral infolding; thick cortex
Spectral continuum with polymicrogyria-pachygyria
Band Heterotopia
Most genetic; X-linked inheritance
Most (90%) are female
Males severely affected, rare survival
Band of incompletely migrated GM between cortex & ventricle (double cortex)
GM band size inversely proportional to overlying cortex thickness
Hemimegalencephaly
Unilateral hemispheric overgrowth
Dysplastic enlarged ipsilateral ventricle
Overlying skull & soft tissues overgrown
Helpful Clues for Less Common Diagnoses
DNET
Discrete T2 hyperintense “bubbly” cortical mass, low grade neuronal neoplasm
Associated cortical dysplasia common
Medial temporal lobe most common
Ganglioglioma
Cystic/solid enhancing, cortically based mass, mixed neuronal-glial tumor
Temporal lobe most common site
Associated cortical dysplasia common
Pleomorphic Xanthoastrocytoma
Cyst + enhancing nodule classic
Well-circumscribed, no surrounding edema
Involvement of adjacent meninges typical
Helpful Clues for Rare Diagnoses
Sturge-Weber Syndrome
Malformation of cortical & pial veins
Clinical diagnosis by trigeminal distribution facial “port-wine” stain
Earliest intracranial finding = ipsilateral enlarged choroid plexus
Later = ipsilateral hemiatrophy
Status Epilepticus
Focal cortical (& subcortical) edema, T2 hyperintense
Varied cortical enhancement
Usually DWI & FLAIR bright
Persistent seizures, often > 24 hours
May show hyperperfusion: High CBV & CBF, delayed MTT
Most resolve in days-weeks
Long term atrophy may result
Other Essential Information
“New onset seizures” require routine brain MR with & without contrast
Rule out acute lesions: Hemorrhage, tumor, infection, & stroke
“Epilepsy” high resolution MR evaluation
High resolution T1/T2 (3D techniques at 1 mm slices preferred) through entire brain
IR techniques improve gray-white matter contrast (STIR, FLAIR, & T1 FLAIR)
High field strength (3T) preferred
Image Gallery
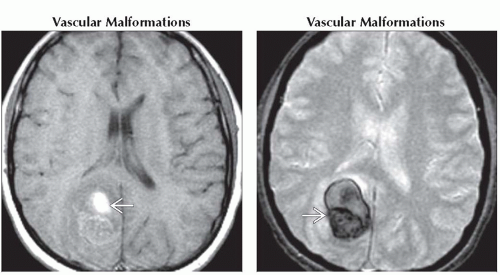 (Left) Axial T1WI MR shows hyperintensity related to recent hemorrhage in a cavernous malformation
 . Seizures are often the presenting symptom for vascular lesions such as a cavernoma or AVM. (Right) Axial T2* GRE MR shows susceptibility artifact in this cavernous malformation . Seizures are often the presenting symptom for vascular lesions such as a cavernoma or AVM. (Right) Axial T2* GRE MR shows susceptibility artifact in this cavernous malformation  with recent hemorrhage. GRE/SWI MR is helpful to search for additional lesions that may be occult on other sequences. with recent hemorrhage. GRE/SWI MR is helpful to search for additional lesions that may be occult on other sequences.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|