♦ Preoperative
Imaging
- Contrast enhanced head computed tomography with sagittal and coronal reconstructions: evaluate for bony erosion of floor of the anterior fossa, sinus cavities, and orbits
- Contrast enhanced brain magnetic resonance imaging: determine the extent of soft tissue disease, intracranial and orbital involvement
- Consider acquiring preoperative scan for intraoperative image guidance
Operative Planning
Interdisciplinary Approach Required
- Otolaryngology: determine extent of sinus and cervical disease; to acquire a tissue biopsy, determine transfacial approach for tumor resection, perform neck dissection if cervical disease present
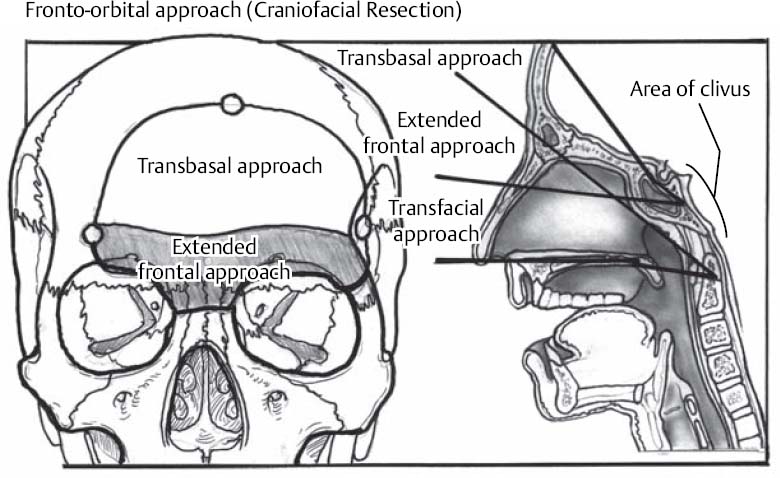
- Neurosurgery: determine extent of anterior cranial fossa, dural, and intradural involvement; determine transcranial approach for tumor resection (Fig. 53.1)
- Neuro-ophthalmology: to identify visual deficits, determine extent of orbital involvement, assist during intraorbital tumor resection and orbital reconstruction
- Medical oncology: to assess for metastatic disease; administer pre- or postoperative chemotherapy therapy if indicated
- Radiation oncology: to administer pre- or postoperative radiation therapy if indicated
Modified Kadish Staging
- A: tumor in nasal cavities
- B: tumor in paranasal cavities
- C: tumor locally advanced beyond paranasal cavities
- D: metastatic disease to cervical lymph nodes or elsewhere
Fig. 53.1 Dissection corridors allowed by fronto-orbital approaches: transbasal, extended frontal, and transfacial.
Biopsy
- Required prior to definitive therapy; acquired by otolaryngologist
Preoperative Adjuvant Therapy
- Preoperative radiation therapy: considered for all stages of disease
- Preoperative chemotherapy: considered for Kadish stage C lesions
Routine Equipment
- Major craniotomy tray
- Mayfield head holder or horseshoe headrest
- High-speed drill
- Lumbar drain set-up
- Operating microscope
- Fibrin glue
Special Equipment
- Ear, nose, and throat transfacial/transnasal tray and endoscopic set-up per otolaryngology
- Image guidance system
- Leyla bar for self retaining retractors
- Tarsorrhaphy set-up
- Headlights
- Loupes
- Bipolar and monopolar cautery
- Endoscopy equipment
- Image guidance equipment
Anesthetic Issues
- Antibiotics (cefazolin: 2 g intravenously at least 30 min prior to incision and then every 4 hours or vancomycin: 1 g intravenously 30 min prior to incision and then every 12 hours)
- Dexamethasone (10 mg intravenously) preoperative
- Antiepileptic medication (phenytoin 15 mg/kg intravenously during surgery to achieve therapeutic level)
- Mannitol (1 g/kg intravenously at incision)
- Precordial Doppler to monitor for air embolism (superior sagittal sinus exposed with bifrontal craniotomy)
- Anticipate 2 to 4 liters of blood loss
- Arterial line and either good peripheral venous or central venous access
♦ Intraoperative
Spinal Drain
- Five to 10 mL of cerebrospinal fluid (CSF) are removed periodically to facilitate brain relaxation and reduce frontal lobe retraction.
Positioning
- After intubation, the patient is placed in a lateral decubitus position for spinal drain insertion via L4–L5 interspace.
- The patient is then positioned supine. The neck is slightly extended. The head is placed on a horseshoe headrest or pinned in a Mayfield head holder if self retaining retractors or image guidance is utilized for resection of intracranial disease.
Tarsorrhaphies
- Performed bilaterally
Preparation of Operative Fields
- Sterile preparation of the head and face are performed. The abdomen is sterilely prepared for harvesting of a fat graft.
Bifrontal Craniotomy
- Bicoronal incision from zygoma to zygoma. The scalp, galea, and pericranium are reflected anteriorly and the periorbita is reflected from the orbits. Temporalis muscle is reflected inferiorly.
- Bifrontal craniotomy is then performed. This craniotomy should extend from one superior temporal line to the other.
- Dura is reflected from the anterior cranial base and cribriform plate. Olfactory fibers are divided. Dural openings are primarily repaired if intracranial tumor is not present.
- Nasal, ethmoid, and orbital osteotomies are performed to remove the supraorbital bar if required.
- Frontal sinus exenteration and cranialization is performed.
- Cottonoids are applied to cover the inferior dura.
- Nasal, ethmoid, and orbital osteotomies are performed to remove the supraorbital bar if required.
Tumor Resection
- If present, intracranial tumor is resected with involved dura. Dura is replaced with allograft, fascia, or pericranium.
- Additional osteotomies are performed to access tumor if required.
- The otolaryngologists perform the transfacial procedure to resect tumor. This may involve a lateral rhinotomy incision or transnasal endoscopy. Nasal, ethmoidal, or maxillary osteotomies may be required. The medial canthal tendon and lacrimal system may require sectioning.
- Specimens are sent to verify pathology and margin status.
Reconstruction
- The anterior cranial base is reconstructed. Pericranium is isolated from the scalp flap. This vascularized pedicled flap is layered over the defect in the anterior cranial fossa and secured to dura with several sutures. A split-thickness calvarial bone graft that covers the bone defect in the floor of the anterior cranial fossa is inserted between the leaves of the pericranial graft. Fibrin glue is generously applied. Fat graft harvested from the abdomen may be used to occupy dead space.
- The medial canthal tendon is repaired if sectioned.
- Dacryocystorhinostomy is completed if the lacrimal duct has been sectioned.
♦ Postoperative
- Significant intraoperative fluid resuscitation may have occurred. Extubation may be delayed secondary to pulmonary and airway edema.
- Spinal drainage may be continued at 5 to 10 mL/hr for 2 to 3 days.
- Antibiotics are continued for 24 hours.
- Antiepileptic medication is continued for 5 days if intracranial tumor resected.
- Nasal packing is removed after 5 days by otolaryngologists, if utilized.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue