21 Exploring New Frontiers
Endovascular Treatment of the Occluded ICA
Introduction
Surgical revascularization of the occluded extracranial carotid artery has been established as a potential therapy in selected patients.1 However, this procedure has not been widely applied because its intrinsic risks and the questionable benefits. Endovascular revascularization of acutely and chronically occluded femoral and coronary arteries has been performed for some time with good degree of clinical and radiological success. Application of these techniques to the extracranial carotid and vertebral arteries has lagged behind for fear of dislodging emboli. With advances in endovascular techniques, increasing experience with angioplasty and stenting of large extracranial cervical vessels, and the availability of a variety of distal protection devices, several operators have reported their results following endovascular revascularization of the acutely or even chronically occluded internal carotid artery (ICA).2–20 In this chapter, we provide an overview of the rationale, techniques, results, and complications of endovascular revascularization of acute and chronic occlusion of the extracranial ICA.
Acute carotid occlusion
Management of patients with stroke caused by acute ICA occlusion is challenging. Medical therapy alone is associated with a high rate of permanent severe neurological disability and mortality.1 In patients with acute stroke and ICA occlusion, early restoration of flow in the occluded ICA may prevent further worsening, improve symptoms, and reduce the risk of recurrent stroke.2 Currently, the invasive treatment of patients with acute ICA occlusion is not standardized. Acute ICA occlusion responds poorly to intravenous thrombolysis alone or in combination with intra-arterial pharmacological thrombolysis with recanalization rates ranging from 10%21 to 50%,22–24 and resultant mortality of 50%.21–24 Slightly better clinical results have been reported following mechanical thrombectomy, but only a few reports are available.25,26
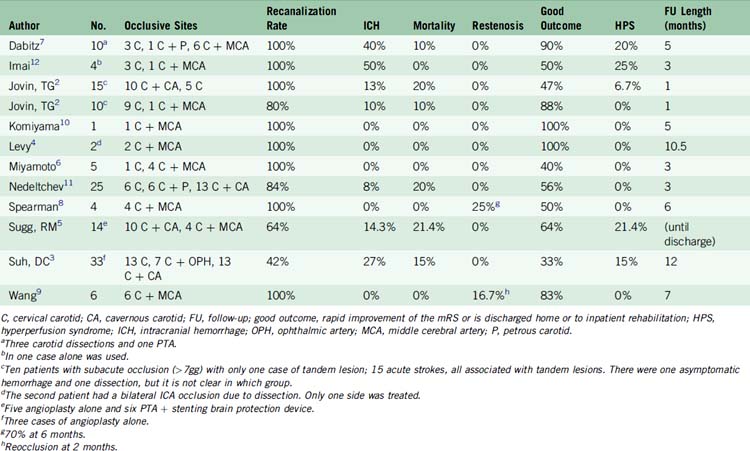
Over the past decade, several authors2,3–11,27 have reported the feasibility of endovascular revascularization of the acutely occluded internal carotid artery with angioplasty and stenting with higher rates of recanalization and clinical improvement than reported with other methods (Table 21–1).
Technique
Symptomatic acute thrombosis of the proximal ICA often occurs in concomitance with ICA bifurcation (T-lesion) or MCA occlusion. The natural history of associated proximal ICA and central distal occlusions is poor.2,3–10,12 Acute revascularization of the proximal ICA in such cases allows catheterization and thrombolysis of the distal segment and, by increasing distal flow, improves the chances of maintaining vessel patency after successful distal thrombolysis. In addition, stenting of the occluded ICA may “trap” thrombus against the carotid wall, potentially decreasing the risk of delayed distal emboli.
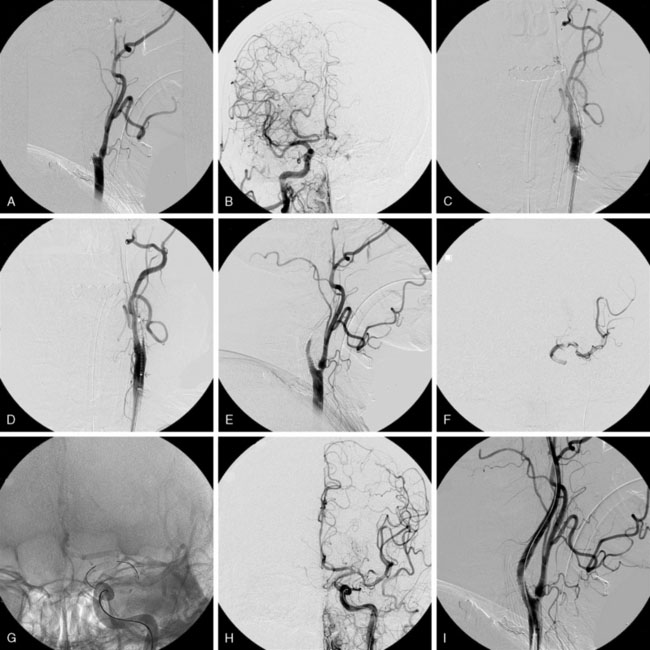
At the completion of the procedure, strict blood pressure control is maintained in those patients with successful recanalization (systolic pressure below 160 mm Hg in patients with acute occlusions or below 140 mm Hg when the occlusion is subacute or chronic). Clopidogrel is continued for 30 days and aspirin indefinitely. A head CT scan is routinely performed the following morning to rule out hemorrhage and to assess the extent of the infarcted area (Figure 21–1).
Results and Complications
Over the past 10 years, several authors have detailed their results with revascularization of the acutely occluded ICA. Nedeltchev and coworkers11 studied 56 consecutive patients who suffered an MCA stroke following ICA occlusion between 1997 and 2003. Twenty-five of these patients underwent attempted endovascular revascularization (endovascular group), while 31 patients received medical treatment consisting of antiplatelet medications and, in some cases, heparin therapy (medical group). Recanalization of the ICA was achieved in 84% of patients in the endovascular group with a combination of thrombo-aspiration through an 8-French guide-catheter and stent deployment in the occluded ICA. Recanalization of the coexistent MCA occlusion (TIMI grade 2 and 3) was obtained in 52% of these patients. In the endovascular group, outcome at 3 months was favorable (modified Rankin score of 0–2) in 56% of patients and unfavorable in 24%. Twenty percent of patients died. In the medically treated group, a favorable outcome was observed in only 26% of patients. This series stresses the importance of recanalization of the coexistent distal occlusion since MCA recanalization was the only predictor of good outcome. Symptomatic hemorrhage occurred in 8%. Although concerns exist regarding the risk of dissection and vessel perforation during blind “probing” of the occluded segment, these complications were not observed in this series.
Jovin and collaborators2 reported a series of 23 patients who underwent successful ICA revascularization (in two additional patients crossing of the occlusion was not possible and no stent could be deployed). Of these 23 patients, 15 were revascularized within the time window for acute stroke therapy while the remaining eight had suffered subacute ICA occlusion and demonstrated ongoing symptoms related to hemodynamic compromise. A good outcome at 30 days was reported in five patients (33%) with acute ICA occlusion. Four of the five patients experiencing a good outcome did not have a coexistent intracranial occlusion and the fifth one had a coexistent MCA occlusion that was revascularized with pharmacological intra-arterial thrombolysis. No patient who had a tandem occlusion that did not revascularize achieved a good outcome. Complications related to the endovascular procedure included one asymptomatic hemorrhage and one dissection of the ICA without flow compromise. No serious complications were observed in the eight patients who had received IV tPA in conjunction with endovascular revascularization indicating the feasibility and safety of this approach. Table 21–1 provides a comprehensive summary of results and complications after revascularization of acute ICA occlusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree