5 | Failed Anterior Cervical Fusion |
 | Case Presentation |
History and Physical Examination
A 42-year-old female smoker initially presented with right arm radicular pain and a substantial component of axial neck pain. Further discussion of her symptoms revealed loss of fine motor control, handwriting changes, and some gait dysfunction. On physical examination motor function was normal as well as sensation, except for a right C6 radicular decrease in pinprick and touch sensation. A mild cervical myelopathy was illustrated on her physical examination by increased reflexes in the legs and a wide-based tandem gait. Initial anteroposterior (AP) and lateral plain radiographs and magnetic resonance imaging (MRI) showed cervical spondylosis with cord compression at C5-6 and C6-7, with concurrent foraminal stenosis compressing the right C6 nerve root. She was seen and treated by an outside surgeon with an anterior cervical diskectomy and instrumented allograft fusion of C5-6 and C6-7. Immediately postoperatively, she had complete resolution of her radiculopathy and axial neck pain. She continued to improve for approximately 6 months’ time, and then over the next year and a half she began having progressively worsening neck pain as well as trapezial and paraspinal muscle spasms. In addition, she developed mild bilateral C7 radiculopathies, which progressively intensified. The patient sustained a minor fall that further exacerbated her neck pain and radicular symptoms. She then presented to our emergency room.
Radiological Findings
Plain radiographs of her cervical spine illustrated a lordotic alignment with anterior instrumentation from C5 to C7 (Fig. 5–1). However, the images revealed a lucency of the C6-7 disk space suggestive of pseudarthrosis. The plate maintained contiguous contact along the anterior cervical spine, with the screws in good position without evidence of loosening. As part of her evaluation, MRI of her cervical spine was obtained. Unfortunately the images were severely degraded by artifact from the instrumentation, and the neural elements could not be visualized. Therefore, the patient underwent computed tomographic (CT) myelography, which illustrated sclerotic bone at the C6-7 level that was consistent with a pseudarthrosis. In addition, the myelogram illustrated severe foraminal stenosis of C6-7 without evidence of spinal cord compression.
Diagnosis
Failed anterior cervical fusion with pseudarthrosis and radiculopathy
 | Background |
To obtain a solid arthrodesis, the optimal environment for the graft and vertebral end plates is required. These components include a well-carpentered graft, adequately prepared end plates, as well as a favorable systemic environment. Maximal surface area along the end plate should be exposed. The end plates should also be well decorticated to establish a well-vascularized area for the fusion to mature. One technique that has been advocated in preparing the fusion bed is to burr the vertebral end plates to actively bleeding bone. However, a biomechanical evaluation compared this technique with perforation of the end plates using a curette. The study demonstrated that the burring technique resulted in a significantly lower tolerance to compressive loads.1 Although excellent graft carpentry and fusion bed preparation are required, other factors such as malnutrition, diabetes, osteoporosis, rheumatoid arthritis, and medications (such as nonsteroidal antiinflammatory agents or corticosteroids) can contribute to poor graft healing and result in an increased risk of nonunion.2–4

Figure 5–1 Lateral radiograph demonstrating C6-7 pseudarthrosis, preserved cervical lordosis, and intact instrumentation.
The selection of the bone grafting material can significantly affect fusion rates. Autograft bone is known to have the highest fusion rates and considered the “gold standard” in spinal surgery. Advantages associated with autograft bone include greater histocompatibility, similarity in bone density between the graft and the fusion bed, elimination of the risk of disease transmission, and a higher fusion rate. However, these advantages must be weighed against the associated morbidity with harvesting autograft, which can be significant, and include chronic pain, nerve injury, and infection.5 The rate of persistent graft site pain has been reported to be as high as 30%.6,7 Many surgeons, therefore, prefer the use of allograft bone despite its disadvantages, which include risk of disease transmission and lower rates of fusion. There has also been interest in additional graft substances and in the osteoinductive abilities of bone morphogenetic proteins (BMPs). Several animal models have demonstrated that BMP-containing allograft or synthetic carrier medium is as effective as or superior to autograft bone in promoting spinal fusion.8 In a series of anterior lumbar fusions, Burkus et al illustrated that allograft cortical bone with rhBMP had equivalent fusion rates compared with autogenous bone graft.9 In addition to allograft, prosthetic implants and cages have also been shown to allow a stable arthrodesis. Biopsies obtained from within radiographically successful intervertebral body fusions with cages have shown that autogenous bone graft was incorporated with viable bone and restoration of hematopoietic bone marrow.10
A significant inhibitor of spinal arthrodesis is tobacco, and this inhibitory influence may affect the physician’s decision to use autograft versus allograft bone. Nicotine is believed to inhibit angiogenesis and neovascularization, thus preventing fusion maturation. This effect may be further intensified by the hypoxia associated with cigarette smoking because smoking is known to decrease vertebral blood supply. These synergistic effects of tobacco products lead to a higher rate of nonunion in smokers. Surgeons should consider the use of autogenous bone graft in this high-risk population.4,11
In the patient presented, her greatest risk factor for the development of a pseudarthrosis was likely her persistent use of tobacco products. In addition, the use of allograft bone likely elevated her risk.4,12 In two-level anterior cervical fusions, allograft fusion rates have been shown to be substantially lower than seen with the use of autograft bone, with a 27% nonunion rate in autograft fusion compared with a 41% nonunion rate in allograft fusion.13 However, the use of anterior cervical plating or instrumentation may offset this difference.4,14–16 Wang et al illustrated a decrease in pseudarthrosis rate from 37 to 18% when supplementing multilevel cervical fusions with an anterior cervical plating system.17 Lastly, the utilization of dynamic anterior cervical instrumentation systems has been shown to further increase the rate of fusion even with multilevel grafting procedures.18
 | Authors’ Preferred Method of Surgical Management |
The patient was taken to the operating room and had a posterior cervical fusion from C5 to C7. This was supplemented with posterior instrumentation using lateral mass screw fixation at C5, C6, and C7 (Fig. 5–2). Concurrent bilateral C6-7 foraminotomies were performed. The patient tolerated the procedure well and was placed in a Philadelphia collar (Ossur Americas, Aliso Viejo, CA) immediately after the procedure.
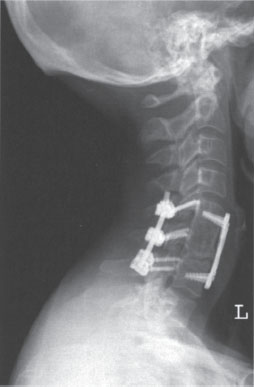
Figure 5–2 Lateral postoperative radiograph demonstrating posterior cervical instrumentation from C5 to C7.



