II 6 Evaluation and Management of Spinal Cord Injury 7 Spinal Rehabilitation and Disability Evaluation 9 Thoracolumbar Spine Fractures I. Introduction A. Approximately 12,000 to 14,000 spinal cord injuries occur in North America per year. 1. Most commonly affect adolescent males 2. Most are caused by motor vehicle collisions II. Prehospital evaluation period A. Care of any trauma patient begins with immobilization of the spine at the scene of injury. B. American College of Surgeons mnemonic for in-field management of a trauma patient 1. A—airway 2. B—breathing 3. C—circulation 4. D—disability 5. E—exposure and environment C. All trauma patients should be immobilized with a rigid cervical orthosis and transferred using lateral bolsters. 1. The patient should be placed on a long backboard secured with tapes or straps. 2. Helmeted athletes a. Helmet and shoulder pads should not be removed. III. Emergency room management A. Polytrauma patients may have an altered level of consciousness and are vulnerable to further worsening of their neurological injuries. B. Once the ABC’s have been established, a thorough but focused physical examination to assess the patient’s neurological function should be performed. 1. Entire spinal column should be palpated for “step-off” or misalignment of the spinous processes.
Trauma
6
Evaluation and Management of Spinal Cord Injury
| Eye opening | Voice | 3 |
| Pain | 2 | |
| None | 1 | |
| Verbal response | Oriented | 4 |
| Inappropriate | 3 | |
| Incomprehensible | 2 | |
| None | 1 | |
| Motor response | Obeys commands | 5 |
| Localized pain | 4 | |
| Withdraws | 3 | |
| Decorticate | 2 | |
| Decerebrate | 1 |
C. Head trauma
1. Glasgow coma scale
a. Total score can range from 15 (normal responses to stimuli) to 3 (no response or comatose) (Table 6–1).
D. Evaluation of airway and breathing
1. Elective intubation should be performed in patients with severe head injuries or who are unable to protect the airway because of a depressed level of consciousness (Glasgow coma scale < 8).
2. Patients with spinal cord injuries (particularly above C5) having difficulty with respiration should be considered for elective intubation.
3. Manual in-line stabilization of the cervical spine during orotracheal intubation is a technique that minimizes motion of the unstable cervical spine.
E. Neurological examination
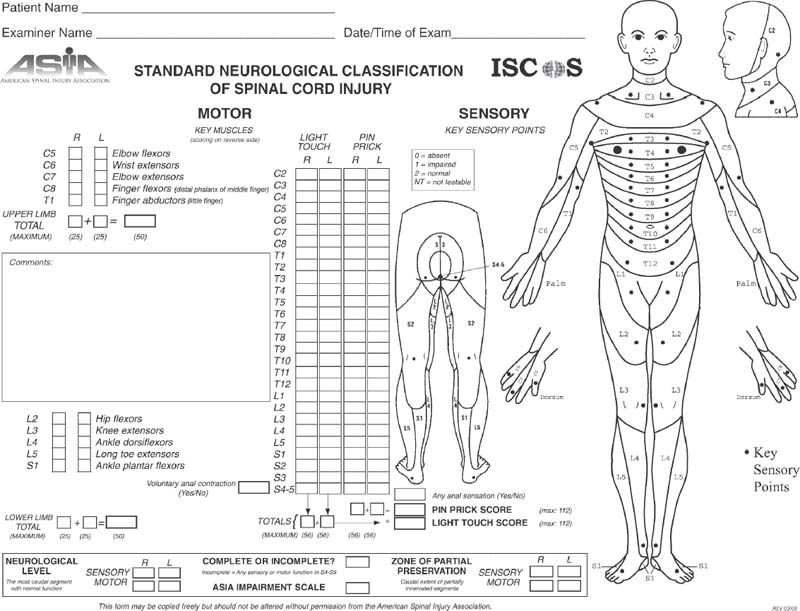
1. American Spinal Injury Association (ASIA) standard of neurological testing provides a concise and detailed method of evaluating spinal cord and peripheral nerve root function.
a. Sensation is determined in all 28 dermatomes bilaterally by the patient’s ability to detect the sharp end of a pin (Fig. 6–1).
b. Motor function is documented and graded 1 to 5 based on resistance to physical manipulation or gravity (Table 6–1).
c. Based on both the motor and sensory examination, the patient is further classified or graded using the ASIA modification of the Frankel neurological classification system (Table 6–2).
F. Spinal cord injuries
1. Complete injury
a. No functional motor (less than grade III motor strength) or sensory activity below the zone of injury
2. Incomplete injury