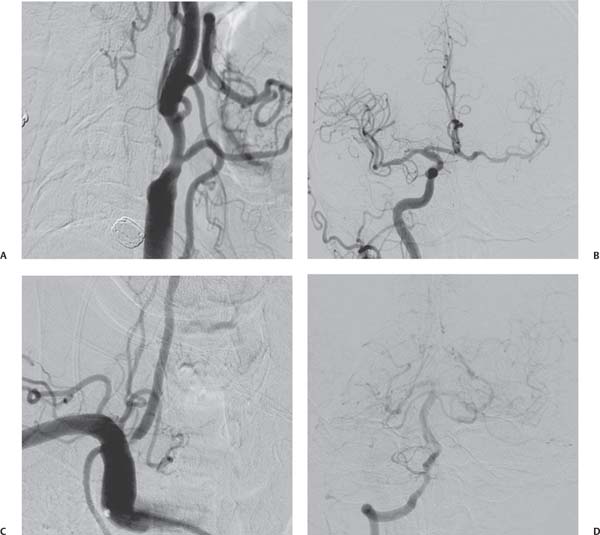
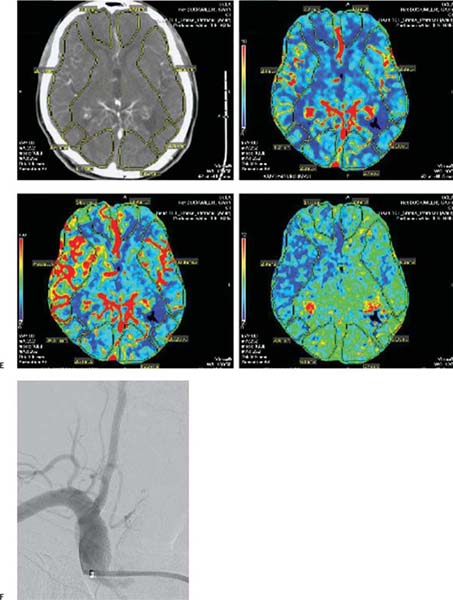
Chapter 13 Stenoocclusive disease of the extracranial vertebral artery may represent a serious disorder with a high potential for death and disability if left untreated. Twice as common in men than women, vessel stenosis usually develops after the age of 60 years. Although often asymptomatic, the 5-year risk of disease progression and development of posterior fossa stroke is estimated to range between 20 and 60%, with a documented mortality rate as high as 30%.1,2 Vertebrobasilar ischemia often remains undiagnosed secondary to nonspecific clinical symptoms, and difficulties in noninvasive visualization of the extradural vertebral arteries. The significance of vertebral artery stenosis, therefore, may be underestimated in current clinical practice. Presenting symptoms may include a constellation of headache, nausea, vomiting, vertigo, imbalance, cranial neuropathy, visual disturbances, and decreased level of consciousness, but an ischemic event often manifests as isolated dizziness.3 Often, it is unclear as to whether the symptoms of vertebrobasilar territory ischemia result from thromboembolic events or from hypoperfusion. Classically, embolic events present as sudden, maximal-onset clinical events referable to high-flow vascular territories, whereas hypoperfusion states result in slower, fluctuating, often positional symptomatology due to reduced distal perfusion pressures secondary to critical or tandem stenoses. Clinical presentation coupled with results of noninvasive cerebral imaging modalities, such as magnetic resonance imaging/angiography (MRI/MRA) and computed tomography angiogram (CTA)/CT perfusion in conjunction with digital subtraction angiography delineate well the pathophysiology of vertebrobasilar ischemia (Fig. 13.1). The vertebral artery arises most frequently from the posterosuperior wall of the subclavian artery. However, it can also arise from the aortic arch, the innominate artery, or the common carotid artery. The vertebral artery is divided into four anatomic segments. The first portion extends from its origin at the subclavian artery to the foramen transversarium at the level of the C6 vertebral body. The second segment travels through the foramen transversarium of the cervical vertebrae to the atlas. The third portion leaves the foramen transversarium of the atlas and extends posteriorly and horizontally on the superior surface of the posterior arch of the atlas until it reaches the dura. The fourth segment pierces the atlantooccipital membrane and the dura and enters the intracranial cavity through the foramen magnum extending to the pontomedullary junction, where it joins with the contralateral vertebral artery to form the basilar artery. Less than 5% of vertebral arteries terminate in the posterior inferior cerebellar artery (PICA). These vessels are usually diminutive, and care must be taken to avoid vessel rupture or infarction due to forceful injections during angiography. The anterior spinal artery most often originates from the intradural vertebral artery. Muscular branches of the cervical vertebral artery anastomose with the ascending cervical, posterior deep cervical, and the external carotid artery branches, most notably the occipital and ascending pharyngeal divisions. Although a greater number of collateral vessels portends better outcome in the setting of vertebral stenoocclusive disease, it is important to be mindful of these branches when manipulating the catheter and wire during angiography.4 The vertebral artery ranges in diameter from 3 to 5 mm. Unilateral vertebral artery stenosis is usually well tolerated due to compensation by the contralateral vertebral artery or cerebral collateral network. This is the reason for the clinically silent nature of many vertebrobasilar disturbances. However, the risk of in situ thrombus formation and distal embolization remains a potential issue even for patients with compensated perfusion from the contralateral vertebral artery. The most frequent cause of vertebral artery stenosis is atherosclerosis, and less commonly vasculitis, dissection, or extrinsic compression. Occlusive disease of the proximal and cervical portions of the vertebral artery represents a risk for posterior circulation ischemia. Atherosclerotic processes most frequently afflict the vertebral origin.5 The extracranial vertebral artery is most susceptible to traumatic injury or spontaneous dissection where it is most mobile, at the entrance to the foramen transversarium at C6 and after it exits the foramen above C2. Narrowing in the third segment can result from an altered head position, most notably extension and rotation.6 Medical treatment for vertebral artery stenosis has historically included the use of antiplatelet agents along with systemic anticoagulation. The efficacy is uncertain. Surgical bypass, endarterectomy, and reconstruction are technically challenging and carry a risk of thromboembolic complications, lung injury, and nerve damage, including Horner syndrome in a significant number of cases.7,8 In symptomatic patients with collateral channels that are poorly demonstrated angiographically, who have failed medical therapy, and for whom surgical bypass procedures present unacceptable risk, balloon-assisted stent angioplasty is reported to be of benefit. There are no clear inclusion criteria or guidelines used for patient selection. Most agree that vertebral artery angioplasty and stenting is indicated for patients with greater than 70% vessel stenosis and symptoms anatomically referable to the territory of the affected vertebral artery who have failed medical therapy. However, the anatomy of collateral circulation, the vascular contribution of the contralateral vertebral artery and the configuration of Willisian collaterals (most notably the posterior communicating arteries) factor into preoperative decision making in patients with less obvious symptomatology and those with less severe stenoses. Fig. 13.1 Diagnostic cerebral angiography in a patient presenting with left hemispheric strokes. (A) Cervical angiogram of the left common carotid artery demonstrates complete occlusion of the internal carotid artery distal to the bifurcation. (B) Intracranial right common carotid artery angiogram demonstrates filling across the anterior communicating artery to opacify the left anterior and middle cerebral arteries. (C,D) Right subclavian angiograms demonstrate stenosis at the ostium of the right vertebral artery and filling of the left middle cerebral artery through the posterior communicating artery. Although the left posterior communicating is quite large, there is relatively little flow through this vessel due to high-grade narrowing of the bilateral vertebral arteries (not shown). (E) CT perfusion. There is an increase in mean transit time and reduction cerebral blood flow in the left middle cerebral artery (MCA) territory, suggesting ischemia. (F) Poststenting angiogram. Because of the high-grade bilateral vertebral origin stenoses, coupled with a chronic left internal carotid artery occlusion, which is relying on poor collateral posterior circulation flow through the left posterior communicating artery, angioplasty and stenting of the right vertebral artery origin were undertaken using a self-expanding stent. Note the proximal stent positioning within the subclavian artery to address plaque extension through the vertebral artery ostium.
Extracranial Vertebral Artery Angioplasty and Stenting
 Background and Indications
Background and Indications
 Technique
Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree