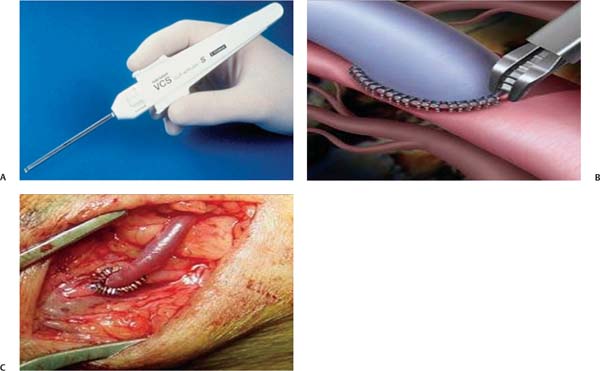
Chapter 21 The first vascular anastomosis was described by Eck in 1877.1 The French physician Carrel developed and published in 1902 the first arterial end-to-side anastomosis using fine suture material and triangulation.2 The development of neurosurgical vascular bypass techniques made a leap in the 1960s, when the merging with the development in surgical magnification led to the rapid growth of cerebral microvascular surgery.3 Since then, to construct a microvascular anastomosis, temporary occlusion of the recipient vessel and end-to-side attachment of a donor vessel with interrupted or continuous microsutures is still the standard technique in neurosurgery and other professions using microanastomoses. The conventional microanastomosis has several benefits. The first is the well-known reliability of the anastomosis over the long term. Enormous experimental and clinical experience has been acquired in the past 100-plus years. The second benefit is the relative flexibility of the method. The anastomosis can adapt to many different tissue conditions and localizations. Finally, the suture material is readily available and relatively inexpensive. Nevertheless, a sutured conventional microanastomosis has several disadvantages. The first disadvantage is the potential vascular wall damage caused by the penetrating needle and passage of the suture material. This can influence the local healing response and may cause an inflammatory reaction, thrombocyte aggregation, impaired endothelial function, intimal hyperplasia, and hence stenosis. Although different types of nonabsorbable suture materials, absorbable sutures, and atraumatic needles have been used to create vascular anastomoses, vascular wall damage cannot be eliminated by any of these devices.4 The second disadvantage is the technical difficulty that is associated with conventional anastomosis creation when the depth of the anastomosis is increased and the working channel is narrow, as is often the case in vascular neurosurgery. A third disadvantage is the temporary occlusion time of the recipient artery during anastomosis attachment. This potentially results in ischemia in the flow territory of the recipient artery.5 Moreover, the temporary clips can damage the recipient artery vessel wall. Therefore, a conventional microanastomosis is certainly not an ideal anastomosis. An ideal microanastomosis should meet several criteria. First, the attachment should not cause damage to the recipient artery. Second, it should be possible to perform the anastomosis relatively easily and quickly. For neurosurgical purposes, it is important that the anastomosis can be constructed through a narrow working channel and at increased depths without damaging or even touching surrounding intracranial structures. Third, the anastomosis should not be accompanied by typical problems like leakage in the acute phase or pseudoaneurysm formation in the chronic phase. Finally, it has to be shown that the anastomosis reendothelializes in the long term, including eventual intraluminal parts, without causing intima hyperplasia and resulting stenosis. Several attempts have been made to invent an ideal anastomosis: sutures have been reduced or even abandoned (“sutureless”) as well as temporary occlusion (“nonocclusive”). In this chapter we further describe some of the most intriguing new techniques developed to partially or fully meet the criteria of an ideal anastomosis. Generally, a surgical sealant is easier and more quickly applied than a suture. Anastomosis attachment with only surgical sealant is currently impossible because the anastomotic strength is too low, resulting in leakage and pseudoaneurysm formation. However, during replacement of part of the sutures or as an adjunctive next to an anastomotic device, some sealants have been shown to be of use.6,7 Using a sealant to replace several sutures needed to attach any type of anastomosis theoretically simplifies the procedure and reduces complications and surgery time. Furthermore, it would make an anastomosis possible on locations at which it is impossible to suture in one or more quadrants. Four families of surgical sealants are currently available that can be used for vascular anastomosis sealing. The first group is formed by the fibrin sealants. Benefits include good applicability and nontoxicity. Several fibrin sealants are approved for intracranial use, such as Tisseel (Baxter Healthcare Corp., Deerfield, IL) and Beriplast (CSL Behring, King of Prussia, PA). Fibrin sealants have less strength than other sealant families. Moreover, the glue is very fluent at application, which can result in unintentional entering of the anastomosis or migration to other areas. However, patches coated with fibrinogen and thrombin (TachoSil; Nycomed, Zurich, Switzerland) circumvent these drawbacks and have better strength. This sealant shows less migration but with good flexibility.8 The second category is composed of a bovine serum albumin/glutaraldehyde sealant (Bioglue, Kennesaw, GA). This sealant has good applicability and strength, but it has toxic potential. It has not been approved by the U.S. Food and Drug Administration (FDA) for intracranial use. The third group is formed by the polyethylene glycol sealants (DuraSeal, Covidien plc, Dublin, Ireland; CoSeal, Angiotech Pharmaceuticals, Vancouver, British Columbia, Canada). The benefits of these sealants include strength and nontoxicity, and they are FDA approved for intracranial use. They are difficult to apply because of low viscosity and unpractical applicators, however, and they swell within 24 to 48 hours after application. The fourth group comprises the cyanoacrylate sealants (OMNEX; Ethicon, Somerville, NJ). These sealants are strong but are histotoxic and nondeformable after polymerization, which is very fast. Hence, they are difficult to apply. In conclusion, the optimal intracranial anastomotic sealant has not been found yet. The most promising sealant is a patch coated with fibrinogen and thrombin (TachoSil). Another option to replace a suture is a clip. Two systems are currently on the market, and both have been used for cerebral revascularization. The vascular closure staple (VCS) system (United States Surgical Corp., Norwalk, CT) involves titanium clips with non-penetrating tips, housed in an automated, disposable clip applier (Fig. 21.1). Four different sizes of clips are available for different vessel wall thickness, from 0.9 to 3.0 mm. The clips are applied to everted vessel edges in an interrupted fashion.9 The main advantage of the system is that no intraluminal foreign body is present, resulting in minimal platelet aggregation and less endothelial damage than conventional suturing methods. The system does not penetrate the vessel lumen or compromise its diameter. Its main drawback is the technical challenge involved in inverting the walls of atherosclerotic vessels and joining the vessels, especially when the anastomosis is deep.10 Microsurgical training and knowledge of clip-related pitfalls are mandatory. Fig. 21.1 (A) Vascular closure staple (VCS) applier (United States Surgical Corp., Norwalk, CT). (B,C) End-to-side VCS anastomosis. Fig. 21.2 (A) U-clip anastomotic device before deployment. (B) U-clip anastomotic device after deployment. (Courtesy of Medtronic, Inc., Minneapolis, MN.)
Evolving Technology for Open Surgical Revascularization
 Conventional Microanastomosis
Conventional Microanastomosis
 Ideal Microanastomosis
Ideal Microanastomosis
 New Techniques
New Techniques
Sealants
Clips
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree