6 | Failed Dorsal Cervical Fusion |
 | Case Presentation |
History and Physical Examination
The patient is a 41-year-old male with a history of a traumatic C7-T1 fracture-subluxation who underwent instrumented fusion from C5 to T2 for spinal stabilization at another institution. The patient had an uncomplicated recovery but did complain of limited cervical range of motion postoperatively. Despite intensive physical therapy the patient had persistent neck discomfort and was unable to extend his neck. He underwent surgical removal of the instrumentation by his surgeon. His cervical spine, however, remained immobile even after instrumentation removal and he continued to experience neck pain.
On examination, the patient’s head was in a flexed position and active range of motion testing revealed limited cervical extension, flexion, and axial rotation. Motor examination revealed full strength in all extremities. Sensation was intact, there was no hyperreflexia, and there were absent Babinski and Hoffmann reflexes. Gait was normal.
Radiological Findings
Plain films of the cervical spine demonstrated kyphotic angulation centered at C5 of ~25 degrees in magnitude with bone formation anteriorly ventrally from C2 to C7 (Fig. 6–1). Flexion-extension views demonstrated motion, predominantly at the occiput–Cl-2 and C2-3 junction.
Diagnosis
Failed dorsal cervical fusion with kyphosis
 | Background |
Although the patient presented in the clinical vignette had successful arthrodesis following dorsal instrumentation for a traumatic fracture-subluxation, the cervical fusion failed to provide normal cervical curvature; thereby prohibiting neutral positioning of the head and causing constant mechanical neck pain.
Why is achieving a normal cervical lordosis important? Under physiological axial load-bearing conditions, the lordotic cervical spine accepts and distributes force to vital load-sharing structures such as the facets. The alignment of the articulating surfaces of the facet joints approximates a coronal plane orientation and thus, as the neck is extended, the facets abut and participate in load bearing. Lordosis is also a biomechanically superior alignment for the cervical musculature and supporting structures.
Failure to reconstruct cervical lordosis in fusion results in an unfavorable biomechanical environment. Any force can be described by vectors. A force exerted on a lever causes a bending moment. In the spine, a bending moment will occur in relation to the instantaneous axis of rotation (IAR), which acts as the fulcrum.1 The moment arm is the product of the applied force (a vertically oriented vector under axial loading) and the distance of the radius between the IAR and the position at which the force is applied (perpendicular to the applied force).

Figure 6–1 Plain film of the cervical spine demonstrates a kyphotic angulation centered at C5 with bone formation anteriorly from C2 to C7.
Even in a minimally kyphotic cervical spine, the position at which the axial load is applied is in a relative ventral position with relationship to the IAR. This creates a bending moment, thus leading to progressive kyphosis. As the kyphotic deformity progresses, the moment arm increases, as does the bending moment. In this manner, with repetitive axial load bearing, the curvature becomes less favorable and more unstable in a self-propagating, vicious cycle.1 Additionally, the facet joints are slightly distracted in the presence of kyphotic alignment. By not having contact with one another, the facets cannot contribute to axial load bearing and cannot “resist” the progression of kyphosis. As the degree of kyphosis steepens, the associated symptoms, including pain and myelopathy, can worsen. Kyphosis also leads to an accelerated degeneration of adjacent intervertebral disks. Thus kyphotic alignment must be avoided in cervical spine fusion, and if reasonable and possible, should be corrected if already present.
 | Authors’ Preferred Method of Surgical Management |
In view of the posture-related symptoms, the patient was offered surgery for correction of the kyphotic deformity. The operation was performed in two phases. The first phase involved a dorsal approach to release the spine to facilitate deformity correction. The second phase involved restoration of normal cervical curvature, interbody fusion, and instrumentation.
The patient was placed into a Mayfield three-pin head holder fixation. He was positioned prone on thoracic rolls and attached with the Mayfield frame (Integra, Plainsboro, NJ) to the operating room table. After making a midline incision, subperiosteal dissection was carried down the spinous processes and laterally to expose the laminae bilaterally from C7 to C3. A large amount of fusion mass was encountered extending laterally and involving the facets. A high-speed drill was used to make a trough just medial to the facets bilaterally along the laminae of C4, C5, and C6. These laminae were then removed en bloc utilizing a 1-mm Kerrison punch. The bone was cleaned and saved for later use as autograft. Facetectomies were performed at the C3-4, C4-5, C5-6, and C6-7 levels bilaterally using a high-speed drill and 1- and 2-mm Kerrison punches (Fig. 6–2). Autograft bone was then placed into the facetectomy defects.
The patient was then turned supine on a second operating table with the head on a donut pillow. A high thoracic roll was employed to place the patient in a slight amount of neck extension. An attempt at distraction revealed the cervical spine to be quite immobile. A standard ventral cervical approach along the sternocleidomastoid muscle was used to access the ventral elements of the spine. Large osteophytes were noted on either side of the vertebral bodies; these were taken down with a high-speed cutting burr to gain access to the intervertebral disks.
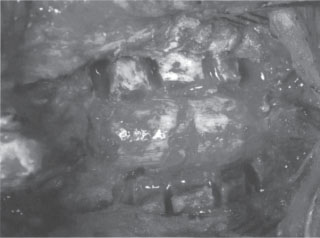
Figure 6–2 Intraoperative image of facetectomies performed at the C3-4, C4-5, C5-6, and C6-7 levels bilaterally with full exposure of the nerve roots.
Distraction posts were introduced into the bodies of C3, C4, C5, C6, and C7. Anterior diskectomy was then performed at C3-4, C4-5, C5-6, and C6-7. Care was taken to preserve the posterior longitudinal ligament (PLL) at every level. Trapezoid-shaped allograft wedges were then fashioned from a single piece of fibula to fit each disk space. The grafts ranged in size from 6 to 8 mm. A DOC dynamic ventral cervical plate system (DePuy-Acromed, Raynham, MA) was then contoured to the desired curvature. Cervical lordosis was then achieved using simultaneous manual distraction, vertebral body distraction posts, and screw tightening at intermediate points of fixation on the contoured implant (1,2,3). Self-tapping screws were used for fixation. The dynamic sliding bars were set to enable several millimeters of settling.
Pearls and Pitfalls
Cervical spine kyphosis can be addressed by a ventral, dorsal, or combined approach. Given the history of prior fusion in this patient, a dorsal osteotomy to release the spine was required prior to ventral instrumentation. Intraoperative inspection revealed the fusion to be involving the facets, so the releasing laminectomies were extended laterally to complete foraminotomies/facetectomies at C3-4, C4-5, C5-6, and C6-7. This allowed for relaxation of the dorsal elements involved in the bony fusion to decrease resistance to distraction. In addition, wide dorsal osteotomy allowed full exposure of the nerve roots at those levels. This prevented neural element tethering or compression that could result in injury during spinal manipulation for deformity correction.
A ventral approach was then undertaken to release the fused ventral spine, to remove reactive osteophytes, and to perform diskectomies at multiple levels. In the absence of spondylolisthesis and disk fragments compressing the spinal cord, we advocate leaving the PLL intact. The PLL adds stability to the spine as a supporting structure. In addition, during deformity correction, the PLL acts as a fulcrum about which lordosis can be achieved. After the diskectomies, a large Cobb instrument was inserted into each disk space and gentle distraction was performed. This maneuver released the spine ventrally and facilitated extension.
When positioning the patient for the ventral approach, the use of a high thoracic roll to elevate the scapulae off the operating table is of importance. By raising the scapulae in relation to the occiput, the strong force of gravity can be employed safely and effectively to aid in deformity correction via extending the cervical spine.1 Actual extension should not be applied until after ventral decompression via diskectomy or corpectomy is performed. A donut or pillow beneath the head can be removed at that point, thus facilitating the aforementioned extension (Fig. 6–3).
Distraction posts that are placed in a convergent manner (with screw insertion at an angle perpendicular to the vertebral body surface) can deliver the greatest amount of distraction by straightening the posts so that they are in parallel alignment. Once satisfactory alignment is achieved with the use of distraction posts and manual traction, the preparatory steps for fusing the patient in a more biomechanically advantageous curvature can be undertaken. Wedge-shaped pieces of bone autograft are designed to fit the interbody space in the newly aligned position. The interbody struts serve several functions, including providing adequate interbody distraction to maintain the lordosis, and serving as both the substrate and material for arthrodesis.

Figure 6–3 (A) Placement of a high thoracic role and a donut pillow underneath the head with the patient in prone position maintains the neck in neutral or slightly extended position. (B) Removal of the donut results in further extension of the neck under the force of gravity.
(From Benzel EC Deformity prevention and correction: complex clinical strategies. In: Biomechanics of Spine Stabilization. New York: Thieme; 2001:390. Reprinted with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


