♦ Preoperative
Imaging
- Neurophysiologic monitoring with continuous video EEG
- Establish diagnosis of partial epilepsy and localize/lateralize epileptogenic zone
- High-resolution MRI
- Extratemporal lesions are best detected on the following MRI sequences: fast fluid attenuated inversion recovery axial, fast T2 axial, T1 sagittal, and magnetization prepared rapid gradient echo coronal sequences
- Improved MRI techniques have eliminated many suspected nonlesional cases
- Extratemporal lesions are best detected on the following MRI sequences: fast fluid attenuated inversion recovery axial, fast T2 axial, T1 sagittal, and magnetization prepared rapid gradient echo coronal sequences
- Neuropsychologic evaluation to assess resective risk and localize dysfunctional hemisphere
- Functional imaging: PET and postictal and interictal SPECT
- FDG-PET is often poorly localizing in nonlesional extratemporal epilepsy
- Computer-aided subtraction ictal SPECT coregistered to MRI improves the accuracy of intracranial monitoring
- FDG-PET is often poorly localizing in nonlesional extratemporal epilepsy
- MEG is may be used to localize interictal epileptiform discharges
- May provide unique information when other tests are nonlocalizing
- Goal of presurgical evaluation: localization hypothesis to explain partial epilepsy based on anatomy, semiology, and neurophysiologic data
Operative Planning
- Invasive recordings to prove epileptogenic zone and identify functional cortex (see Chapter 58, Subdural Grid Placement and Chapter 59, Stereotactic Placement of Temporal Depth Electrodes, Figs. 58.1 and 59.1)
- Resection of involved tissue without invasive recordings based on semiology, neurophysiologic data, and metabolic imaging (e.g., premotor frontal lobectomy)
♦ Invasive Recordings
- Useful when presurgical data are discordant and more accurate localization of involved cortex is desirable including relationship to functional cortex
- Can potentially be done in operating room with electrocorticography (limited to interictal data and lack of time) and functional intraoperative mapping
- Best accomplished in chronic fashion with implanted electrodes to gather ictal and chronic interictal data and detailed functional information.
- Surgical technique covered in Chapters 58 and 59
- Resection proceeds based on ictal onset/interictal data identified by the implanted electrodes
- Potential neurologic deficits can be predicted based on location of epileptic zone and surrounding eloquent cortex:
- Frontal lobe epilepsy: motor deficits, supplementary motor area syndrome, frontal eye fields, motor speech
- Parietal lobe epilepsy: sensory deficits, expressive speech, neglect syndromes, visual field defects
- Occipital lobe epilepsy: contralateral homonymous hemianopsia, expressive language deficits
- Frontal lobe epilepsy: motor deficits, supplementary motor area syndrome, frontal eye fields, motor speech
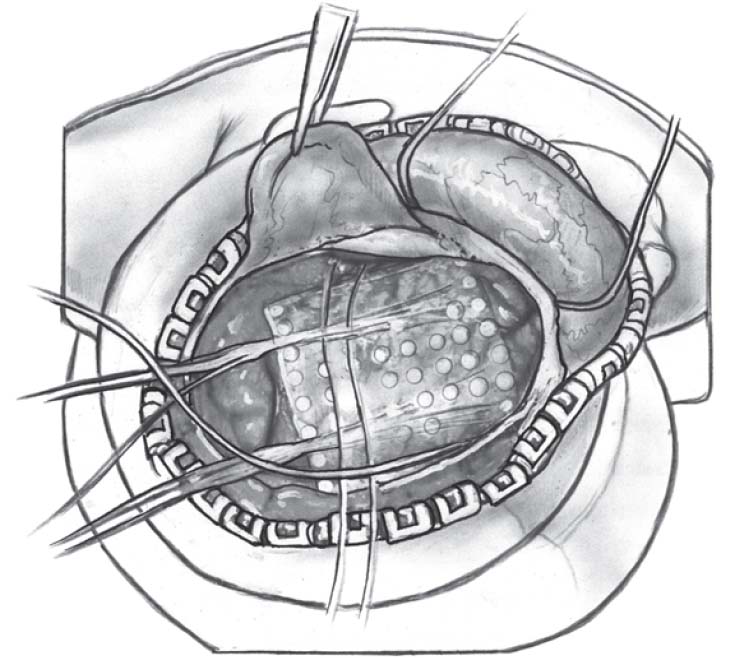
♦ Intraoperative (Fig. 61.1)
Resection After Invasive Electrode Implantation
- Preoperative antibiotics/anticonvulsant therapy
- Under general anesthesia, the patient is positioned with the head rigidly fixed.
- The wires extending in the subgaleal space from the subdural grids and depth electrodes which project through the skin are draped out of the operative field.
- The previous incision is reopened.
- The bone flap is removed and the dura opened without disturbing the position of the grids.
- The location and orientation of the grids is confirmed with the help of the epileptologist.
- The epileptogenic zone and functional cortex are verified beneath the corresponding grid contacts and marked.
- The epileptic zone in nonlesional epilepsy is resected using subpial dissection techniques.
- Careful preservation of the draining cortical veins and arterial supply of adjacent cortex is mandatory.
- One of the grid electrodes is sent for routine culture.
- After meticulous hemostasis, the dura is closed with 4–0 running Nurolon suture.
- The bone flap is replaced and affixed with titanium plates.
- A subgaleal drain may be utilized.
- The galea is sewn with 2–0 Vicryl and the skin sutured with running 3–0 nylon.
- A sterile dressing is applied and the head wrapped.
Frontal Lobe Operative Techniques
- Nondominant frontal lobectomy includes the resection of the three horizontal gyri and anterior cingulate, anterior to the precentral gyrus; the posterior orbital cortex and subcallosal gyrus are spared.
< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree