♦ Preoperative
Operative Planning
- Review imaging studies (computed tomography [CT], magnetic resonance imaging, or ultrasound in neonates)
- Access to the lateral ventricle can occur at any point along the midpupillary line with a trajectory that is perpendicular to the skull (if the ventricular system has not been deformed by an intracranial process).
- Majority of access occurs via anterior (frontal) versus posterior placement (Fig. 83.1).
- Frontal location: right Kocher’s point is the most commonly used site because the right frontal lobe is less eloquent (nondominant hemisphere) in most p atien ts.
- Kocher’s point: lies at the perpendicular intersection of:
- Posteriorly directed midpupillary line
- Superiorly directed line starting at the midpoint between the external auditory meatus and the lateral canthus of the ipsilateral orbit
- Posteriorly directed midpupillary line
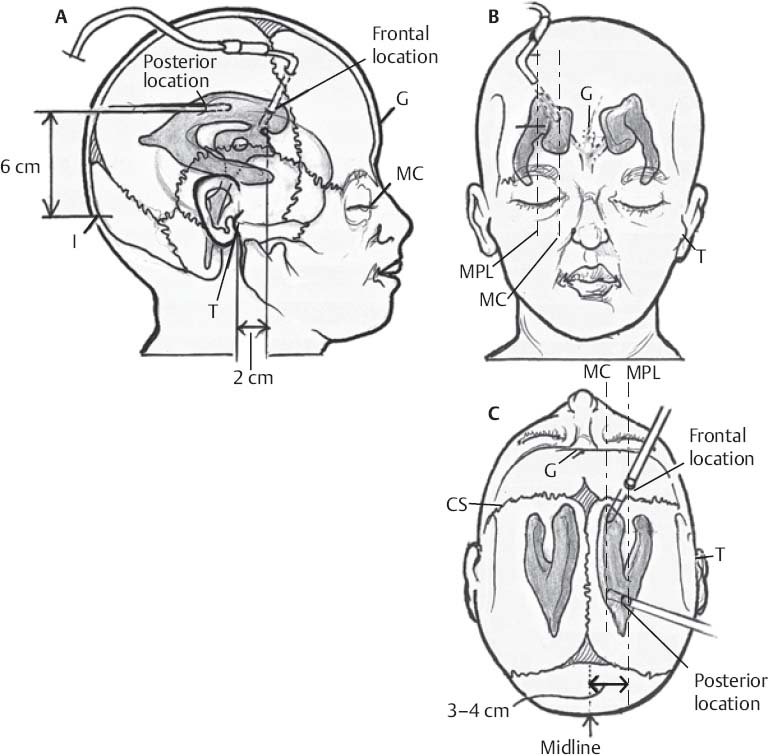
- Alternatively, a site 3 to 4 cm lateral to the midline (along the midpupillary line) and 1 cm anterior to the coronal suture can be used if the coronal suture is palpable.
- Advantages of Kocher’s point: lies anterior to motor strip; lies posterior enough to avoid incision on forehead; lies lateral to superior sagittal sinus and its bridging veins
- Posterior location: Frazier burr hole is placed 6 to 7 cm superior to the inion and 3 to 4 cm lateral to midline; this places the burr hole ~1 cm anterior to the lambdoid suture and allows insertion of the catheter down the length of the body of the lateral ventricle.
- Depth of catheter is estimated from the imaging studies (most important in pediatric patients); in the adult patient, the catheter will most often encounter CSF when advanced no more than 5 cm deep to the inner table of the skull.
Anesthesia Issues
- One percent lidocaine
- Short-acting intravenous (IV) sedation (midazolam or propofol if intubated)
- Avoid paralytics if possible to allow neurologic exam immediately following catheter placement
- At least one dose of IV antibiotics prior to incision to cover skin flora (cefazolin 2 g, clindamycin 600 mg, oxacillin 2 g, or vancomycin 1 g)
- Some advocate continuing IV antibiotics while external ventricular drain (EVD) in place, but this is controversial as microbial selection may occur, putting patient at risk for antibiotic-resistant ventriculitis
- Use of antibacterial impregnated catheter may decrease risk of bacterial colonization but shuold not substitute for preoperative antibiotics
- Some advocate continuing IV antibiotics while external ventricular drain (EVD) in place, but this is controversial as microbial selection may occur, putting patient at risk for antibiotic-resistant ventriculitis
Equipment
- Standard EVD kit includes
- Razors (two)
- Marking pen with ruler
- Sterile prep swabs
- Sterile towels, gauze, and clear plastic drape
- Needles: 25-gauge and 22-gauge
- Sterile saline solution
- Scalpel
- Handheld cranial twist drill
- 3–0 nylon and silk sutures
- Needle driver, forceps, scissors
- Razors (two)
- Standard or antimicrobial-impregnated ventricular catheter
- External drainage collection kit
- Sterile gloves
♦ Intraoperative
Frontal Location
Positioning
- Patient supine with the head of bed slightly elevated (20 degrees) and the neck in a neutral position
- The appropriate side of the head is liberally shaved to allow for adequate sub-galeal tunneling of the catheter; use electric razor if available
- Entry point on scalp is measured with a ruler and marked with a pen
- The shaved area is scrubbed with chlorhexidine for 5 minutes and sterile-prepped
- A clear drape is placed, taking care to clearly define the midline
- One percent lidocaine is injected subcutaneously at the planned incision and at drain exit site
- The drill bit depth guide is set to allow penetration of inner and outer calvarial tables
- A 1-cm stab incision down to the bone is made with the scalpel at the marked site just large enough to permit passage of the drill bit
- The twist drill is held perpendicular to the skull to make a hole in the skull
- Irrigate away the bone chips if required
- Insert drill bit or spinal needle into burr hole to gently puncture the dura, enough to pass the catheter
- If the dura is not opened large enough, and the catheter is forced down the burr hole, an epidural hematoma may develop from stripping the dura
- Furthermore, if the dura is not opened large enough, the catheter may drag on the dura, allowing the stylet to puncture the catheter tip and protrude into the brain parenchyma
- If the dura is not opened large enough, and the catheter is forced down the burr hole, an epidural hematoma may develop from stripping the dura
- The catheter with stylet is inserted perpendicular to the brain surface to a depth no greater than 5 cm below the inner table of the skull (Fig. 83.1A); the stylet is withdrawn to ensure CSF flow; if CSF flow is obtained prior to 5 cm, the stylet is removed and the catheter is passed the remaining distance without the stylet to reduce the chance of injury
- If no CSF flow is obtained at 5 cm, the tendency to insert the catheter further must be resisted
- The catheter shuold be removed without the stylet and flushed with saline
- The landmarks and trajectory shuold be confirmed
- The stylet is reinserted and the catheter redirected
- Aiming the catheter slightly more medially is usually a safe and effective way to establish CSF flow
- The catheter shuold be removed without the stylet and flushed with saline
- For a frontal ventriculostomy, the catheter must be pointed at the glabella in the sagittal plane (Fig. 83.1B); in the coronal plane, the target is ~2 cm anterior to the ipsilateral tragus. This trajectory guides the terminal portion of the catheter toward the frontal horn of the lateral ventricle with the tip near the foramen of Monro (Fig. 83.1A).
- The tunneling device (trocar) is attached to the distal end of the catheter; while holding the catheter proximally as it enters the skull, the distal portion is tunneled under the galea to an exit site at least 5 cm distant from the entry site.
- The distal end of the catheter is connected to the adapter; a tuberculin syringe is then attached to the adapter allowing controlled release of CSF.
- The adapter is secured to the catheter using a 3–0 silk suture; the incision is sutured and the catheter secured to the scalp in at least three places using 3–0 nylon; withdrawal of CSF using the tuberculin syringe checks that the catheter has neither been occluded nor withdrawn during manipulation.
- The distal end of the catheter is then connected to the pressure transducer and/or drainage system; avoid entraining air within the system as air bubbles dampen accurate pressure transduction.
Posterior Location
Positioning
- Patient supine with ipsilateral shuolder roll and head turned fully toward the contralateral shuolder or prone
- Entry point: Frazier burr hole is placed 6 to 7 cm superior to the inion and 3 to 4 cm lateral to midline
Trajectory
- Direct catheter toward the glabella or middle of forehead in the sagittal plane; careful attention shuold be taken to aim toward the medial canthus as there is a natural tendency to cross the midline
- Pass the catheter perpendicular to skull to a depth of 5 cm below the inner table (Fig. 83.1C)
- After CSF flow encountered, stylet is held still and the catheter alone is passed to a depth of 8 to 12 cm (tip shuold be beyond the foramen of Monro)
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue






