Chapter 15 External Beam Radiotherapy for Tumors of the Spine
EXTERNAL BEAM RADIOTHERAPY TECHNIQUES
CONVENTIONAL 2-DIMENSIONAL RADIOTHERAPY
High-energy megavoltage radiation is produced by a linear accelerator (Fig. 15-1). The generated beam of radiation diverges from the head of the linear accelerator gantry and may be collimated or shaped using simple “jaws” that create square or rectangular fields. A secondary level of collimation can be achieved by placing lead-based alloy blocks in front of the beam to create a unique shape. Conventional radiotherapy using 2D techniques relies on simple 2D x-ray imaging and bony anatomical landmarks to determine where the beams of radiation should be focused. Historically, radiation therapists relied on a detailed knowledge of the relative relationship of internal organs with respect to the bony anatomy to define the radiation fields. These techniques are most commonly used for urgent radiation delivery or when treating simple bony lesions of the axial skeleton.
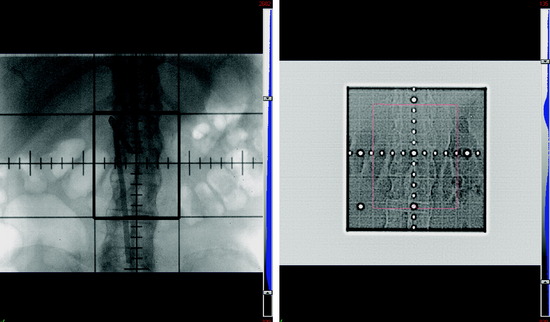
Figure 15-2 depicts a simulated radiation field created to treat a patient who presented with painful bony spinal metastasis at L2. In this x-ray image, the center of the beam is shown by the intersection of the perpendicular crosshairs. The thick continuous lines represent the “jaws,” which create a rectangular central area around the center of the beam that defines the target radiation field. It is customary to include at least one vertebral body above and below the target level when treating spinal metastases. The lateral borders of the field are set to encompass the paraspinal extent of the tumor with additional margin to account for uncertainties of internal organ motion, patient motion, and day-to-day variation in radiation field set-up. Parallel-opposed fields from anterior and posterior projections are used to treat the target within the rectangular field. Opposed lateral fields may be used for cervical spinal lesions. Thus, all the intervening organs and tissues contained in this field also will be irradiated. In this case, the amount of radiation that can be safely delivered is limited by the radiation sensitivity of the normal tissues, such as the spinal cord and small bowel.
THREE-DIMENSIONAL CONFORMAL RADIOTHERAPY AND INTENSITY MODULATED RADIOTHERAPY
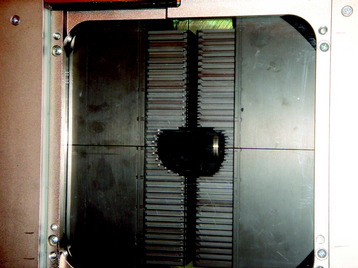
With the advent of computed tomography (CT), creation of complex radiation doses that conform to the shape of the clinical target is feasible. After contouring the target and normal structures on individual CT slices, a 3D representation of these structures is created by digital reconstruction. Unlike simple 2D treatment planning, 3D conformal radiotherapy (3D-CRT) and intensity modulated radiotherapy (IMRT) use an array of radiation beam angles. Custom field blocking of each field is based on the relative relationship between the target and normal structures from the beam’s eye view. The blocking is achieved by either lead-based alloy blocks or by a multi-leaf collimator (MLC). With the MLC, 3- to 10-mm rectangular tungsten leaves are independently positioned a certain distance from the center of the field to create a custom shape of the field (Fig. 15-3). In most cases of 3D-CRT, the radiation dose delivery through each field is both homogeneous (i.e., radiation dose does not vary in intensity) and static (i.e., there is no change in the beam angle or field blocking). The resultant radiation dose distribution will conform to the shape of the target relatively homogeneously. This technique is widely used.
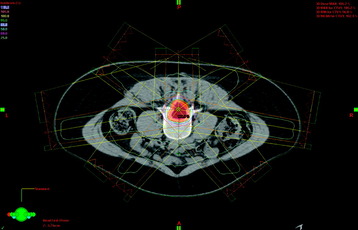
Figure 15-4 shows the radiation dose distribution of a seven-field IMRT plan for a spinal tumor. By converging beams from multiple angles and modulating the dose for each field, the prescription radiation dose, depicted by the yellow curve, tightly conforms to the shape of the target, depicted by the light red shaded contour. At the same time, the radiation dose to the bowel is about 25% of the prescribed dose.
RADIOTHERAPY FOR SPINAL METASTASES AND MALIGNANT SPINAL CORD COMPRESSION
The spine is the most common site of osseous tumor spread of cancer, comprising 40% of skeletal metastases.1–4 Adjuvant radiotherapy after surgery or radiotherapy alone remains a mainstay of palliation of spinal metastases.5–8 Most spinal metastases are either asymptomatic or cause pain only. A smaller percentage evolve to cause epidural compression of the spinal cord or cauda equine.9
Radiotherapy is very effective in palliating pain caused by spinal metastases. A recent review by Falkmer et al10 showed that more than 80% overall pain relief is achievable by radiotherapy for skeletal metastases. Currently, radiotherapy alone is recommended for patients with painful spinal metastases without epidural spinal compression, patients with metastatic epidural spinal cord compression (MESCC) caused by radioresponsive tumors (e.g., lymphoma, leukemia, germ cell tumors), medically inoperable patients, and patients with multiple levels of compression.5,9
Conventional radiotherapy for painful bony metastases is generally delivered either as a single fraction of approximately 8 Gy or as a fractionated course of 20–40 Gy over 5–20 daily fractions. Multiple randomized trials and retrospective reviews have explored the relative palliative benefit of short duration radiation schedules (e.g., 8 Gy in a single fraction) vs. longer schedules (e.g., 30 Gy in 10 fractions).11–16 Even though short and longer schedules of radiotherapy generally have similar effectiveness in early pain relief, re-treatment is required more frequently after the shorter courses.10,12 Therefore, when death does not appear to be imminent, 30 Gy in 10 fractions is generally the preferred palliative course of treatment.
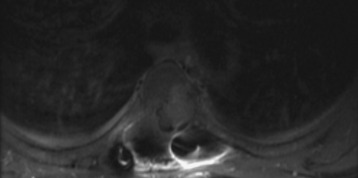
In recent years the important role of surgical resection in addition to radiotherapy for MESCC has been better defined. Patchell et al7 reported a randomized control trial of direct decompressive surgical resection plus adjuvant radiotherapy vs. radiotherapy alone; the results strongly support the use of surgery plus adjuvant radiotherapy for MESCC. In this study, 101 patients with MESCC were randomized. After initiating high-dose steroids, patients were treated as randomized. Ninety-four percent of surgical patients who were ambulatory on study entry retained their ambulatory status compared with only 74% of radiation alone patients. Sixty-two percent of surgical patients who were non-ambulatory at study entry regained walking ability after treatment compared with only 19% of radiotherapy alone patients. These results translate into an overall post-treatment ambulatory rate of 84% in surgery plus radiotherapy patients and 57% in radiotherapy alone patients. The radiation alone results in this study are similar to the results shown by randomized radiation trials of MESCC exploring different radiation schedules. Maranzano et al17–19 reported on several prospective trials including a randomized, multi-institutional trial comparing two different hypofractionation schedules and showed that approximately three-quarters of patients are ambulatory post-treatment and 54–59% show complete relief of back pain. Figure 15-5 shows an example of MESCC at the left posterior aspect of T4.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree